PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
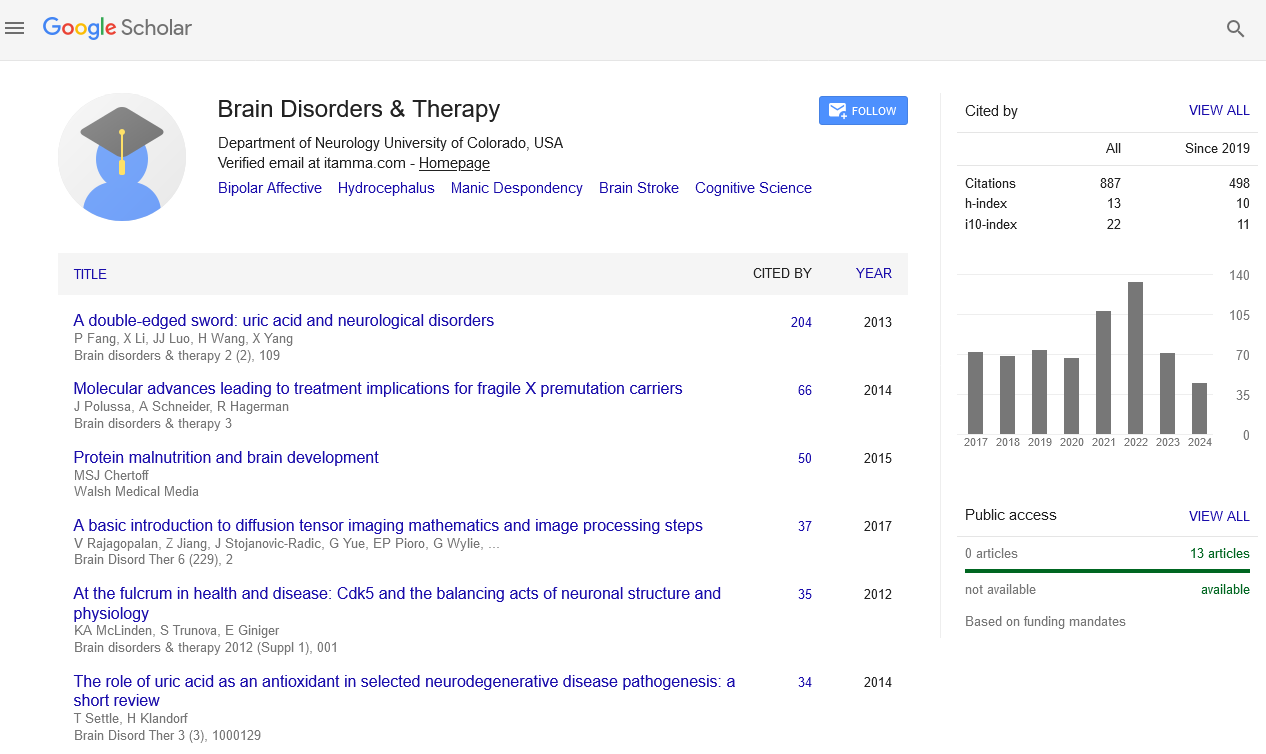
- Publons
- Geneva Foundation for Medical Education and Research
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Increased Blood brain barrier permeability in a transgenic model of Huntingtonâ??s disease and Motor neuron disease favors increased brain uptake of the complement C5a receptor antagonist PMX205
International Conference on Brain Disorders & Therapeutics
August 24-26, 2015 London, UK
Vinod Kumar
University of Queensland, Brisbane, Australia
Posters-Accepted Abstracts: Brain Disord Ther
Abstract:
Complement system activation in neurodegenerative diseases such as Huntington�??s disease (HD) and motor neuron disease (MND) promotes the pathology of neurological conditions, in co-ordination with increased permeability of the blood brain barrier (BBB). We have previously shown that the C5a receptor antagonist, PMX205, reduces brain inflammation and neuronal death in neurodegenerative disease models. The present study investigated the extent and stages of BBB integrity alteration during the progression of neurodegeneration in a model of HD and MND. In addition we examined whether increased BBB permeability, allowed for increased PMX205 entry into the degenerating brain. Transgenic R/61 mice harbouring the human mutant huntingtin gene, transgenic SOD1 mice and age/litter matched control mice at various ages were injected i.v. with sodium fluorescein (Na-FL) to examine BBB permeability. Blood and tissue samples including brain regions (cerebellum, cortex, striatum) and spinal cord were collected after 15 min. Samples were processed for fluorescence determination using a validated quantitative method, and results were expressed as level of Na-FL (ng/g) and % fluorescence uptake. Pharmacokinetic studies were performed by administering PMX205 1 mg/kg i.v., and collecting blood and perfused brain and spinal cord samples after 2.5min. Samples were processed and analysed for PMX205 levels by a validated method using LC-MS/MS. We identified increased BBB permeability in transgenic mice, compared to wild-type littermates. BBB permeability changes occurred early in disease, and increased as neurodegeneration progressed. In line with this, we identified significant changes in PMX205 brain levels, Na-FL levels and fluorescence uptake. In conclusion, these studies demonstrate breakdown of the BBB and blood-spinal cord barrier (BSCB) occurs in the early stages of neurodegeneration in these mouse models. This increased permeability would likely favors effective transport of drugs into degenerating regions of the brain/spinal cord. In this study, we demonstrate increased PMX205 entry, which may assist in the neuroprotective effects of this drug in these neurodegenerative models.
Biography :
Email: v.kumar1@uq.edu.au