Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- Directory of Abstract Indexing for Journals
- OCLC- WorldCat
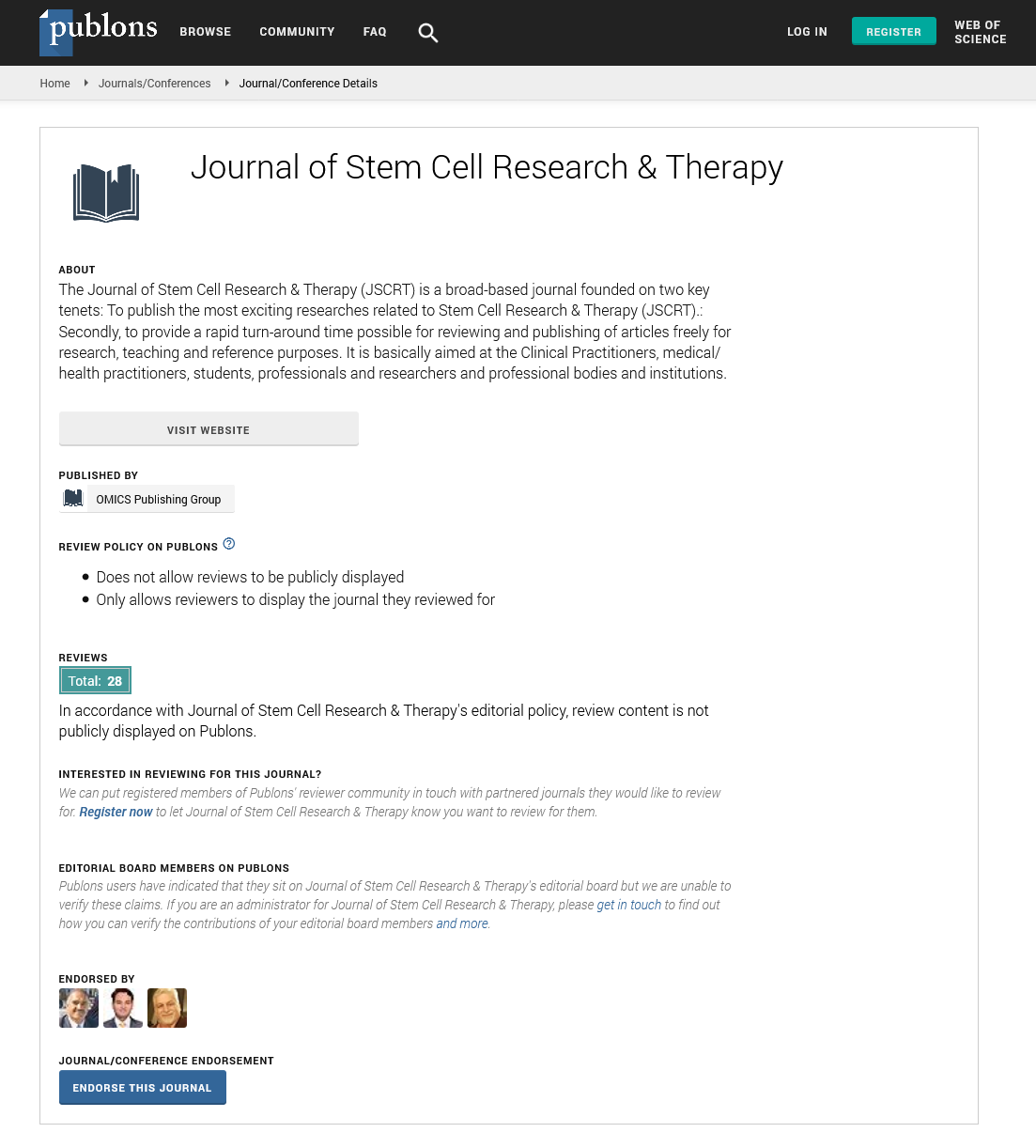
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Micro-fragmented adipose tissue as a disease targeting stem cell-based therapeutic with drug delivery potential in orthopaedic medicine
17th World Congress on Tissue Engineering, Regenerative Medicine and Stem Cell Research & 10th Global Conference on Physiotherapy, Physical Rehabilitation and Sports Medicine
October 28, 2022 | Webinar
Mark Slevin
Manchester Metropolitan University, United Kingdom
Scientific Tracks Abstracts: J Stem Cell Res Ther
Abstract:
Statement of the Problem: Current options for treatment of osteoarthritis (OA) are limited, with advanced grades normally requiring invasive surgical joint replacement or athroplasty. Given the increasingly young age of patients undergoing athroplasty, new technologies are urgently required to stabilise and slow down the progression of OA, in these individuals (aged <65). This will delay the need for surgical intervention due to the prosthetics limited lifespan, particularly in active individuals, and the inevitable later necessity for revision which is accompanied by an increase in surgical complications and shorter life expectancy of the second or third prosthetic. Purpose: The purpose of this study is to characterise and delineate the potential of a biological material - microfragmented adipose tissue (MFAT) for its usability, capacity to block the progression of moderate to severe OA and, it’s possible drug targeting capacity, with the ultimate aim of delaying the necessity for athroplasty in younger patients. Methodology and Theoretical Orientation: Information will be provided detailing MFAT preparation, characterization of its active components and mechanisms of action, stratifying super responders and non-responders to treatment, storage capacity for multiple use and drug uptake and release for pharmacologically enhanced targeted treatments. Findings: Highly anti-inflammatory long-term (months) surviving MFAT micro-clusters or grafts can be delivered by ultrasound-guided injection to OA sites of joint damage where paracrine activity and release of facors including interleukin-1 receptor alpha antagonist provided significant improved mobility and pain reduction over two years in patients deemed suitable for knee athroplasty. MFAT could be cryopreserved without loss of viability whilst, absorbtion of chemotherapeutic drugs by MFAT was sufficient to inhibit tumour growth for several months in experimental models. Conclusion and Significance: Algorithmically defined stratified use of MFAT or drug-loaded MFAT may provide medium-longterm control of symptomatic OA postponing the need for athroplasty.
Biography :
Mark Slevin is a Director of the Centre for Biomedicine from 2016-2018 and was Manchester Met lead on dementia research-linked with the greater Manchester dementia consortium. UOA3 university committee member and university committee for research and knowledge exchange. He was returned as number 1 ranked in UOA3 in 2002, 2008 and 2014 REF/RAE returns for Manchester Metropolitan University. He has full Professorial titles at the Universities of Targu Mures (Romania) and Griffith University, Brisbane (Australia). He is also visiting Chair in Clinical Biomedicine at the ICCC-CSIC, St Pau Hospital Barcelona and Adjunct Professor at both Almajmaah and Ha’il Universities in Saudi Arabia. He is also a Fellow of the Royal College of Pathologists and has been since 2008. He is also a consultant for Smith and Nephew pharmaceuticals (2012-1017) and LIPOGEMS incorporated (2017). He currently is scientific director of the Centre for Advanced Medical and pharmaceutical Research in UMFST, Targu Mures, Romania.