PMC/PubMed Indexed Articles
Indexed In
- Academic Journals Database
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Scimago
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- MIAR
- University Grants Commission
- Geneva Foundation for Medical Education and Research
- Euro Pub
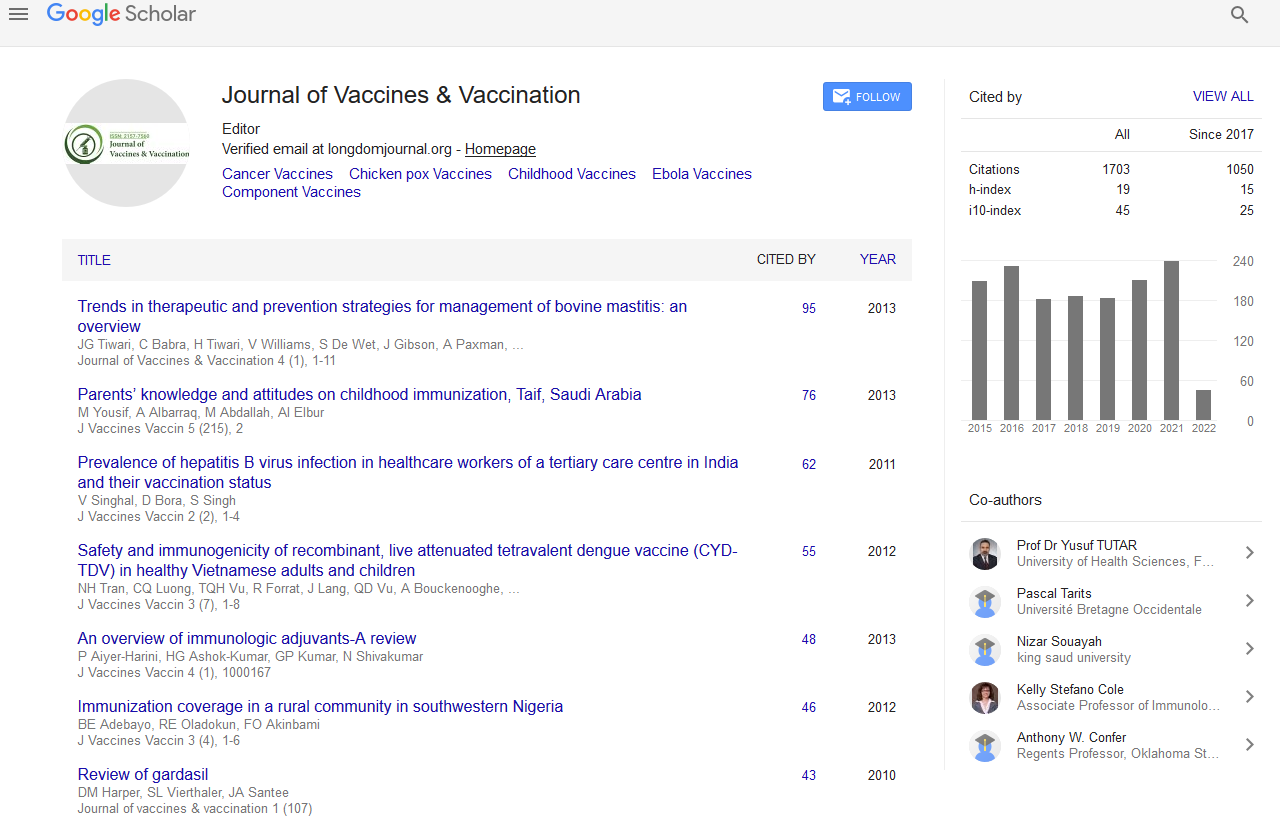
- Google Scholar
Useful Links
Share This Page
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Topical treatment or vaccines: Health economic evaluation of treatments for cutaneous Leishmaniasis ulcers in Afghanistan
7th Middle East - Global Summit and Expo on Vaccines & Vaccination
September 28-29, 2015 Dubai, UAE
Hans-Christian Stahl and Andrew Farlow
Universität Heidelberg, Germany
Scientific Tracks Abstracts: J Vaccines Vaccin
Abstract:
Background: Despite recent advances in topical treatments of chronic cutaneous Leishmaniasis ulcers, future treatment options that reduce the burden of the disease for the population at risk in terms of infection probability and for the patients in terms of avoided life-long and disfiguring scars are investigated herein. A cutaneous Leishmaniasis vaccine could control the spread of the parasite in humans and animals and thereby eliminate the disease. Based on most recent published clinical results of costeffective wound debridement and moist wound care in chronic cutaneous Leishmaniasis ulcers, we investigate the comparative cost-effectiveness of vaccines in the context of a neglected disease such as cutaneous Leishmaniasis. Methods: A decision analytical model based on pre-defined health states was used to analyze the comparative cost-effectiveness of two wound care regimens versus intra-dermal Sodium Stibogluconate investigated within a randomized controlled clinical trial in cutaneous Leishmaniasis patients in Afghanistan. Costs were collected from a societal perspective. Effectiveness was measured in wound-free days. The decision tree was calibrated e.g., baseline parameters, sensitivity ranges and parameter distributions on the basis of the patient-level data collected during the trial. The results are then compared to vaccine costs and effectiveness calculations taken from the literature. Final outcomes were the efficiency of the regimens and a budget impact analysis in the context of Afghanistan. Results: Average baseline costs per patients were 11 US$ for intra-dermal antimony (Group-1), 16 US$ for wound debridement and subsequent moist wound care (Group-2) and 25 US$ for moist wound care alone (Group-3) in patients with a single chronic CL ulcer elicited by L. tropica or L. major.The incremental societal budget impact analysis estimated additional costs of 0.765 Million US$ and 2.3 Million US$ in 2013 US$ prices for Group-2 and Group-3 regimens compared to Group-1 respectively. The budget impact of the DAC N-055 basic crème preparation in Group-2 and 3 would save 0.353 million US$ in regimen 2 and 0.036 million US$ in regimen 3 compare to the intralesional sodium Stibogluconate WHO EMRO IL SSG case management protocol. The incremental baseline cost-effectiveness ratio of Group-2 versus Group-1 was 0.09 US$ and Group-3 versus Group-1 0.77 US$ and very cost-effective according to WHO CHOICE criteria. Within a Monte-Carlo probabilistic sensitivity analysis Group-2 was cost-effective in 80% of the cases starting at a willingness-to-pay of 80 cents per wound free day. Conclusion: Group-2 is the most cost-effective treatment alternative compared to Group-1. The comparative cost-effectiveness of Group-3 depends on the re-ulceration rate and the number of dressings necessary to avoid super-infections. A future multicentre implementation research study to account for subgroup analysis and for the heterogeneity of patients should supplement the results obtained in Group-3.
Biography :
Email: hcstahl@gmail.com