Indexed In
- Open J Gate
- Genamics JournalSeek
- SafetyLit
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
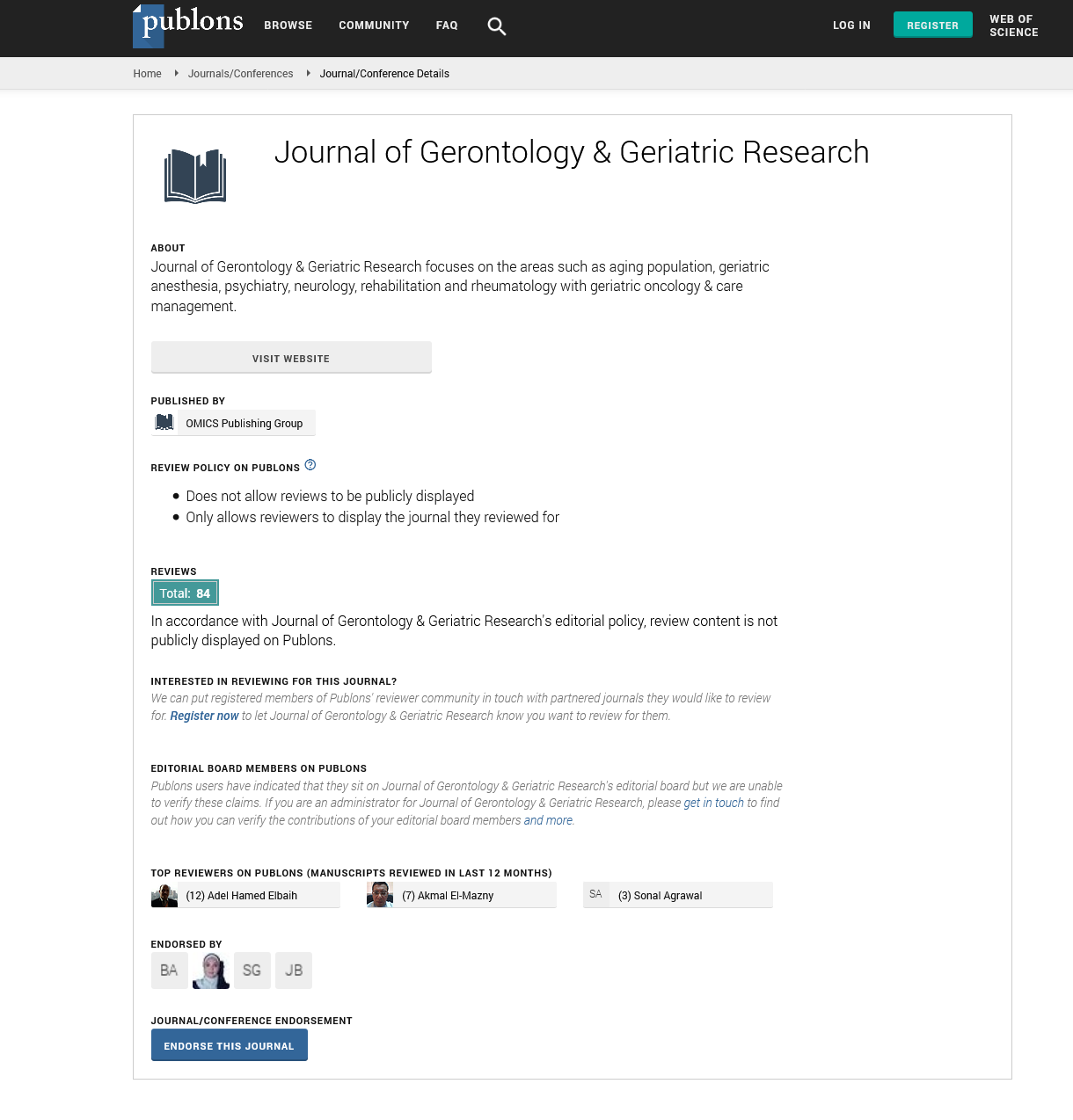
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
DNACPR: CAN THE GO-FAR SCORE IMPROVE DECISION-MAKING?
2nd International Conference on Aging & Gerontology
June 26-27, 2017 San Diego, CA, USA
Georgina Hicks & Thomas Pepper
Chelsea and Westminster Hospital, UK
Scientific Tracks Abstracts: J Gerontol Geriatr Res
Abstract:
Statement of the Problem: Do Not Attempt CPR (DNACPR) decisions are commonly made in UK hospitals. Recent legislation dictates that the decision be discussed with the patient or their relatives. Many patients and relatives have unrealistic expectations of CPR outcome and it is essential that this is addressed in such conversations. We undertook two investigations of the appropriateness of resuscitation decisions based on a validated tool for predicting neurologically intact survival after in-patient CPR (Good Outcome Following Attempted Resuscitation, GO-FAR score). Methodology: All patient records from a geriatric ward were reviewed on a single day. Information was collected regarding patient age, comorbidities and DNACPR decisions, and a GO-FAR score calculated. The process was repeated on a second day two months after reporting our initial findings to clinical staff. Findings: 48 patients with a mean age of 73 years (SDļ?±13) were included. Of the 25 patients in the initial study, 5/9 patients with a 9.4% likelihood of neurologically intact survival were DNACPR, 9/12 with a 1.7% likelihood were DNACPR, and 1/4 with a 0.9% likelihood was DNACPR. Of the 23 patients in the subsequent study, 1/9 patients with a 9.4% likelihood of neurologically intact survival was DNACPR, 3/11 with a 1.7% likelihood were DNACPR, and 2/3 with a 0.9% likelihood were DNACPR. Conclusion & Significance: Following introduction of the GO-FAR score, a smaller proportion of patients with 9.4% and 1.7% likelihood of neurologically intact survival were made DNACPR (p=0.13 and 0.04 respectively), and a greater proportion of patients with 0.9% likelihood were made DNACPR (p=0.49). Introduction of the GO-FAR score influenced the practice of clinicians with varying significance. The scoreā??s greatest utility may be in prompting consideration of resuscitation status for patients with <1% likelihood of neurologically intact survival, and facilitating an evidence-based discussion with the patient and their relatives.
Biography :
Georgina Hicks has undertaken her Post-graduate Medical degree at King’s College London. Following graduation, she has worked as Foundation Doctor in London, gaining broad experience in geriatric wards specializing in heart failure and stroke, as well as other specialties.
Email: tom.pepper@outlook.com