Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- Directory of Abstract Indexing for Journals
- OCLC- WorldCat
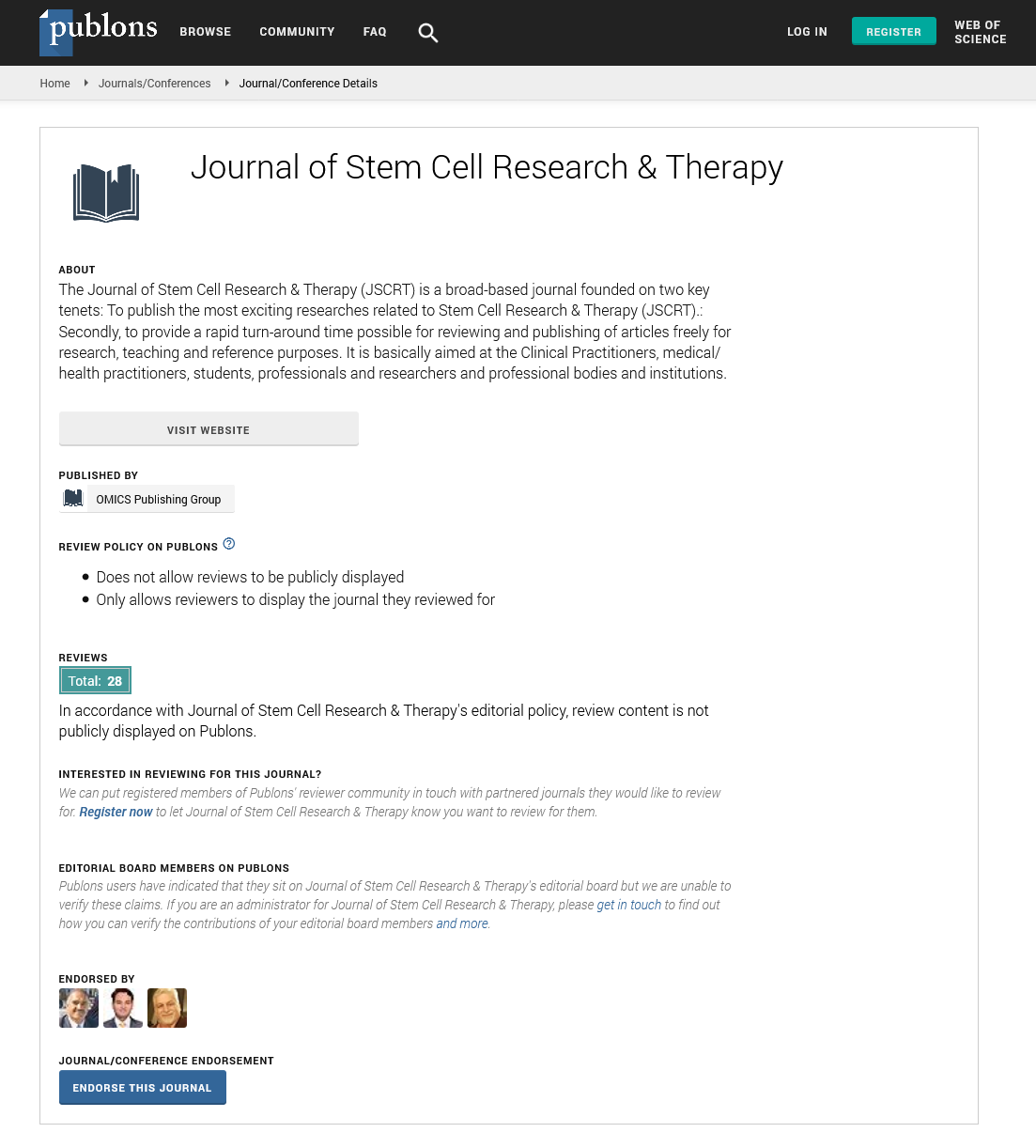
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Progress in AAV-based gene therapy for cardiovascular diseases: Towards improved outcomes and higher quality of life
4th International Conference and Exhibition on Cell & Gene Therapy
August 10-12, 2015 London, UK
Paul L Hermonat
Keynote: J Stem Cell Res Ther
Abstract:
Adeno-associated virus (AAV) is a vector which is highly appropriate for the field of cardiovascular gene therapy, being very
long-lived and is weakly recognized by the immune system compared to adenovirus vectors (Ad). We have made progress
in the last few years in AAV-based gene therapy against cardiovascular disease (eg. atherosclerosis), both in the selection of
therapeutic genes and in the selection of transcriptional promoters to express those genes. For example, transforming growth
factor beta 1 (TGFβ1) is known to be a powerful gene in regulating immune response and TGFβ1 gene delivery inhibits
atherosclerosis. Yet TGFβ1, a secreted protein, is very pleomorphic in its phenotypes and can give strong systemic adverse
reactions (eg. fibrosis, increased infections). In an attempt to identify an intracellular substitute protein from one of TGFβ1’s
signal transduction pathways, we chose to study human (h) SMAD3. AAV2/8-hSMAD3 gene delivery was compared to AAV/
Neo (control), both being tail vein injected into the low density lipoprotein receptor knockout (LDLR-KO) mice, and then
placed on a high-cholesterol diet (HCD). After 20 weeks on HCD the AAV/hSMAD3 delivery resulted in significantly lower
atherosclerosis (versus Neo control) as shown by larger aortic cross sectional lumen area, thinner aortic wall thickness, and
lower aortic systolic blood velocity. HSMAD3 delivery also pushed aortas into a Th2 response, but without increased fibrosis.
Thus SMAD3 represents a new type of efficacious therapeutic gene, with higher safety than its related, stimulatory chemokine
“parent” TGFβ1. Additionally, we’ve tried to improve therapeutic gene delivery and expression. To do this we observed the
disease-responsive lectin-like oxidized low density lipoprotein receptor 1 transcriptional promoter (LOX1pr) for its ability to
express the therapeutic interleukin 10 (IL10) genes within an AAV vector. Like TGFβ1, IL10, is known to give adverse reactions
such as increased infections and cancer. Thus an AAV/LOX1pr-hIL10 vector was compared to a similar vector using the
strong constitutive CMVpr for efficacy in the LDLR KO-HCD model. Both the AAV/LOX1pr-hIL10 and AAV/CMVpr-hIL10
gene deliveries were found to give statistically equal efficacy in their down-regulation of atherosclerosis (aortic systolic blood
velocity, aortic cross sectional area, and aortic wall thickness). However, overall IL10 transgene expression was much lower
when the LOX1pr was used versus the CMVpr. These data suggest that the use of a disease-specific promoter, such as LOX1pr,
is highly appropriate for giving therapeutic efficacy, yet also giving a built-in safeguard against adverse reactions due by also
giving overall lower transgene expression than the CMVpr. Finally, an overview will be given as to what I believe AAV-based
cardiovascular gene therapy can be expected to do in the future of health care and the field of cardiology.
Biography :
Paul L Hermonat completed his PhD at the University of Florida in 1984, and Postdoctoral studies at the National Institutes of Health. He is Research Career Scientist
at the Central Arkansas Veterans Healthcare System, and a Professor of Internal Medicine and OB/GYN at the University of Arkansas for Medical Sciences. He mapped
mutationally AAVs genes, determined their functions, was the first to generate recombinant adeno-associated virus (AAV/NeoR) and to transfer genes into cells via this
method and has 150 manuscripts published. From his first study on AAV-based gene therapy in 1984 there are now over 2,600 papers on the topic. He now continues studies
on AAV genetics and helper genes, and on gene therapy for cardiovascular disease and cancer..