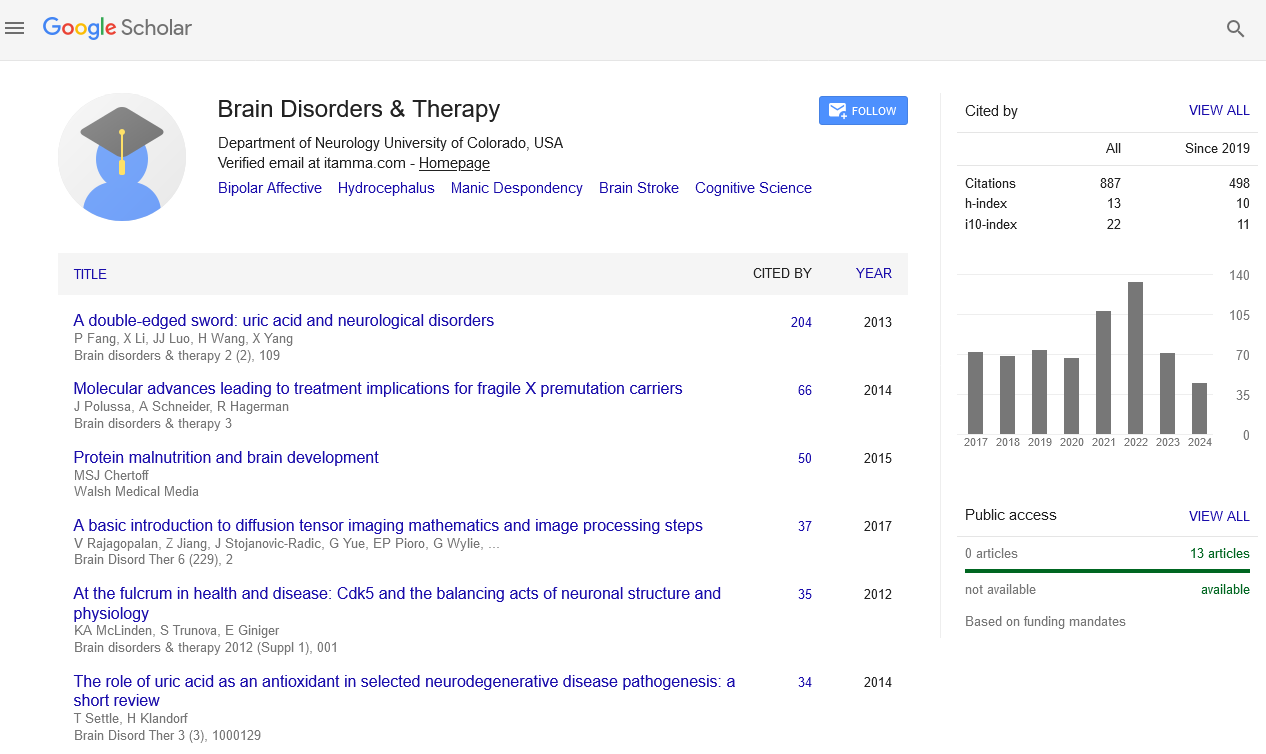
Indexed In
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Novel strategies for stroke therapy based on targeting of mitochondrial dysfunction and ER stress signaling pathways
Global Summit on Stroke
August 03-05, 2015 Birmingham, UK
Howard Prentice
Keynote: Brain Disord Ther
Abstract:
There is a major need for new stroke therapies, and current treatments involving tissue plasminogen activator (tPA) are dependent
upon administration within small time-window after stroke onset. We have employed the neuroprotective agents taurine and
S-Methyl-N, N-diethylthiocarbamate (DETC-MeSO) either individually, or as part of particular combination therapies, to elicit
neuroprotection in a transient focal ischemia rat stroke model. Individually, taurine can protect neurons against ischemia through
preventing calcium overload and through inhibiting pro-apoptotic processes. In our studies on endoplasmic reticulum (ER) stress
pathways, we have demonstrated that taurine elicits neuroprotection by inhibiting two ER stress pathways, namely ATF6 and
IRE-1 pathways, without altering the contribution of the PERK pathway. DETC-MeSO, the active metabolite of disulfiram, is
a partial antagonist of glutamate receptors and was previously shown to be effective in reducing seizures. In our stroke model,
DETC-MeSO administered individually, protected through inhibiting ER stress markers including p-PERK, p-eIF2-alpha, XBP-1
and CHOP. Using a multi-drug combination consisting of DETC-MeSO and the stem cell mobilizing agent granulocyte colony
stimulating factor (G-CSF), in addition to the preconditioning agent sulindac, we found that infarct size was markedly decreased
in the stroke model relative to sham controls. With administration of these agents prior to reperfusion, multidrug treatment was
found, at 4 days after the ischemic episode, to elicit decreases in GRP78, eIF-2-alpha and IRE-1, both in core and penumbra. The
multi-drug combination was highly effective at decreasing infarct size, either under conditions of prior administration, or with
administration of the drug combination 24 hours after reperfusion. Our novel therapeutic agents were found to decrease infarct
size, to elicit protection through decreasing levels of pro-apoptotic components and furthermore to differentially target specific
ER stress pathways.
Biography :
Howard Prentice obtained his Ph.D. from the University of London, UK and after post-doctoral training in the USA he held faculty position at the University of Glasgow, UK
from 1993-2000. He then joined Florida Atlantic University in Boca Raton where he is currently Associate Professor of Biomedical Sciences in the College of Medicine.
From 2013-2014 he was visiting Associate Professor at Harvard Medical School, Boston. He has more than 60 peer reviewed publications. He has been serving on study
sections for the American Heart Association and the NIH and on editorial boards of several international scientific journals.