Indexed In
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2021) Volume 5, Issue 5
Validating and Comparing Efficacy of Supplemental Oxygen Delivery via Four Commercially Available Face Masks
Herman Groepenhoff, Danielle Bayoro, Shiv Parikh, Dennis White, Edward A. Rose, Michael J. Pedro and Andreas D. Waldmann*Received: 16-Aug-2021 Published: 06-Sep-2021, DOI: 10.35248/2684-1606.21.5.155
Abstract
Introduction: While closed simple oxygen masks deliver oxygen at high flow rates, the actual FiO2 received varies. Open oxygen masks allow increased comfort for the patient, improved communication and feeding, and higher clearance of carbon dioxide, but may not deliver sufficient FiO2 at higher oxygen flow rates. This was an in vitro study of two open masks (Vyaire AirLife Open, Southmedic OxyMask) and two closed masks (simple oxygen mask, partial rebreather mask) at a variety of oxygen flow rates and tidal volumes in simulated normal and obstructive pulmonary states.
Methods: We tested three sizes each of four different types of masks. Masks were applied to dedicated head models that had internal tubing to simulate the nasal and oral cavities. The masks were attached to an adjustable oxygen supply. The nasal and oral tubes joined together and led to an ASL 5000 lung simulator and simulated tracheal FiO2 was continuously measured using an oxygen sensor. Tests were repeated for different oxygen flow rates using different simulated lung conditions. Each mask was tested nine times for 60 seconds per flow rate after 60 seconds washout.
Results: At oxygen flow rates of 1 and 3 LPM, the open masks were able to deliver incremental FiO2 in excess of room air. At higher flow rates, the median FiO2 measured was similar across all masks, although the variability in measured FiO2 was significantly higher in the closed masks vs. the open masks (p<0.001). Variability in FiO2 was also significantly related to flow rate (p<0.001) in all masks. These patterns were seen in normal and obstructive lung settings.
Conclusion: The AirLife Open and Southmedic OxyMask delivered similar FiO2 across all flow rates in normal and obstructive lung models. The open masks delivered FiO2 that was similar to that seen in the closed masks as flow rates increased beyond 5 LPM. There was a significantly higher variability of FiO2 in the closed masks compared to the open masks at higher oxygen flow rates. Open masks deliver oxygen at levels that are comparable to simple oxygen masks with decreased variability and can be used at flow rates that are lower than those used in closed masks.
Keywords
Oxygen inhalation therapy; Respiratory therapy; Hypoxia; Chronic obstructive pulmonary disease; Dyspnea; Critical care
Introduction
Oxygen is the most prescribed medical therapy in the hospital today, yet considerable limitations exist in its precise delivery with a minimum of discomfort and inconvenience to the patient. The goal of oxygen therapy is to improve oxygenation beyond a level that which the patient can accomplish on his/her own breathing room air.
In providing oxygen therapy, the precise quantity of oxygen delivered must be reliable. The fraction of inspired oxygen (FiO2) is tracked over time to determine how a patient’s status is progressing or declining over time. Increased oxygen requirements correlate with worsening prognosis, prompting further evaluation and treatment, and the oxygen delivery device must reliably and consistently deliver the desired prescribed FiO2. In these conditions, excessive oxygen delivery could be as deleterious as inadequate oxygen, with adverse effects on organ pathophysiology and increased morbidity. Therefore, it is important that the predicted FiO2 delivered matches with the actual FiO2 ordered [1,2].
There are several factors that affect the accuracy of the FiO2 delivered via an oxygen facemask, including characteristics of the delivery device, the patient, and the oxygen flow rate. Patient breathing patterns greatly affect inspired oxygen concentrations when using a facemask. As respiratory rate increases and tidal volume increases, FiO2 tends to decline as a significantly higher percentage of the breath is comprised of entrained room air versus supplemental oxygen [3]. This breathing pattern is typical of patients experiencing respiratory insufficiency or failure in whom oxygen therapy is a mainstay therapeutic modality [4,5]. Oxygen flow rates also play a large role. FiO2 delivered using low- flow devices tends to fall short of predicted values, while high flow systems tend to deliver the set FiO2 more accurately. As the oxygen flow rate increases, the percentage of inspired volume comprised of delivered oxygen increases and the percentage comprised of entrained room air decreases [6].
Device differences are the third major contributor. The addition of a reservoir bag significantly improves reliability of FiO2 when using supplemental oxygen across a variety of tidal volumes and respiratory rates. Device positioning on the face may also contribute to decreased FiO2 compared to expected [5]. Both the patient and the device may move, and a reliable FiO2 despite changing position on the face is critical in the setting of an awake patient. The use of a tight-fitting mask also improves the FiO2 reliability compared to a loose-fitting mask [7]. However, patient discomfort with a tight-fitting mask is a primary contributor to non-compliance of oxygen therapy, making this option unreliable for delivering a set FiO2. A second major factor for patient non- compliance is the inability to maintain activities of daily living. There is a strong relationship between oxygen therapy compliance and the patient’s ability to live and function normally with therapy. Therefore, the ideal oxygen facemask should be loose-fitting and comfortable to wear, reliably delivering a set FiO2 across multiple respiratory patterns and allowing for maintenance of activities of daily living [8].
The most used supplemental oxygen devices are nasal cannula, simple oxygen masks, and non-rebreather masks. Although they each have their own advantages, each has certain shortcomings that prevent them from being the ideal single optimal supplemental oxygen delivery solution. The main advantage of a nasal cannula is patient comfort which has been associated with increased compliance leading to decreased interruptions in therapy. In addition, patients are able to converse, eat, and drink while maintaining continuous oxygen therapy. Although patients tolerate nasal cannulas very well, these devices are only able to provide up to 45% oxygen concentration in patients in respiratory distress, which may not be sufficient to maintain adequate oxygenation [9,10].
Simple oxygen face masks and non-rebreathers have the advantage of providing higher concentrations of oxygen for patients in respiratory distress. However, simple oxygen masks and non- rebreathers have the disadvantages of delivering a narrow range of oxygen concentration (FiO2 30%-60% simple oxygen mask and 60%-80% non-rebreather). The inability to titrate oxygen concentration either higher or lower with one device has been shown to increase hospital costs. Additionally, they create a partial seal and have limited exhalation openings, contributing to the rebreathing of carbon dioxide. If oxygen flows are not maintained above 5 Liters Per Minute (LPM) the rebreathing of carbon dioxide can lead to acute respiratory failure [11-13].
Newer devices known as open oxygen masks have gained popularity due to their ability to deliver a consistent and reliable FiO2 at various flow rates with improved patient comfort, reduced rebreathing of carbon dioxide, and reduced hospital costs. Specifically, these devices can be used at a flow of 1-15 LPM to deliver 24%-90% oxygen and were designed with one or more large openings to help clear carbon dioxide efficiently and prevent rebreathing. Additionally the large holes were designed to improve activities of daily living by allowing the patient to drink and communicate. Recent studies comparing open oxygen masks to traditional oxygen masks found that open oxygen masks significantly decreased the amount of rebreathing. Another recent study demonstrated that converting to open oxygen masks only within an institution vs. using a nasal cannula, simple oxygen mask, and non-rebreather lead to less severe complications as well as significant cost reductions due to utilizing less oxygen, fewer oxygen devices, and a reduced escalation in care [14-17].
Although these recent studies have shown that open oxygen masks provide a wider range of oxygen concentrations, improvements are still needed. Mask position can have an important effect on delivered oxygen levels. Shin et al. recently compared the impact of mask position on oxygen delivery between non-rebreathers and the OxyMaskTM (Southmedic, Barrie, ON, Canada). Non- rebreather masks were significantly more affected by mask position than were the OxyMasks in both expired gases (expired oxygen and expired carbon dioxide) and comfort [18].
The AirLifeTM Open Plus mask (Vyaire Medical Mettawa, IL) is a novel open oxygen mask designed to address current open mask limitations by accurately and consistently delivering supplemental oxygen despite variations in oxygen flow rates and the patient’s respiratory condition. The primary objective of this study is to compare the efficacy of oxygen delivery between the Air-life Open plus mask (AO), the OxyMask open oxygen mask (OM), and traditional simple and partial rebreather oxygen face masks in a simulated model with various breath rates, tidal volumes, and breathing patterns.
Methods
Study setup and protocol
In this bench study, an active lung simulator (ASL 5000, Ingmar Medical, Pittsburg, Pennsylvania) was connected by an adapter to the simulated trachea of a mannequin face to compare four different face masks: 1) AirLife Open (Vyaire Medical, Mettawa, IL, USA) (small, medium, and large); 2) a simple mask (Vyaire Medical, Mettawa, IL) (small and medium) covering nose and mouth; 3) a partial rebreather mask (Vyaire Medical, Mettawa, IL) (pediatric and adult) covering the nose and mouth; and 4) OxyMask (Southmedic, Barrie, Canada) (Kid, Medium, and Plus), an open mask.
Each tested oxygen mask was attached to an oxygen source and affixed to the mannequin head with an elastic strap, each mannequin face featured a nasal airway path and an oral airway path that were joined into a single pathway posterior to the simulated face. Between the bifurcation and the lung simulator, air was passed through a filter (Vyaire Medical, Mettawa, IL) for mixing and smoothing of airflow and an air sampling tube leading to an oxygen sensor.
FiO2 flow rates were adjusted to deliver between (1 and 15) liters per minute. Novel airway mannequins in different sizes were designed specifically for this study, containing independent nasal and oral gas paths. Tidal breathing and lung conditions were simulated using the ASL 5000 test lung and O measurements were recorded using an Oxigraf O CAP Oxygen/CO2 Analyzer (Oxigraf Inc., Sunnyvale, CA) see Figure 1.
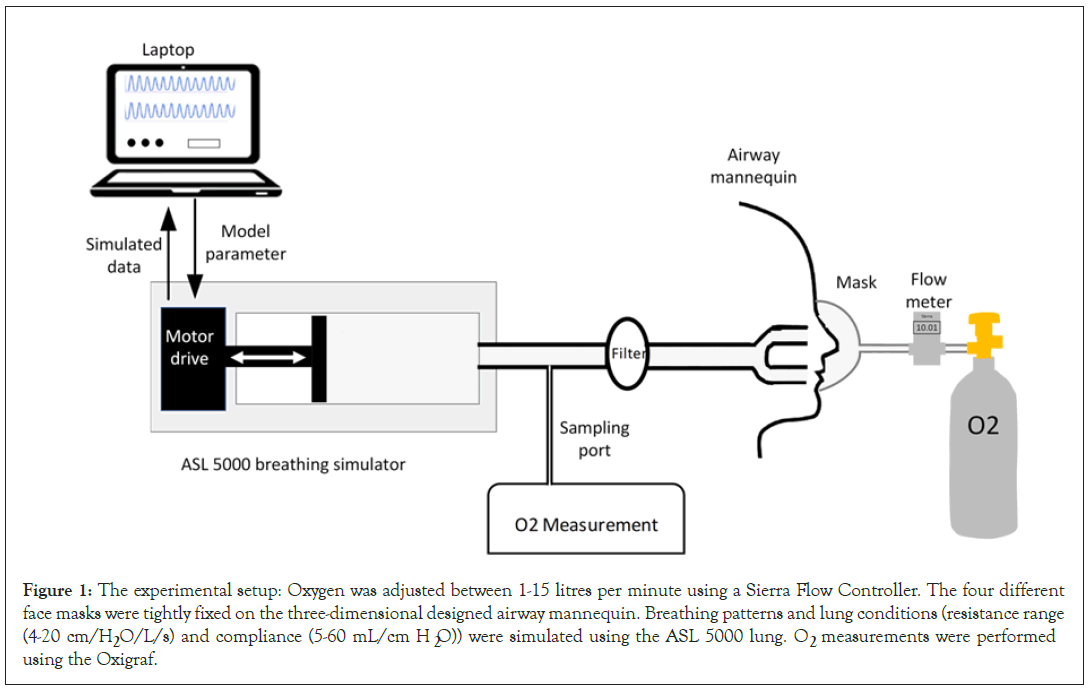
Figure 1: The experimental setup: Oxygen was adjusted between 1-15 litres per minute using a Sierra Flow Controller. The four different face masks were tightly fixed on the three-dimensional designed airway mannequin. Breathing patterns and lung conditions (resistance range (4-20 cm/H2O/L/s) and compliance (5-60 mL/cm H2O)) were simulated using the ASL 5000 lung. O2 measurements were performed using the Oxigraf.
Mannequins
Three facial mannequins were designed based upon computer- aided design models purchased from Anthrotec (Yellow Springs, OH) see Figure 2.
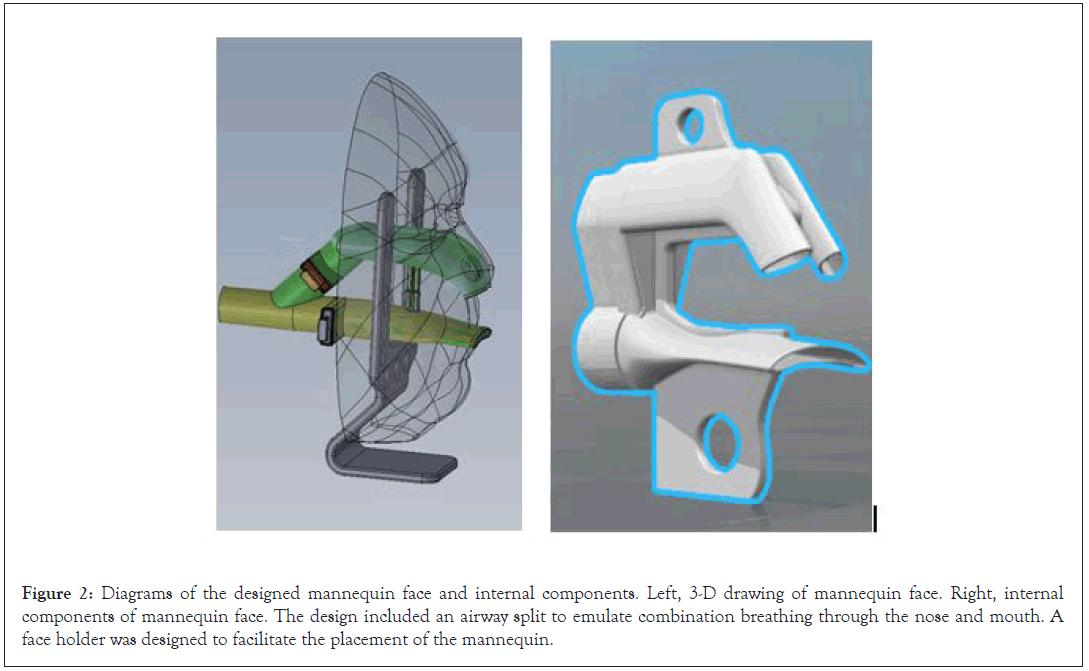
Figure 2: Diagrams of the designed mannequin face and internal components. Left, 3-D drawing of mannequin face. Right, internal components of mannequin face. The design included an airway split to emulate combination breathing through the nose and mouth. A face holder was designed to facilitate the placement of the mannequin.
The models were derived from demographic anthropomorphic data presented in a NIOSH study of subjects working in various occupations that utilize respirators in a work setting. These data were divided into three age strata, two gender strata, and four racial strata [19]. We selected two facial metrics (bizygomatic breadth and Menton-Sellion length) to create large, standard, and small size mannequin faces based on a large adult, a small adult, and a child based on the NIOSH data.
The nasopharyngeal and oropharyngeal passages were generated in SolidWorks (Dassault Systèmes, Tennessee) by creating cross-sectional loft sketches that matched the facial, head, and throat features of CT scans [20]. Images are properly scaled to the scanned models and have approximated key features (such as a nasal septum, nasal vestibules, kidney-shaped nostrils, tongue bulge, etc.) which were most appropriate to the influence of breath flow patterns in the mask volumes. The pharyngeal passages were 3-D printed in nylon and positioned in 3-D printed mold cavities generated from the head scans. Silicone casting rubber was then poured into the mold cavity to form the test heads with the embedded breathing passages. Standard 22 mm taper-fit respiratory circuit connectors were used to connect these mannequin faces to the ASL machine and each face was in turn mounted to a support plate.
Data acquisition and analysis
We applied a wide range of flow rates as indicated by the manufacturer of the lung simulator, and selected compliance and resistance settings to mimic normal and obstructive lung conditions. Age-dependent breathing frequencies and target tidal volumes were used to test the different masks (Table 1).
| Target | Lung Model | Effort Model | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Set# | Age | Mask | State | Height (cm) | IBW (kg) | Vt (ml) | Resistance (cm/H2O/L/s) | Compliance (mL/cm H2O) | Frequency (bpm) | Pmax (cm H2O) | Increase (%) | Release (%) |
| 1 | Child | Small | Normal | 114 | 17.8 | 130 | 8 | 31 | 26 | 5.171 | 40 | 50 |
| 2 | Child | Small | Normal | 165 | 63.2 | 490 | 4 | 5 | 15 | 10.332 | 25 | 30 |
| 3 | Adult | Med | Normal | 150 | 41.6 | 320 | 4 | 50 | 15 | 6.737 | 25 | 30 |
| 4 | Adult | Med | Normal | 206 | 92.1 | 720 | 4 | 50 | 15 | 15.209 | 25 | 30 |
| 5 | Adult | Large | Normal | 196 | 84.6 | 660 | 4 | 50 | 15 | 13.914 | 25 | 30 |
| 6 | Adult | Large | Normal | 221 | 103 | 810 | 4 | 50 | 15 | 17.076 | 25 | 30 |
| 7 | Adult | Small | COPD | 165 | 63.2 | 490 | 8-20 | 60 | 20 | 14.115 | 34 | 22 |
| 8 | Adult | Med | COPD | 150 | 41.6 | 320 | 8-20 | 60 | 20 | 12.566 | 34 | 22 |
| 9 | Adult | Med | COPD | 206 | 92.1 | 720 | 8-20 | 60 | 20 | 28.242 | 34 | 22 |
| 10 | Adult | Large | COPD | 196 | 84.6 | 660 | 8-20 | 60 | 20 | 25.897 | 34 | 22 |
| 11 | Adult | Large | COPD | 221 | 103 | 810 | 8-20 | 60 | 20 | 31.777 | 34 | 22 |
Abbreviations: IBW: Ideal Body Weight; VT: Tidal Volume; BPM: Breaths Per Minute; COPD: Chronic Obstructive Pulmonary Disease.
Table 1: ASL 5000 breathing simulator parameters: Software-only mode.
The parameters were selected according to face mask size. O2 measurements were digitalized at a sampling rate of 108.7 Hz for 60 seconds and the data was analyzed offline. The average of FiO2 delivery was then calculated for all measurements at each flow rate and separately for normal and obstructive lung conditions.
Statistical analysis
Data were analyzed using the Friedman test and Dunn’s Multiple Comparison test for non-parametric data. Two-way analysis of variance (ANOVA) was used to evaluate the differences between the different masks and different oxygen flow rates. Statistical analysis was performed using Minitab software (Minitab, LLC, State College, PA). A p-value<0.05 was considered significant.
Data are presented as boxplots based on these calculations, allowing rapid visualization of datasets. The boxplots have a box extending from the 25th to the 75th percentile with the median as a horizontal line within this box. This represents the Inter Quartile Range (IQR) of the data. Above and below the boxes, the whiskers are the maximum and minimum values up to 1.5 times the IQR.
Results
Measured FiO2 data from adult and pediatric models are shown in Figures 3 and 4.
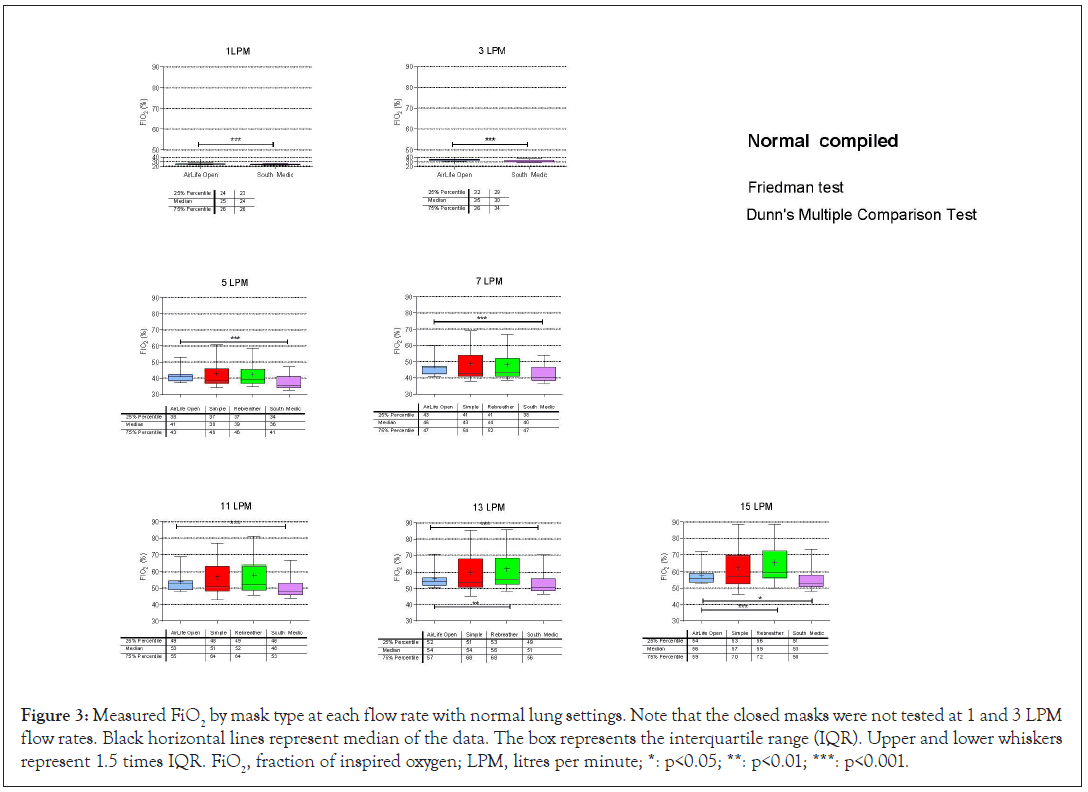
Figure 3: Measured FiO2 by mask type at each flow rate with normal lung settings. Note that the closed masks were not tested at 1 and 3 LPM flow rates. Black horizontal lines represent median of the data. The box represents the interquartile range (IQR). Upper and lower whiskers represent 1.5 times IQR. FiO2, fraction of inspired oxygen; LPM, litres per minute; *: p<0.05; **: p<0.01; ***: p<0.001.
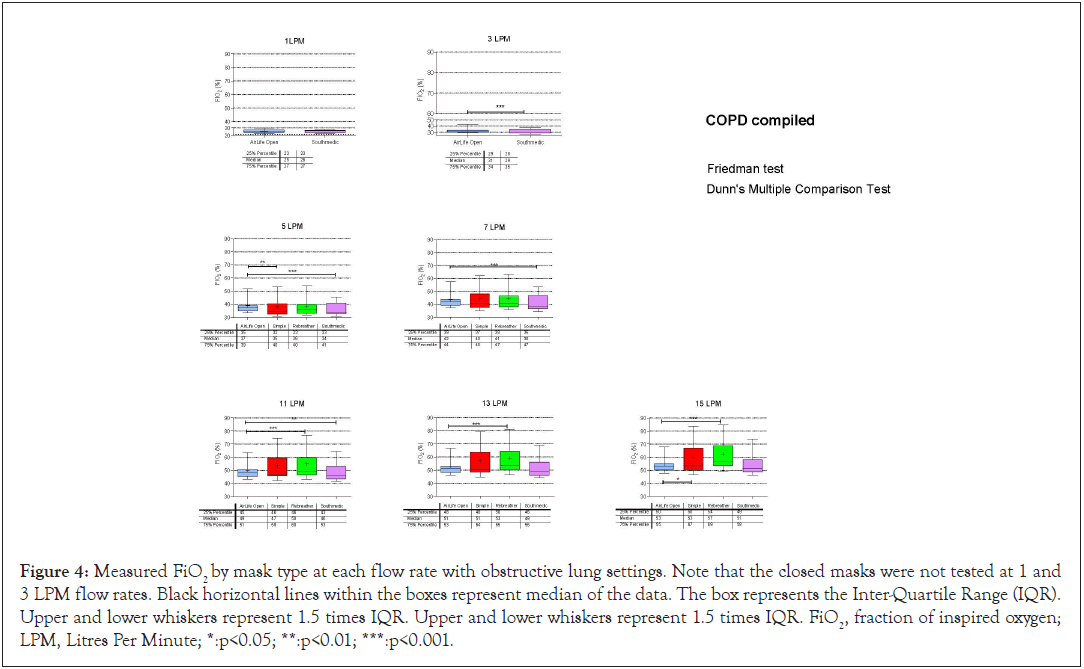
Figure 4: Measured FiO2 by mask type at each flow rate with obstructive lung settings. Note that the closed masks were not tested at 1 and 3 LPM flow rates. Black horizontal lines within the boxes represent median of the data. The box represents the Inter-Quartile Range (IQR). Upper and lower whiskers represent 1.5 times IQR. Upper and lower whiskers represent 1.5 times IQR. FiO2, fraction of inspired oxygen; LPM, Litres Per Minute; *:p<0.05; **:p<0.01; ***:p<0.001.
The AirLife Open mask delivers FiO2 proportional to the oxygen flow rate as expected. While there is some variability around each data point, the variability for the Air Life Open mask appears to be consistent with, and often smaller than, that for the other masks. The closed masks delivered higher FiO2 at higher flow rates than did either of the open masks. Data for both obstructive and normal lung models for all masks and all flow rates are shown in Figures 5 and 6.
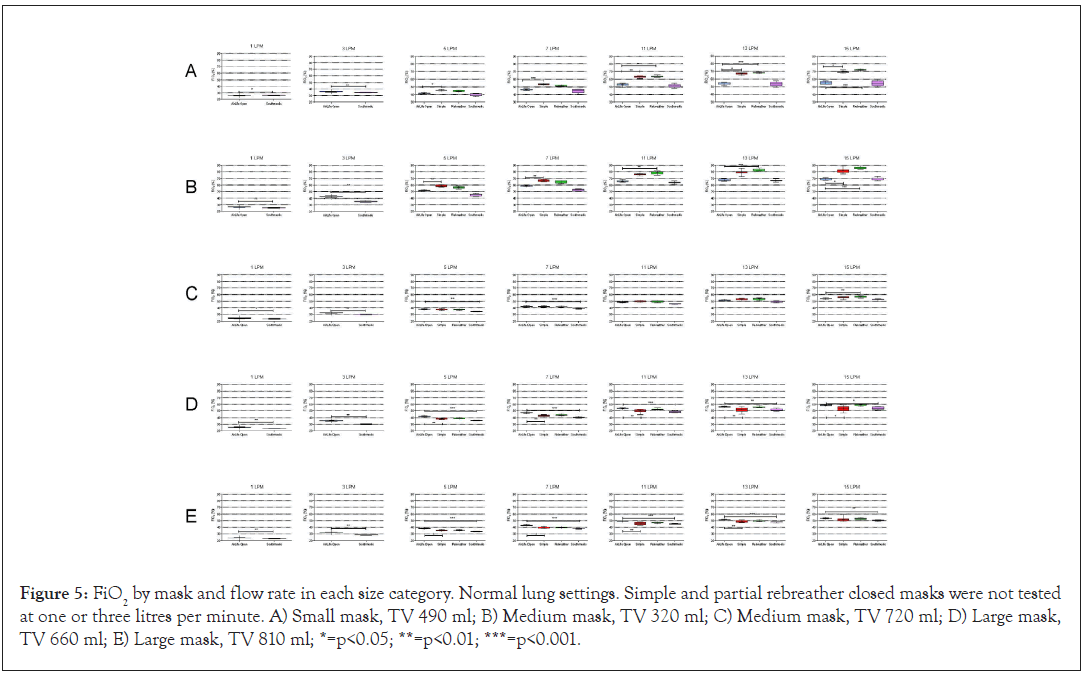
Figure 5: FiO2 by mask and flow rate in each size category. Normal lung settings. Simple and partial rebreather closed masks were not tested at one or three litres per minute. A) Small mask, TV 490 ml; B) Medium mask, TV 320 ml; C) Medium mask, TV 720 ml; D) Large mask, TV 660 ml; E) Large mask, TV 810 ml; *=p<0.05; **=p<0.01; ***=p<0.001.
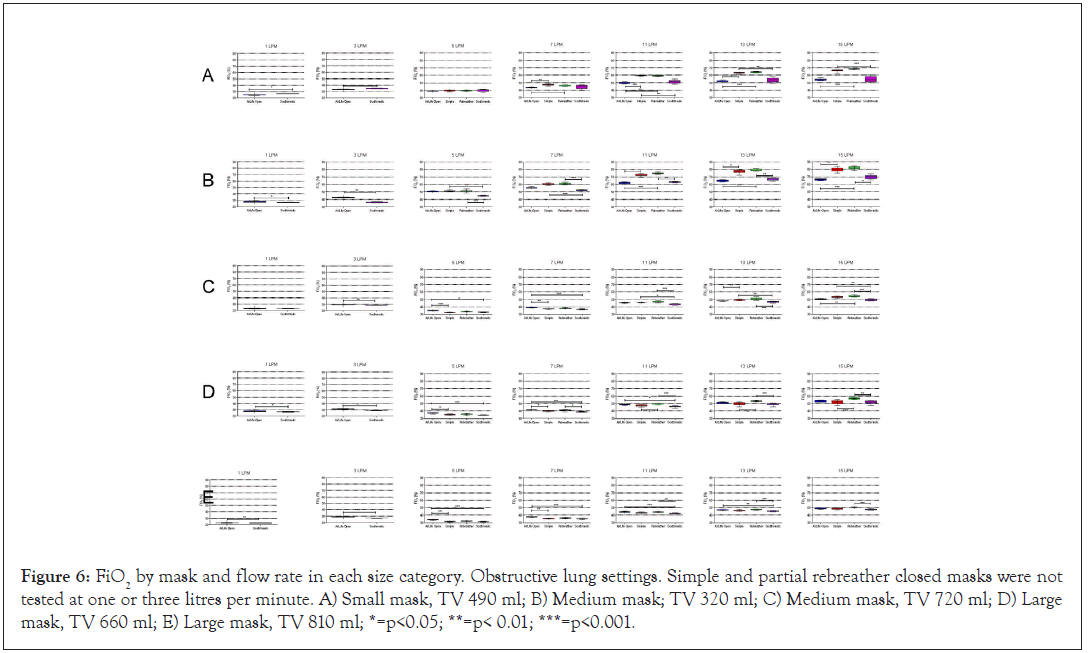
Figure 6: FiO2 by mask and flow rate in each size category. Obstructive lung settings. Simple and partial rebreather closed masks were not tested at one or three litres per minute. A) Small mask, TV 490 ml; B) Medium mask; TV 320 ml; C) Medium mask, TV 720 ml; D) Large mask, TV 660 ml; E) Large mask, TV 810 ml; *=p<0.05; **=p< 0.01; ***=p<0.001.
At levels of 1 and 3 LPM, the open masks performed similarly, although the differences in median FiO2 did reach statistical significance at 3 LPM. As LPM was increased, the FiO2 delivered by the closed masks showed significant increases in variability compared to the measurements from the closed masks despite similar mean values across all masks.
At low flow rates (1 and 3 LPM), the data show that the Air Life Open and the OxyMask delivered similar FiO2 in all sizes over all tidal volumes. The closed masks cannot be used at these lower flow rates and were not tested in this study. Variability of FiO2 was analyzed using stepwise multiple linear regressions. Results are shown in Tables 2 and 3.
| Normal lung | Unstandardized coefficients | Standardized coefficients | |||
|---|---|---|---|---|---|
| B | Std error | Beta | t | p value | |
| Constant (AO) | 7.577 | 1.857 | 4.081 | 0.001 | |
| AO vs. simple | 15.800 | 1.544 | 0.802 | 10.231 | <0.001 |
| AO vs. PRB | 13.600 | 1.544 | 0.690 | 8.806 | <0.001 |
| AO vs. oxymask | 1.200 | 1.544 | 0.061 | 0.777 | 0.449 |
| Flow rate | 1.140 | 0.147 | 0.495 | 7.742 | <0.001 |
Abbreviations: AO: Air Life Open; Simple: Simple Mask; PRB: Partial Re-Breather.
Table 2: Stepwise linear regression analysis of variance of FiO2 comparing air life open mask to other masks and evaluating impact of oxygen flow rates on variability of FiO2. Normal lung settings. Dependent variable: FiO2 range.
| Obstructive lung | Unstandardized coefficients | Standardized coefficients | |||
|---|---|---|---|---|---|
| B | Std error | Beta | t | p value | |
| Constant (AO) | 9.222 | 1.832 | 5.033 | <0.001 | |
| AO vs. simple | 10.600 | 1.524 | 0.698 | 6.955 | <0.001 |
| AO vs. PRB | 10.600 | 1.524 | 0.698 | 6.955 | <0.001 |
| AO vs. Oxymask | 2.000 | 1.524 | 0.132 | 1.312 | 0.209 |
| Flow rate | 1.057 | 0.145 | 0.596 | 7.274 | <0.001 |
Abbreviations: AO: Air Life Open; Simple: Simple Mask; PRB: Partial Re-Breather.
Table 3: Stepwise linear regression analysis of variance of FiO2 comparing AirLife Open mask to other masks and evaluating impact of oxygen flow rates on variability of FiO2. Obstructive lung settings. Dependent variable: FiO2 range.
These calculations show that Air Life Open has less variability in FiO2 delivery compared to both simple masks (p<0.001) and partial rebreather masks (p<0.001) in both normal and obstructive lung settings. FiO2 variability in the Air Life Open was not different from that of the Southmedic OxyMask. Finally, regression analysis confirmed that variability in FiO2 was significantly increased with higher flow rates (p<0.001).
Discussion
In this study, we evaluated four different oxygen masks of different sizes over a wide variety of oxygen flow rates. We included low flow rates that cannot be used by closed masks due to risks of asphyxiation and carbon dioxide retention. There are clinical scenarios in which a clinician may want to supply a small amount of additional oxygen to a patient who cannot use a nasal cannula (for example, facial trauma or nasal surgery), and 1-3 LPM oxygen flow could be beneficial. This is not possible with closed masks. We also tested the masks in simulated normal and obstructive pattern lungs over a range of tidal volumes. Air was sampled for oxygen measurement from a simulated tracheal position (just outside the lung simulator), improving the accuracy of FiO2 interpretation. Finally, data were collected from a series of nine iterations of data collection. The resultant dataset should represent a robust evaluation of these four masks under these conditions.
There were some subtle differences in median FiO2 delivered across all sizes of masks in pediatric and adult models and normal and obstructive lung models, but the differences were small at low flow rates. However, the variability in FiO2 delivery was significantly higher in the simple and partial rebreathing masks compared to the AirLife Open mask and the OxyMask. This variability echoes the results seen in the study by Katz who found variability of up to 60% in FiO2 at high flow rates using nasal cannula. With open masks, high tidal volumes lead to higher entrainment of room air, reducing both the concentration and the variability of FiO2 delivered. Patient position, mouth position, mask fit, and a variety of other factors affect oxygen delivery with all masks [21,22].
Measurement of FiO2 in research is challenging, both in vitro and particularly in vivo. Accurate in vivo measurement requires tracheal sampling, an invasive and uncomfortable process. Published studies rely on a variety of different models, assumptions, and procedures, resulting in widely disparate results. For example, in healthy volunteers, FiO2 delivered by the OxyMask at oxygen flow rates ranging from 1.5 LPM to 30 LPM were higher than that measured in our model. While oxygen flow rates of 15 LPM produced a mean FiO2 of 53% in our study, Paul reported a FiO2 of 80.1%. In that study, however, oxygen concentration was measured at the face rather than in the trachea, so actual FiO2 is unknown. Ogiwara and team compared the OxyMask to a simple oxygen mask in healthy children. At 15 LPM, the researchers noted that measured FiO2 reached 80% in their study. However, in their study, once again FiO2 was not measured in the trachea but rather from a sampling tube placed in the nose, very near the oxygen source. In 2016, Lamb et al. reported a FiO2 of 71.9% at 15 LPM with the Southmedic mask in a simulator and a FiO2 of 68.6% with a non-rebreather at 15 LPM. Their experimental setup involved placing a sampling tube 1 inch into the simulated mouth, again very near the oxygen source. Used models to study oxygen flow rates in the OxyMask compared to a simple mask [23]. At a flow rate of 15 LPM, FiO2 was measured at 74.1%. Their study did utilize intratracheal sampling of air. In contrast, in unpublished data by Sorg and Chatburn using an adult mannequin head, the AirLife Open produced a FiO2 of 58% while the OxyMask produced a FiO2 of 52% at 15 LPM (unpublished abstract).
In essence, besides the one study and an unpublished abstract, there are no studies in the literature against which to compare our results. It is published as an abstract with few details regarding flow rates, number of simulations, or leak. Clearly accurate assessment of FiO2 is challenging given variations in technique and set-ups. In our study, using numerous runs of measurements over numerous simulated lung settings, we found that all masks performed similarly at each flow rate.
The open masks in our study showed a distinct advantage in consistency of FiO2 delivered at higher flow rates compared to that of the closed masks. The wide range of variability in FiO2 seen in the closed masks, particularly at higher flow rates, may be problematic in clinical practice. Higher than expected oxygen dosing may be well tolerated by some patients but may promote respiratory suppression and CO2 retention in patients with Chronic Obstructive Pulmonary Disease (COPD). In fact, hyperoxia has been associated with direct coronary vasoconstriction and increases in myocardial oxygen consumption [24].
The AirLife Open masks, like the Southmedic OxyMask, have an advantage of being useful at lower oxygen flow rates. Closed face masks cannot be used at less than 5 LPM FiO2 because this level of oxygen flow does not meet minimum minute ventilation. Open masks augment entrained room air so that they are able to achieve minimum required levels of oxygen with small additional levels of supplementation. Inadequate flow of a closed mask may contribute to the accumulation of carbon dioxide and CO2 narcosis, while open masks allow adequate clearance of CO2 [25].
A limitation of our study is that it is not in vivo and relies on a simulation. The ASL 5000 has been well validated in numerous publications, and the OxyGraf analyzer is a patient care level device. We believe that the mannequin that we have designed is accurate, and each oxygen mask was fit-tested for each mannequin face. The protocol involved numerous repetitions over a spectrum of oxygen flow rates in both simulated healthy and simulated diseased patients using settings that are also well validated from the literature. Carbon dioxide clearance or accumulation may provide added incentive to use open masks in certain patients and was not tested in this study. We suggest that a similar study be undertaken in vivo along with capnometry.
Conclusion
In this bench study, the AirLife Open mask achieved levels of FiO2 that were comparable to those of the OxyMask and the two closed masks at all levels of oxygen flow tested. The variability of FiO2 seen with the AirLife was significantly lower than that seen in the closed masks and similar to the OxyMask variability. The AirLife Open mask provides more consistent oxygen delivery over a wider range of oxygen flow rates than a standard closed mask, allowing more predictable control of oxygen dosing during therapeutic oxygen treatment.
Disclosure
Test equipment and testing facilities were provided by Vyaire Medical. All authors are employed by Vyaire Medical. Vyaire designed the study, collected and analyzed data, and interpreted the results.
Acknowledgements
None
Ethical Statement
This in vitro study did not require ethical approval.
REFERENCES
- Brueckl C, Kaestle S, Kerem A, Habazettl H, Krombach F, Kuppe H, et al. Hyperoxia-induced reactive oxygen species formation in pulmonary capillary endothelial cells in situ. Am J Respir Cell Mol Biol. 2006; 34(4): 453-463.
- Farquhar H, Weatherall M, Wijesinghe M, Perrin K, Ranchord A, Simmonds M, et al. Systematic review of studies of the effect of hyperoxia on coronary blood flow. Am Heart J 2009; 158(3): 371-377. 2009/08/25.
- Katz I, Chen J, Duong K, Zhu K, Pichelin M, Caillibotte G, et al. Dose variability of supplemental oxygen therapy with open patient interfaces based on in vitro measurements using a physiologically realistic upper airway model. Respir Res 2019; 20(1): 149.
- Sim MA, Dean P, Kinsella J, Black R, Carter R, Hughes M. Performance of oxygen delivery devices when the breathing pattern of respiratory failure is simulated. Anaesthesia. 2008; 63(9): 938-940.
- Wagstaff TA, Soni N. Performance of six types of oxygen delivery devices at varying respiratory rates. Anaesthesia. 2007; 62(5): 492-503.
- Bateman NT, Leach RM. ABC of oxygen. Acute oxygen therapy. BMJ. 1998; 317(7161): 798-801.
- Boumphrey SM, Morris EA, Kinsella SM. 100% inspired oxygen from a Hudson mask-a realistic goal? Resuscitation. 2003; 57(1): 69-72.
- Eastwood GM, O'Connell B, Gardner A, Considine J. Patients' and nurses' perspectives on oxygen therapy: A qualitative study. J Adv Nurs. 2009; 65(3): 634-641.
- Eastwood GM, O'Connell B, Gardner A, Considine J. Evaluation of nasopharyngeal oxygen, nasal prongs and facemask oxygen therapy devices in adult patients: A randomised crossover trial. Anaesth Intensive Care. 2008; 36(5): 691-694.
- Wettstein RB, Shelledy DC, Peters JI. Delivered oxygen concentrations using low-flow and high-flow nasal cannulas. Respir Care. 2005; 50(5): 604-609.
- Pruitt WC, Jacobs M. Breathing lessons: Basics of oxygen therapy. Nursing. 2003; 33(10): 43-45.
- DeJuilio PA, Jenkins MB, Huml JP. Evaluation of safety and cost of an open-design oxygen mask in a large community hospital. Respir Care. 2018; 63(4): 412-416.
- Phillips JS, Pangilinan LP, Mangalindan ER, Booze JL, Kallet RH. A comparison of different techniques for interfacing capnography with adult and pediatric supplemental oxygen masks. Respir Care. 2017; 62(1): 78-85.
- Paul JE, Hangan H, Hajgato J. The oxymaskTM development and performance in healthy volunteers. Med Devices (Auckl). 2009; 2: 9-17.
- Beecroft JM,Hanly PJ. Comparison of the oxymask and venturi mask in the delivery of supplemental oxygen: Pilot study in oxygen-dependent patients. Can Respir J. 2006; 13(5): 247-252.
- Lamb K, Piper D. Southmedic oxymask (TM) compared with the hudson RCI (R) non-rebreather mask (TM): Safety and performance comparison. Can J Respir Ther. 2016; 52(1): 13-15.
- Ogiwara S, Tamura T, Sai S, Nojima M, Kawana S. Superiority of oxymask (TM) with less carbon dioxide rebreathing in children. Eur J Pediatr. 2021: 1-5.
- Shin HJ, Choi JH, Lee JW, Moon HJ, Park Sh, et al. A Single-center, Prospective, cross-over study to compare the efficiency of oxygen supply between the oxymasktm and non-rebreather mask in healthy adults. J Korean Society Emergency Med. 2017; 28(1): 17-25.
- Zhuang Z, Bradtmiller B. Head-and-face anthropometric survey of U.S. respirator users. J Occup Environ Hyg. 2005; 2(11): 567-576.
- Zhao K, Scherer PW, Hajiloo SA. Effect of anatomy on human nasal air flow and odorant transport patterns: implications for olfaction. Chem Senses. 2004; 29(5): 365-379.
- Nugent OA, Kelly PT, Stanton J, Swanney MP, Graham B. Measurement of oxygen concentration delivered via nasal cannulae by tracheal sampling. Respirol. 2014; 19: 538-543.
- Bazuaye EA, Stone TN, Corris PA, Gibson GJ. Variability of inspired oxygen concentration with nasal cannulas. Thorax. 1992; 47(8): 609-611.
- Sonetti DA, Vines DL, Peters J. Comparison of inspired oxygen between an oxymask and simple mask and nasal cannula. Chest. 2009; 136(4): 126S.
- Kallstrom TJ. AARC clinical practice guideline: Oxygen therapy for adults in the acute care facility-2002 revision and update. Respir Care. 2002; 47: 717-720.
- Jensen AG, Johnson A, Sandstedt S. Rebreathing during oxygen treatment with face mask. The effect of oxygen flow rates on ventilation. Acta Anaesthesiol Scand. 1991; 35: 289-292.
Citation: Groepenhoff H, Bayoro D, Parikh S, White D, Rose EA, Pedro MJ, et al. (2021) Validating and Comparing Efficacy of Supplemental Oxygen Delivery via Four Commercially Available Face Masks. J Surg Anesth. 5:155.
Copyright: © 2021 Waldmann DA et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
