Indexed In
- Open J Gate
- Cosmos IF
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
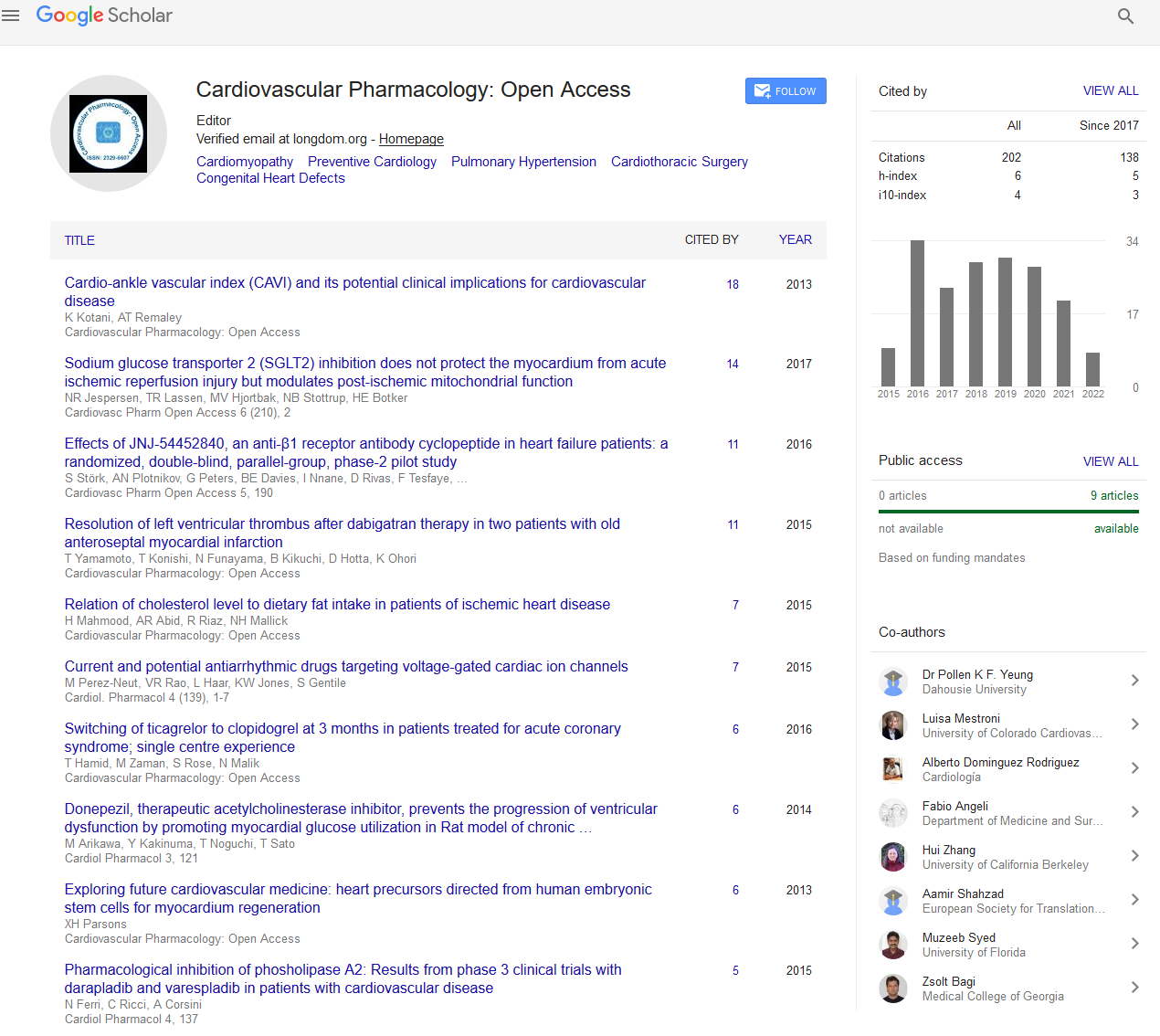
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
A near fatal mistake
International Conference and Expo on Heart and Cardio Care
May 25, 2022 | Webinar
Zahra Hosseini
Iran University of Medical Sciences, Iran
Scientific Tracks Abstracts: Cardiovasc Pharm
Abstract:
Eosinophilic myocarditis is a rare myocardial disease. This form of myocarditis has been identified in 0.5% of cases in an unselected autopsy series and in 0.1% of cases among a cohort of patients biopsied for suspected myocarditis. Etiologies of eosinophilic myocarditis should be considered based on the prevalence of the underlying causes in each area. These etiologies are included: Allergic reactions, Drug-related (Amphotericin B, ampicillin, chloramphenicol, penicillin, tetracycline, streptomycin, cephalosporin, sulfonamides, and antituberculous drugs), antipsychotics (clozapine), antiinflammatory drugs (indomethacin, oxyphenbutazone, and phenylbutazone), diuretics (acetazolamide, chlorthalidone, hydrochlorothiazide, and spironolactone), angiotensin converting enzyme inhibitors (captopril, enalapril), inotropes (dobutamine, digoxin), and others (tetanus toxoid, methyldopa, amitriptyline, lenalidomide, and sulfonylurea). Infections (Strongyloides, Toxocara, Trichinella, Echinococcus and Filaria) Malignancies (GI and urogenital cancers and also in some types of hematologic disorders such as lymphomas, acute lymphoblastic leukemia, acute and chronic myeloid leukemia, eosinophilic leukemia, and rarely in myeloproliferative diseases like polycythemia vera or essential thrombocythosis). Vasculitis (CSS or eosinophilic granulomatosis with polyangiitis), and hyper eosinophilic syndromes (persistent eosinophilia>1500/mm3) for at least six months which is associated with end organ damage. The major involved organs in hyper eosinophilic syndrome (HES) are cardiovascular and neurologic systems. The overall prevalence of cardiovascular involvement is more than 50% such as heart failure (60%), myocardial ischemia, arrhythmias, and pericarditis (4%). Neurologic events could be happened in about 25% of patients. Our patient was a 23-year-old man who was referred to the OR for mitral valve replacement (MVR) due to severe mitral regurgitation with misdiagnosis of congenital hypoplatic posterior MV leaflet without any attention to the eosinophilic count. After detection of hyper-eosinophilia in peripheral blood smear, HES was confirmed by TTE and CMR. As noted above, the meticulous part is characterized the underlying cause, which in this patient, chronic eosinophilic leukemia was denoted by bone marrow biopsy. As this rare disease (HES) has different phases, in this patient, the disease was diagnosed in necrotic phase. So, after assessment for FIP1L1 (FIP 1 like 1), PDGFRA (platelet derived growth factor receptor alpha), and PDGFRB (platelet derived growth factor receptor beta) gene mutation and confirming that the patient is responsive to the Imatinib (Tyrosine kinase inhibitor), the treatment was started and fortunately MVR was performed in the remission phase. After 8 years follow-up.
Biography :
Zahra has completed the GP course from Iran, Shiraz medical university and the general cardiology and Interventional cardiology fellowship from Iran-Tehran medical university. She has participated in more than 40 papers and is one of the writers and editors of the 3 interventional cardiology books which have been published by springer Nature. She will be associated professor of interventional cardiology 1 month later and her interesting field is advanced structural heart disease.