Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- Directory of Abstract Indexing for Journals
- OCLC- WorldCat
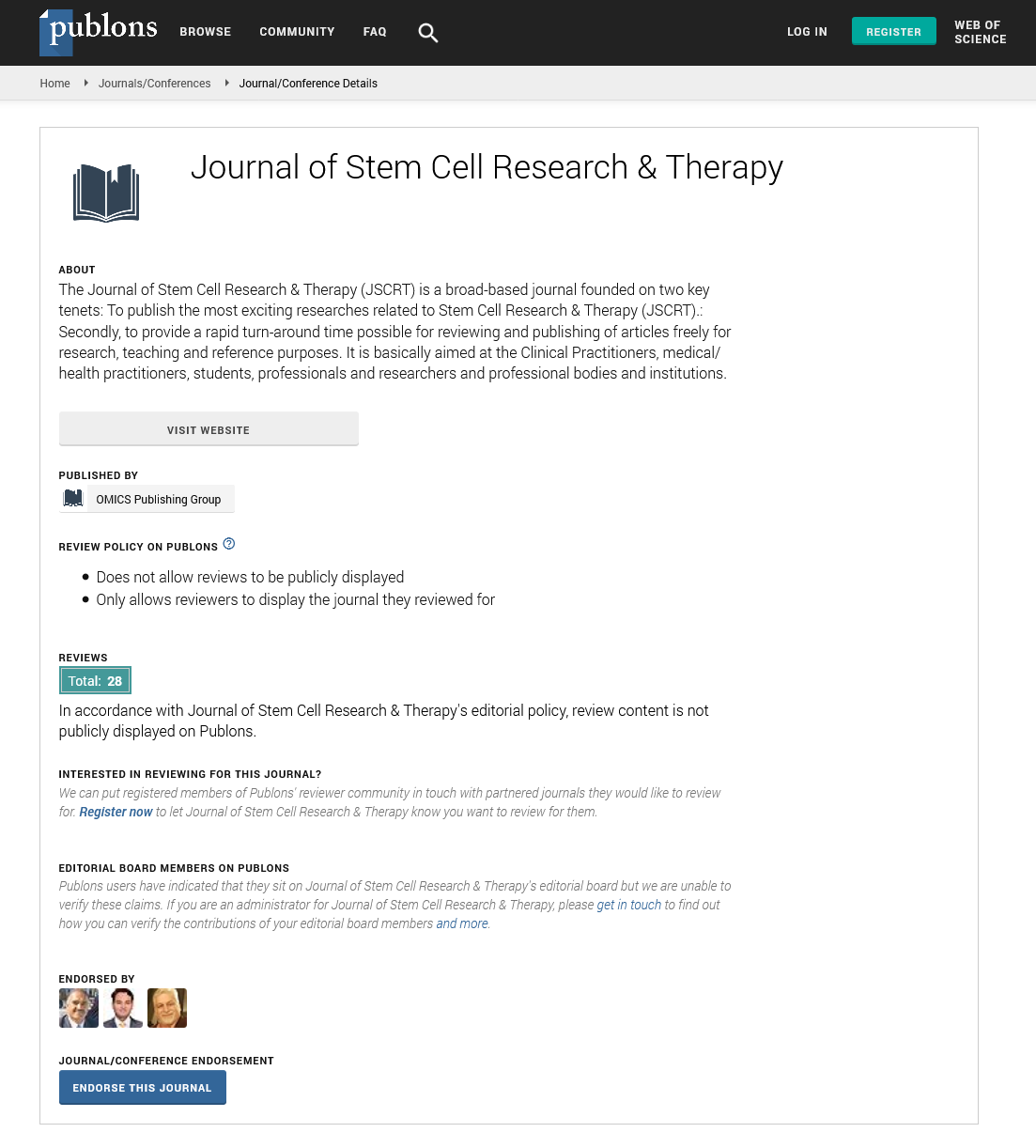
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Collagen coating for tissue engineered diaphragm in rats
11th Annual Conference on Stem Cell and Regenerative Medicine
October 15-16, 2018 Helsinki, Finland
Elena V Kuevda, Elena A Gubareva, Timofei E Grigoriev, Dmitry P Puzanov, Sergey V Krasheninnikov, Ksenia I Lukanina, Christina Likhacheva,Alexander L Vasiliev and Sergei N Chvalun
Kuban State Medical University, Russia
Kurchatov Institute, Russia
Posters & Accepted Abstracts: J Stem Cell Res Ther
Abstract:
Congenital diaphragmatic hernia and other malformations play an important role in the increased mortality rate both in children and adults. Regenerative medicine methods are promising sources for the anatomical patch repair. Diaphragmatic repair could be implemented with the tissue engineered constructions contained collagen coated decellularized biological scaffolds and autologous cells. In our study we focused on obtainment and characterization of rat diaphragm scaffolds coated with 0.1% (group 1), 0.5% (group 2), 1% (group 3) collagen and seeded with rat bone Marrow-derived Stem Cells (MSCs). Decellularized rat diaphragm scaffold reseeded without additional coating was used as a control. Acellular diaphragm matrices were obtained after detergent-enzymatic decellularization with 4% sodium deoxycholate with EDTA and bovine pancreatic DNAse I according to our previously modified protocol. Lyophilization was carried out in lyophilic drying Martin Christ ALPHA 2-4LSC. Samples filled up with water were frozen in liquid nitrogen and then lyophilized for 3 days at 20 �C. Grafts biocompatibility was tested with XTT test and Alamar blue assay after 48 hours of incubation under standard conditions. Cell viability and scaffold cytotoxicity indices were calculated in percentage. Cell viability indices for the tested groups were 33.33%; 33.32%; 33.32%; 33.40%, respectively. Cytotoxicity indices were 8.41%; 8.37%; 8.50%, respectively. Cell viability and cytotoxicity indices for the control group were 0.05% and 24.93%, respectively. Histological staining revealed no significant differences between the tested groups cells were spread on the surface of the samples. The control ones had a few cells on the exteriority. Thus, the process of collagen coating significantly improves cell adhesion and proliferation on the scaffold and is a promising strategy for the creation of the tissue engineered constructions. The quantity of collagen used for the coating did not affect the scaffold biocompatibility and cell proliferation.
Biography :
Elena V Kuevda has her expertise in Regenerative Medicine and Tissue Engineering. She has completed her MD and the PhD from Kuban State Medical University. She is currently working as Researcher in the Laboratory of Fundamental Research in the field of Regenerative Medicine at Kuban State Medical University, Russia. She has published more than 70 papers in reputed journals.
E-mail: elenakuevda@yandex.ru