PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- ResearchBible
- China National Knowledge Infrastructure (CNKI)
- Scimago
- Ulrich's Periodicals Directory
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- MIAR
- Scientific Indexing Services (SIS)
- Euro Pub
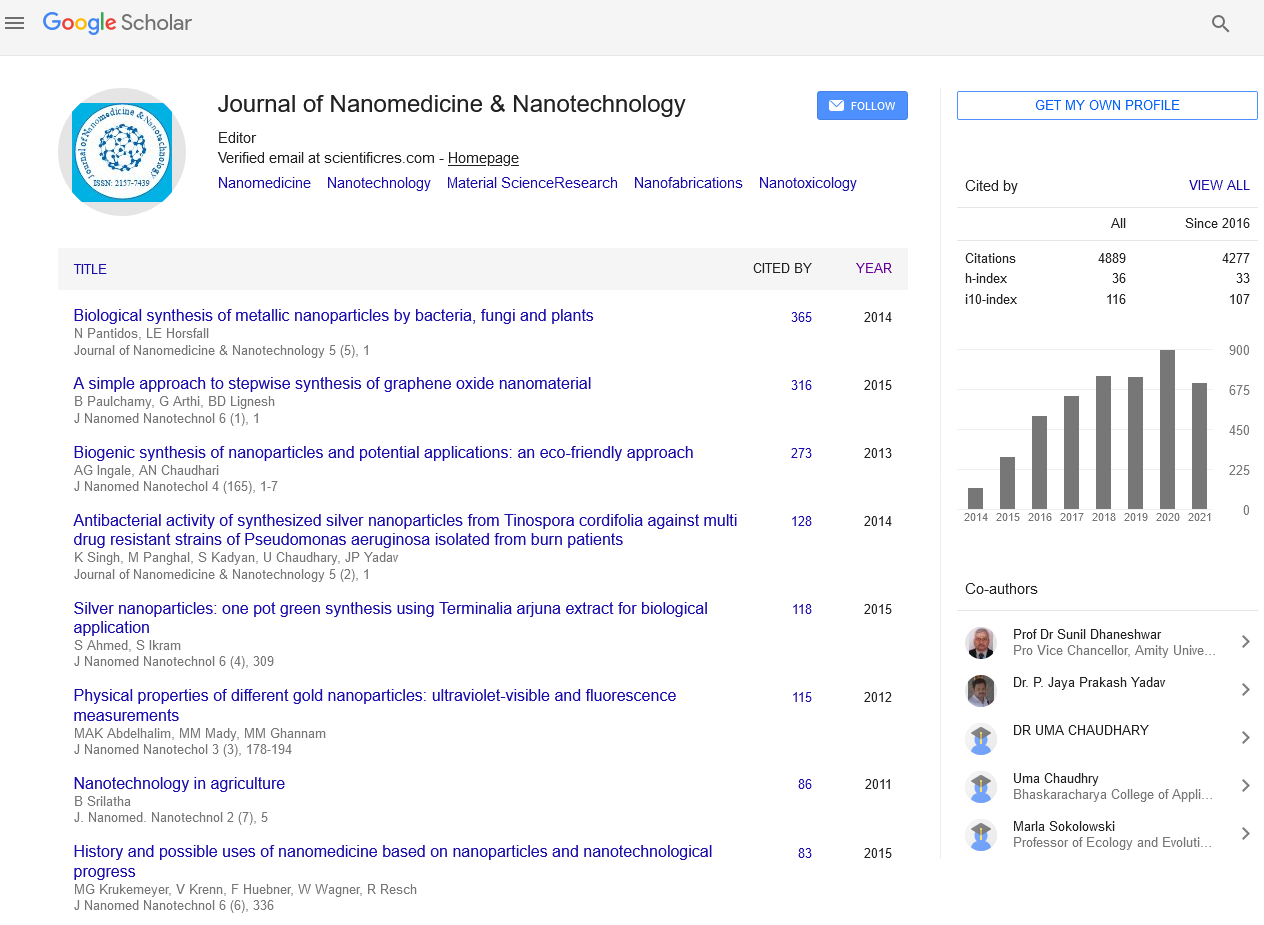
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Nanodelivery of a multimodal drug cerebrolysin reduces brain pathology following amyloid beta peptide infusion induced Alzheimerâs disease
Nanotechnology Congress & Expo
August 11-13, 2015 Frankfurt, Germany
Hari S Sharma
Keynote: J Nanomed Nanotechnol
Abstract:
Alzheimer?s Disease (AD) induced brain pathology is instrumental in causing functional and behavioral disturbances in patients. Research reports in AD suggest deposition of amyloid-?-peptide (ABP) within the brain could be instrumental in precipitating the pathophysiology of AD. Chronic intracerebroventricular infusion of ABP in rats thus results in AD like symptoms in rat model. To reduce the toxic effects of ABP and to enhance neurorepair we used a multimodal drug Cerebrolsyin (Ever NeuroPharma) that is a balanced composition of various neurotrophic factors and active peptide fragments in our AD model. Infusion of ABP (1-40) intraventricularly (i.c.v.) in the left lateral ventricle 250 ng/10 ?l once daily for 4 weeks resulted in ABP deposits in cortex and in hippocampus and associated with an increased glial fibrillary acidic protein (GFAP) immunoreactivity, loss of myelin basic protein (MBP) and leakage of albumin in these brain areas. Nissl stain showed marked neuronal loss or distortion in areas showing ABP deposition. The behavioral disturbances on Rota Rod performances and inclined plane angle tests showed significant deterioration along with the ability to retrieve platform in water maze tests in ABP infused rats. Infusion of Cerebrolysin (25 ?l, i.c.v.) starting from 1 week after the onset (but not 2 weeks) of ABP infusion daily and terminated 1 week before ABP last infusion, significantly reduced brain pathology improved the behavioral functions. Interestingly, TiO2-naonowired Cerebrolsyin administration 2 weeks after ABP infusion daily for 1 week only resulted in marked neuroprotection and significantly improved behavioral functions. Our observations clearly suggest that (i) Cerebrolsyin administration if given during a critical therapeutic time window is able to attenuate AD pathology, and (ii) nanodelivery of cerebrolysin has superior effects and extended therapeutic window in AD. The possible mechanisms and functional significance of our findings will be discussed.
Biography :
Hari S Sharma, (Swedish Citizen) is the Director of Int. Expt. CNS Injury & Repair (IECNSIR); Professor of Neurobiology (MRC); Docent in Neuroanatomy (UU) is currently working in Uppsala University Hospital, Department of Surgical Sciences, Division of Anesthesiology & Intensive Care Medicine, Uppsala University, Sweden. He obtained his PhD in Neuroscience in 1982 from Banaras Hindu University, Varanasi, India and Dr. Med. Sci from Uppsala University in 1999. He has published over 300 peer reviewed research articles (ISI database h-index 36) related to neuroprotection and neuroregeneration in relation to the blood-brain barrier in stress, trauma, and drugs of abuse in health and disease. His research on brain pathology and neuroprotection in different model is supported by Laerdal Foundation of Acute Medicine, Stavanger, Norway; role of nanoparticles in neurodegeneration and neuroprotection for treatment strategies from European Aerospace Research & Development (EOARD), London, UK and US Air Force Research Laboratory, Wright Patterson Air Force Base, Dayton, Oh, USA; drug abuse research and neuroprotection from National Institute on Drug Abuse (NIDA); National Institute of Health (NIH).