Indexed In
- Academic Journals Database
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Scimago
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
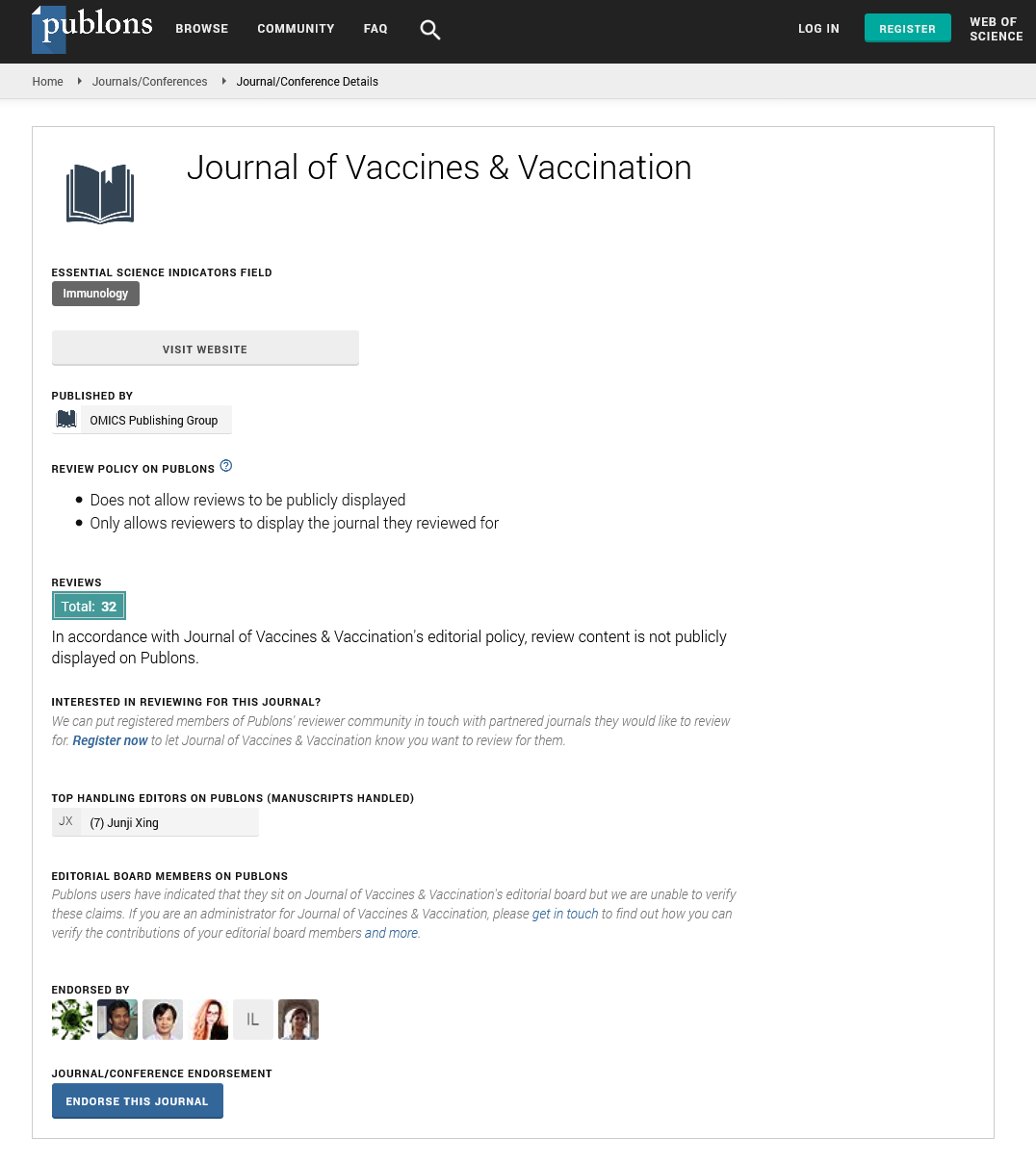
- Publons
- MIAR
- University Grants Commission
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2024) Volume 15, Issue 5
Vaccine Candidates, Immuno-Dominant Antigens and Potent Vaccine Adjuvants for Preventing Cutaneous Leishmaniasis: A Systematic Review
Abiy Ayele Angelo1*, Gashaw Adane1, Yeshambel Belyhun1, Bisrat Birke Teketelew2, Dereje Mengesha Berta2, Elias Chane3, Negesse Cherie4 and Mesele Nigus42Department of Hematology and Immunohematology, School of Biomedical and Laboratory Sciences, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
3Department of Clinical Chemistry, School of Biomedical and Laboratory Sciences, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
4Department of Quality Assurance and Laboratory Management, School of Biomedical and Laboratory Sciences, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Received: 13-Sep-2024, Manuscript No. JVV-24-26924; Editor assigned: 16-Sep-2024, Pre QC No. JVV-24-26924 (PQ); Reviewed: 30-Sep-2024, QC No. JVV-24-26924; Revised: 07-Oct-2024, Manuscript No. JVV-24-26924 (R); Published: 14-Oct-2024, DOI: 10.35248/2157-7560.24.15.568
Abstract
Cutaneous leishmaniasis (CL) is the most common clinical form of leishmaniasis that causes skin disease. Currently, there is no licensed prophylactic vaccine for CL, as the mechanisms of healing and memory T-cell responses that develop after infection with CL are far from fully understood. A review of the published articles identifying CL vaccine candidates, immuno-dominant antigens and potent vaccine adjuvants is needed to provide comprehensive information. Therefore, we aimed to review vaccine candidates, immuno-dominant antigens and potent vaccine adjuvants for preventing cutaneous leishmaniasis.
First-generation vaccine candidates showed complete protection of the specified animal model. They induced strong T-cell mediated and antibody-mediated humoral immune responses (e.g. Curdlan dectin-1, Total Leishmania Antigen (TLA) and L. infantum heat shock proteins (LiΔHSP70-II)). Almost all second and third-generation vaccine candidates and the immuno-dominant antigens of the parasite and the host enhance T cell-mediated and antibody-mediated immune responses. We also reviewed potent vaccine adjuvants such as Myrrh Silver Nanoparticles (MSNPs) and Imiquimod, which play an important role in enhancing immune responses against Leishmania antigens. The T-cell mediated immune response was significantly induced in various experimental models (e.g. IFN-γ and TNF-α response) and also the humoral arm in some instances (e.g. IgG2). This review thus provides comprehensive information on the efficacy and induction of protective immunity of vaccine candidates, antigenic molecules and vaccine adjuvants against CL. However, there is still a need for a comprehensive understanding of the immuno-pathogenesis of the disease upon vaccination.
Keywords
Cutaneous leishmaniasis; Vaccine candidates; Immuno-dominant antigens; Potent vaccine adjuvants
Abbreviations
AMPs: Antimicrobial Peptides; APCs: Antigen Presenting Cells; CL: Cutaneous Leishmaniasis; CLR: C-type Lectin Receptors; CNPs: Copper Nano-Particles; CRAMP: Cathelicidinrelated Antimicrobial Peptides; DC: Dendritic Cells; DCL: Diffuse Cutaneous Leishmaniasis; DTH: Delayed Type Hypersensitivity; GP63: Glycoprotein-63; HASPB: Hydrophilic Acylated Surface Protein B; JBI: Joanna Briggs Institute’s; KMP11: Kinetoplastid Membrane Protein 11; LACK: Leishmania Homolog of Receptors for Activated C-kinase; LiHSP70-11: L. infantum Heat Shock Protein 70-11; LPG: Lipo-Phsphoglycan; MCL: Mucocutaneous Leishmaniasis; MSNPs: Myrrh Silver Nanoparticle; NO: Nitric Oxide; PEPCK: Leishmania Phospho-Enol-Pyruvate Carboxy-Kinase; PKDL: Post Kalazar Dermal Leishmaniasis; PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses; PROSPERO: Prospective Register of Systematic Reviews; PRR: Pattern Recognition Receptor; ROS: Reactive Oxygen Species; SDLNs: Skin-Draining Lymph Nodes; SNPs: Silver Nanoparticles; STI1: Stress-Inducible Protein-1; TH1: T helper 1 cells; TLA: Total Leishmania Antigen; TLR: Toll Like Receptor; TSA: Thiol- Specific Antioxidant; VL: Visceral Leishmaniasis
Introduction
Cutaneous leishmaniasis (CL) is the most prevalent form of leishmaniasis and is characterized by skin lesions that can ulcerate and leave disfiguring scars that lead to discrimination in affected communities [1]. CL encompasses a spectrum of self-healing and chronic skin diseases [2]. The clinical presentation varies depending on the parasite load and host immune response [3]. Common signs of CL are skin papules and ulcerations whereas symptoms may include: Breathing difficulty, skin sores that develop into a slow-healing skin ulcer, closed nose, runny nose, nosebleeds and swallowing difficulty [4].
During a blood meal, flagellated promastigotes deposited in the dermis are ingested by phagocytes such as neutrophils and macrophages, where they transform into amastigotes, a stage of the parasite that copes better with changes in temperature and pH. Amastigotes multiply within the phagocyte until they rupture the cell and infect other tissues. The rapid recruitment of neutrophils and inflammatory monocytes after infection with Leishmania influences the course of the disease [5]. Neutrophils can have both a protective and a damaging function, while inflammatory monocytes kill Leishmania parasites and differentiate into monocyte-derived dendritic cells that promote the development of protective CD4+ T helper 1 (TH1) cells [6]. Control of Leishmania infection depends on the production of IFN-γ by CD4+ TH1 cells, resulting in enhanced killing by macrophages due to the production of reactive oxygen species and nitric oxide [7].
The immunological spectrum observed in CL patients ranges from individuals with a strong T-cell response characterized by delayedtype hypersensitivity (DTH) and high IFN-γ levels to individuals who have no DTH response but possibly high antibody levels [8]. Leishmania species are killed by IFN-γ-activated macrophages and not neutralized by antibodies, individuals with a strong DTH have few parasites in their lesions, while those with only a humoral response are unable to control the parasite load [8,9]. Patients without a T-cell response are expected to develop severe disease, termed Diffuse Cutaneous Leishmaniasis (DCL). At the other end of the spectrum, patients with an exaggerated immune response due to immunopathology also develop a severe disease phenotype, Mucocutaneous Leishmaniasis (MCL). Most MCL patients have lesions on the lip and around the nose where the skin and mucosa meet [4]. Between these extremes are patients who develop lesions that can heal themselves or become chronic, with intermediate levels of T cells and antibody responses [10].
Cutaneous leishmaniasis lesions self-heal without treatment in over 70% of patients, depending on the immune response and the species of Leishmania [11]. Intralesional or systemic antimonial is the gold standard for treating CL; other therapeutic options (e.g. parmomycin, Imiquimod ointments and cryotherapy) appear promising [12]. At the moment, vector control and rational treatment are the only ways to treat and control but, there aren’t plenty of medicines on the market and the available ones are either very expensive, have harmful side effects, or are ineffective. However, the vector control techniques are not as effective [13].
A better understanding of the immune response in the pathogenesis of CL is still needed, taking into account the different species that cause different clinical manifestations of the disease [14]. The fact that we are still far from fully understanding the mechanisms of healing and memory responses that form after infection with CL and how to evaluate these responses, is one of the factors contributing to a failure to develop a vaccine for CL [15]. Although studies have been conducted on vaccine trials for CL in different study settings, there has been no fully licensed effective vaccine for human usage [16,17]. The development of a leishmaniasis vaccine that is safe, effective and reasonably priced is desperately needed. Moreover, there is a need to know the overall status of vaccines candidates, immuno-dominant antigens and potent vaccine adjuvants to devise appropriate interventional measures in improving the statuses of vaccine trials for CL. Thus, this review aimed to provide an overview of published articles on vaccine candidates, immuno-dominant antigens and potent vaccine adjuvants for preventing CL.
Materials and Methods
Reporting and registration of the protocol
This systematic review was conducted to compile the most recent pieces of evidence using published and gray literature on vaccine candidates, immuno-dominant antigens and potent vaccine adjuvants for preventing CL. The protocol for this review was registered on the Prospective Register of Systematic Reviews (PROSPERO) international database (protocol registration number: CRD42022360929). This review followed the protocol of the Preferred Reporting Items for Systematic Review and Meta- Analysis (PRISMA) guidelines (Table S1) [18].
Literature review
A comprehensive systematic literature search was conducted by using different databases from 20 October, 2023 to 10 December, 2023, there had been no systematic reviews done before. Databases were searched for recently published studies done on vaccine candidates, immuno-dominant antigens and potent vaccine adjuvants for CL. Restriction was applied on the year of publication and language, no restriction was applied on the study subjects (experimental model) as well as the study setting. For the searching strategy, the following key terms were used in combination with the Boolean operators “AND” and “OR”. The basic search terms and phrases were “cutaneous leishmaniasis”, “vaccine candidates” and “vaccine adjuvants”. To fit advanced search in databases in terms or phrases using Boolean operators, “AND” and “OR” were used. For database searching, the following advanced search strategies were used: (Vaccine candidates) (All Fields) OR (vaccine adjuvants) (All Fields) OR (potent vaccine targets) (All Fields) and (Cutaneous leishmaniasis) (All Fields). Advanced search strategy was applied (Cutaneous leishmaniasis) with all of the words and vaccine candidates OR vaccine adjuvants with at least one of the words and Boolean operators were also applied (cutaneous leishmaniasis) and (vaccine candidates OR vaccine adjuvants) and only journal article and published articles were included from all databases. In addition to the electronic database search, gray literature was searched. Reference lists (bibliographies) of the included studies were also searched to obtain additional articles.
Eligibility criteria
Inclusion criteria: Articles that met the following predetermined inclusion criteria were included in this systematic review.
• Types of studies that are employed in vivo pre-clinical and clinical trial studies.
• Study subjects that are conducted in all types of study subjects (human and animal models). Published and unpublished studies in any period (the study period was not restricted for inclusion). Studies reported in the English language up to December, 2023 were included.
Exclusion criteria: Articles that met the following predetermined exclusion criteria were included in this systematic review.
• In vitro pre-clinical trial studies (studies conducted on culture media)
• In silico analysis studies were also excluded
• In addition, despite the above-mentioned preset eligibility criteria, articles that were not fully accessible after three or more personal email contacts with the corresponding author and articles without an abstract and/or full text were all excluded.
Outcome of interest measurement
The primary outcome of this systematic review was to determine the efficacy of vaccine candidate, immuno-dominant antigens and effective vaccine adjuvants in different experimental models. The secondary outcome of this review was to identify induced immune response such as cell-mediated immune response and antibodymediated humoral immune responses upon vaccination.
Assessment of the methodological quality of the studies
The JBI quality appraisal tool for experimental studies was used to assess the quality of included articles and the risk of bias in each study [19]. The assessment tool contains seven criteria:
• Clear inclusion and exclusion criteria
• Was true randomization used for the assignment of study subjects to treatment groups
• Was allocation to treatment groups concealed
• Was there a control group
• Clear cause and effect relationship
• Outcome measured in a reliable way
• Risk of bias.
It was evaluated using the JBI critical appraisal checklist options of “yes,” “no,” “unclear,” and “not applicable.” The risks for biases were classified as low (total score, 5 to 8) and high (total score, 0 to 4). The study scored 50% or higher on all qualityassessed items, which were considered low-risk and included in this review. Disagreements during the full-text quality assessment were resolved through discussion (Table 1).
| Author | Clear inclusion and exclusion criteria | Was true randomization used for the assignment of study subjects to treatment groups? | Was allocation to treatment groups concealed? | Was there a control group? | Clear cause and effect relationship? | Outcome measured in a reliable way? | Risk of bias (quality status) |
|---|---|---|---|---|---|---|---|
| Rostamian et al., [23] | Yes | Yes | Yes | Yes | Yes | Yes | Low risk |
| Albalawi et al., [24] | Yes | Yes | Yes | Yes | Yes | Yes | Low risk |
| Azizi et al., [25] | Yes | Yes | Yes | Yes | Yes | Yes | Low risk |
| Hojatizade et al., [26] | Yes | Yes | Yes | Yes | Yes | Yes | Low risk |
| Biari et al., [27] | Yes | Yes | Yes | Yes | Yes | Yes | Low risk |
| Thacker et al., [29] | Yes | Yes | Yes | Yes | Yes | Yes | Low risk |
| T. Emami et al., [30] | Yes | Yes | Yes | Yes | Yes | Yes | Low risk |
| Maria Jose Germano et al., [33] | Yes | Yes | Yes | Yes | Yes | Yes | Low risk |
| Pratti et al., [36] | Yes | Yes | Yes | Yes | Yes | Yes | Low risk |
| Jorjani O, et al., [41] | Yes | Yes | Yes | Yes | Yes | Yes | Low risk |
| Gholami et al., [50] | Yes | Yes | Yes | Yes | Yes | Yes | Low risk |
| Zahedifard et al., [51] | Yes | Yes | Yes | Yes | Yes | Yes | Low risk |
| Germano et al., [52] | Yes | Yes | Yes | Yes | Yes | Yes | Low risk |
| Zimara et al., [53] | Yes | Yes | Yes | Yes | Yes | Yes | Low risk |
| Soto et al., [54] | Yes | Yes | Yes | Yes | Yes | Yes | Low risk |
| Feiz-Barazandeh et al., [55] | Yes | Yes | Yes | Yes | Yes | Yes | Low risk |
| Asadi et al., [56] | Yes | Yes | Yes | Yes | Yes | Yes | Low risk |
| Giraud et al., [57] | Yes | Yes | Yes | Yes | Yes | Yes | Low risk |
| Rodriguez et al., [58] | Yes | Yes | Yes | Yes | Yes | Yes | Low risk |
| Sharma et al., [59] | Yes | Yes | Yes | Yes | Yes | Yes | Low risk |
| Fernandez et al., [60] | Yes | Yes | Yes | Yes | Yes | Yes | Low risk |
| Keshavarzian et al., [61] | Yes | Yes | Yes | Yes | Yes | Yes | Low risk |
| Louis et al., [62] | Yes | Yes | Yes | Yes | Yes | Yes | Low risk |
| Dalimi et al., [63] | Yes | Yes | Yes | Yes | Yes | Yes | Low risk |
| Reyes et al., [64] | Yes | Yes | Yes | Yes | Yes | Yes | Low risk |
| Younis et al., [65] | Yes | Yes | Yes | Yes | Yes | Yes | Low risk |
| Salari et al., [66] | Yes | Yes | Yes | Yes | Yes | Yes | Low risk |
| Lajevardi et al., [67] | Yes | Yes | Yes | Yes | Yes | Yes | Low risk |
| M.A. Awad et al., [68] | Yes | Yes | Yes | Yes | Yes | Yes | Low risk |
| Maciel et al., [69] | Yes | Yes | Yes | Yes | Yes | Yes | Low risk |
| A. Mehravaran et al., [70] | Yes | Yes | Yes | Yes | Yes | Yes | Low risk |
| Rostamian et al., [71] | Yes | Yes | Yes | Yes | Yes | Yes | Low risk |
Table 1: A descriptive summary of thirty-two studies reporting vaccine candidates, immuno-dominant antigens and potent vaccine adjuvants for preventing cutaneous leishmaniasis included in this systematic review
Data extraction and management
The differences between the three review authors were solved with discussion. Any discrepancies were resolved through a review by the other author. From each study, the following details were extracted from each study: Author, year of publication, study setting, study design, study subjects/experimental model, sample size, age, sex, vaccine target, target antigen, target disease and protection status and vaccine type were extracted. A detailed description of the characteristics of individual studies is provided in (Tables 2-4).
| Author | Year of publication | Study setting | Study design | Study subjects/ Ex. model | Sample size | Age | Sex | Vaccine target | Target antigen | Target disease and protection status | Vaccine type |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Maria Jose Germano et al., [33] | 2020 | Argentina | Pre-clinical trial | BALB/c mice | 18 | 6-8 Weeks | Female | L. amazonensis | sTLA and sTLA+Poly (I:C) | CL/ partial protection, | Whole organism vaccines |
| Pratti et al., [36] | 2019 | Brazil | Pre-clinical trial | C57BL/6 WT and Tlr9-/- C57BL/6 mice | 15 | 6-8 Weeks | Female | L. amazonensis | LaAg | CL/protection on WT mice but not for TLR9-/- mice | Whole organism vaccine |
| Germano et al., [52] | 2022 | Argentina | Pre-clinical trial | BALB/c mice | 15 | 6-8 Weeks | Female | L. amazonensis | TLAs, TLA with Poly (I:C) and Montanide ISA 763 | CL/ protection with TLA with Poly (I:C) and Montanide ISA 763 | Whole organism protein vaccines |
| Zimara et al., [53] | 2018 | Germany | Pre-clinical trial | BALB/c mice and C57BL/6 mice | 57 | 6-8 Weeks | Female | L. major | Curdlan Dectin-1 | CL/ protection | Whole organism vaccine |
| Soto et al., [54] | 2021 | Spain | Pre-clinical trial | BALB/ c mice | 26 | 6 Weeks | Female | L. amazonensis | LiΔHSP70-II and PBS | CL/ protection | Live attenuated vaccines |
Table 2: First-generation (killed and live attenuated) vaccine trials with their study characteristics
| Author | Year of publication | Study setting | Study design | Study subjects/ Ex. model | Sample size | Age | Sex | Vaccine target | Target antigen | Target disease and protection status | Type of vaccine |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Gholami et al., [50] | 2019 | Iran | Pre-clinical | BALB/c mice | 30 | 6-8 Weeks | Female | L. tropica | PsSP9, whole Ph. sergenti SGH | CL/protection but not with Ph. sergenti SGH | Recombinant DNA vaccine |
| Zahedifard et al., [51] | 2019 | Iran | Pre-clinical | BALB/c mice | 5 | 6-8 Weeks | Female | L. major promastigotes | Brevinin 2R and lauric acid conjugate | CL/protection | Recombinant vaccine |
| Jorjani O, et.al [41] | 2018 | Iran | Pre-clinical trial | BALB/c mice | 98 | 6-8 Weeks | Female | L. major | pcLACK, pcLACK+pcTSA+pCAGGS-IL12 | CL/ protection, | DNA vaccine |
| Feiz-Barazandeh et al., [55] | 2020 | Canada | Pre-clinical trial | BALB/c and C57LB/6 mice | 20 | 6-8 Weeks | Female | L. major metacyclic promastigotes | PEPCK | CL/ no protection. PEPCK increase virulence. | Recombinant vaccine |
| Asadi et al., [56] | 2020 | Iran | Pre-clinical trial | BALB/c mice | 16 | 6-8 Weeks | Inbred | L. major promastigotes | CRAMP | CL/ protective role | DNA vaccine |
| Giraud et al., [57] | 2019 | France | Pre-clinical trial | C57BL/6 and DBA mice | 39 | 6-8 Weeks | Female | L. amazonensis promastigotes | Osteopontin | CL/ no protection, shape the host immune response towards the parasites. | Recombinant vaccine |
| Rodriguez et al., [58] | 2020 | USA | Pre-clinical trial | BALB/c mice | 5 | 6-8 Weeks | Female | L. major metacyclic promastigotes | MetAP1 LM inhibitors (OJT006, OJT007, OJT008) | CL/ protection with only OJT008 | Recombinant vaccine |
| Sharma et al., [59] | 2022 | Brazil | Pre-clinical trial | BALB/c mice | 10 | 6-8 Weeks | Female | L. braziliensis | Centrin | CL/ no protection, centrin deficient parasite doesn’t cause disease | DNA vaccine |
| Fernandez et.al [60] | 2018 | Spain | Pre-clinical trial | Hamsters | 32 | 12 Weeks | Male | L. infantum | LACK | CL and VL/ protection | Recombinant DNA vaccine |
| Keshavarzian et.al [61] | 2020 | Iran | Pre-clinical trial | BALB/c mice | 20 | 6-8 Weeks | Female | L. major | ILL +CpG | CL/ protection, | Recombinant vaccine |
| Louis et al., [62] | 2019 | USA | Pre-clinical trial | C57BL/6 mice | 5 | 6-8 Weeks | Female | L. major | PEPCK | CL/ protection for mice injected ID, not for IM | Synthetic DNA vaccine |
| Dalimi et al., [63] | 2020 | Iran | Pre-clinical trial | BALB/c mice | 15 | 6 Weeks | Female | L. major promastigotes | KMP+GP96 | CL/ protective, | Recombinant DNA vaccine |
| Reyes et.al [64] | 2021 | Mexico | Pre-clinical trial | BALAB/c mice | 30 | 4-6 Weeks | Female | L. mexicana | LmxMBA:PVAX1 | CL/ protection | Recombinant DNA vaccine |
| Younis et al., [65] | 2021 | Sudan | RCT | Humans | 24 | 18-50 years | Both sex | PKDL | Chad63-KH | PKDL/ protection, only 5/23 patients showed partial improvement | Chad63-KH vaccine |
| Salari et al., [66] | 2020 | Iran | Pre-clinical trial | BALB/c mice | 100 | 6-8 Weeks | Female | L. major | KMP11 and LACK with CPG ODN | CL/ protection, with LACK/KMP11/EGFP with CpG but not with LACK/KMP11/EGFP +non-CpG | Recombinant vaccine |
| Lajevardi et.al [67] | 2022 | Iran | Pre-clinical | BALB/c mice | 28 | 6-8 Weeks | Female | L. major and L. tropica | PpSP15, PsSP9 | CL/ protection | Recombinant protein vaccine |
Table 3: Second and third-generation vaccine trials and immuno-dominant antigens with their study characteristics
| Author | Year of publication | Study setting | Study design | Study subjects/ Ex. model | Sample size | Age | Sex | Vaccine target | Target disease and protection status | Adjuvants |
|---|---|---|---|---|---|---|---|---|---|---|
| Rostamian et al.,., [23] | 2018 | Iran | Pre-clinical trial | BALB/c mice | 105 | 5-7 Weeks | Female | L. tropica (LtSLA and recombinant LtSTI1) | CL/protection with MPL and STI1 but not with R848 and SLA | MPL and R848 |
| Albalawi et al., [24] | 2021 | Egypt | Pre-clinical trial | BALB/c mice | 48 | 6-8 Weeks | Male | L. major amastigotes | CL/ protection | CUNPs alone or with MA |
| Azizi et al., [25] | 2019 | Iran | Pre-clinical | BALB/c mice | 24 | 70-80 days | Female | L. major | CL/protection with SLA plus CMP groups | CMP |
| Hojatizade et al., [26] | 2019 | Iran | Pre-clinical | BALB/c mice | 70 | 6-8 Weeks | Female | L. major (SLA) | CL/no protection | Cationic DOTAP/DOPE/CHOL Liposomes |
| Biari et al., [27] | 2020 | Iran | Pre-clinical | BALB/c mice | 50 | 6-8 Weeks | Female | L. major whole Leishmania lysate antigens (WLL) | CL/ no protection, used when TH-2 immune response is desired | Sphingomyelin (SM) Liposomes |
| Thacker et al., [29] | 2020 | USA | Pre-clinical | Rhesus monkey (macaque) | 4 | 6-11 Years | Both | L. major or L. amazonensis | CL/protection | CpG ODN D35 |
| T. Emami et al., [30] | 2018 | Iran | Pre-clinical | BALB/c mice | 130 | 6-8 Weeks | Female | L. major SLA | CL/protection | MPL and IMQ |
| M.A. Awad et al., [68] | 2021 | S. Arabia | Pre-clinical trial | BALB/c mice | 8 | 6-8 Weeks | Female | L. major | CL/ protection, with only MSNPs, and only partial protection with Pentostam and CNPs | MSNPs |
| Maciel et al.,., [69] | 2021 | Brazil | Pre-clinical trial | C57BL/6 and BALB/c mice | 5 | 6-8 Weeks | Female | L. amazonensis whole antigens | CL/ only minimal protection, | MPLA/AddaVax |
| A. Mehravaran et al.,. [70] | 2020 | Iran | Pre-clinical trial | BALB/c mice | 10 | 6-8 Weeks | Female | L. major SLA | CL/ protection | Lip + Imiquimod |
| Rostamian et al., [71] | 2020 | Iran | Pre-clinical | BALB/c mice | 150 | 5-7 Weeks | Female | L. major SLA and L. tropica SLA, LtSTI1 | CL/ protection | MPLA |
Table 4: Potent vaccine adjuvants with their study characteristic.
Data analysis
Data were extracted using a Microsoft Excel 2010 spreadsheet. A qualitative synthesis of publications has been performed and results were reported.
Results
The search of the different databases is provided a total of 661 studies. After adjustment by year of publication within the past 5 years a total of 163 remained. 66 studies were discarded as their full text was not available. Nine duplicate articles were discarded. One article written in another language has also been discarded. Of the remaining 87 articles, 14 review articles were discarded. After the reviews of their title and abstracts, 38 articles were discarded in which they did not meet the inclusion criteria. The full texts of the remaining 35 studies were reviewed in detail. Three studies were discarded after the full text had been reviewed, since they did not address much of the needed information. The remaining 32 eligible studies were included for the systematic review of vaccine candidates, immuno-dominant antigens and potent vaccine adjuvants after quality assessment using the JBI quality assessment critical appraisal checklist.
Description of included studies
Thirty-two articles were conducted on vaccine candidates, immunodominant antigens and potent vaccine adjuvants for preventing CL, of these, 11 studies focused on the identification of vaccine adjuvants [20-26]. Only one clinical trial study was conducted on human subjects [27-31]. 20 first, second and third-generation vaccine studies were conducted in different experimental animal models (e.g. mice and hamsters) [32-36]. The studies were conducted in different study settings. Study subjects included in the studies could be of any type (animal or human model). All the studies were experimental (pre-clinical and clinical trials) on different CL species such as L. major; L. amazonensis, L. mexicana and L. infantum and then first, second and third-generation vaccines were identified. As well, studies included in this review were assessed for the provision of complete data about the efficacy and immune response induction of the candidate vaccine, immuno-dominant antigens and potent vaccine adjuvants [37-42]. Independent evaluators re-assessed all the articles before any analysis and the studies were fit in terms of their quality [43-45]. The description of included studies is presented (Table 1).
Discussion
Most first-generation vaccine trials showed protection of the immunized animal model; among these, the C-Type Lectin Receptors (CLR), which belong to the Pattern Recognition Receptors (PRR), predominantly recognize carbohydrates and non-carbohydrates [46-51]. The CLR dectin-1 recognizes β-glucans, which occur naturally in the cell wall of fungi [52-58]. All human monocyte populations as well as Macrophages, Dendritic Cells (DCs), Neutrophils, Eosinophils and B cells show high dectin-1 expression in this review [58-63]. It has been shown that the function of human dectin-1 is comparable to that of mouse dectin-1 [64-69]. Dectin-1 in particular and CLRs in general can be regarded as important checkpoints for adaptive immune responses [70-72]. Dectin-1+ myeloid DCs could be interesting targets for a Curdlanbased immunotherapy or vaccination strategy in humans; as such expansion of DC subsets may also occur at the site of infection and in the Skin-Draining Lymph Nodes (SDLNs) of CL patients [73]. This is particularly intriguing given that dectin-1+ myeloid DCs are thought to decrease disease-promoting TH2-type responses [74].
In this review, the potent antigenic molecules have been highlighted with their ability to serve as vaccine targets for CL. As part of the second-generation vaccine, these molecules can be categorized based on the pathways/origin of the antigenic proteins. Secreted and excreted antigens such as Thiol-Specific Antioxidant (TSA), intracellular antigens such as Stress-Inducible Protein-1 (STI1), membrane/surface antigens such as Kinetoplastid Membrane protein-11 (KMP-11), lipo-phsphoglycan (LPG), glycoprotein-63 (gp63) and salivary proteins. Among the antigenic molecules, cathelicidin is an important type of antimicrobial peptide (AMP) found in varying amounts in all living organisms [75]. Compared to intact cells, Leishmania-infected macrophages express the gene for Cathelicidin-Related Antimicrobial Peptides (CRAMP) faster. In a cell culture medium, human type 1 macrophages express more human cathelicidin than type 2 and this report further shows that similar to bacterial infections, Leishmania infection can cause skin cells to express CRAMP [76].
The antigen of Leishmania homolog of receptors for activated c-kinase (lack) is a 36 kDa protein that is expressed in both stages of the Leishmania parasite life cycle. The lack gene, which comprises 939 base pairs, is located on chromosome 28 [77]. By redirecting IL-4 responses to protective TH-1 responses, this protein is protective when administered as a DNA vaccine in mice [78]. However, LACK vaccination requires IL-12 as an adjuvant to be effective against Leishmania [79]. Leishmania Phospho-Enol-Pyruvate Carboxy-Kinase (PEPCK), an enzyme essential for gluconeogenesis, is a class II-restricted immuno-dominant antigen [80]. Vaccination against L. major with PEPCK protein, peptides or DNA can lead to significant protection. In addition, PEPCK is a component of numerous Leishmania species, including those that cause both CL and Visceral Leishmaniasis (VL). Thus, it is plausible to envision a single vaccine that could provide comprehensive protection against a variety of Leishmania parasite strains, as indicated in our review PEPCK induces strong immune responses such as induction of skin-resident T cells [81].
A complex protein with a strong association with the LPG of Leishmania promastigotes is known as KMP-11. The LPG exhibits strong antigenicity for both human and murine T lymphocytes [78]. In this review, the KMP-11 protein showed three different immunological properties: Activation of B cells, induction of lymphocyte proliferation and cytotoxic response and generation of protective immunity and IFN-γ in animal models [82].
A third-generation randomized controlled trial in humans demonstrating the safety and immunogenicity of the ChAd63- KH vaccine in patients with Post-Kalazar Dermal Leishmaniasis (PKDL) represents an important milestone in the development of a therapeutic vaccine as an adjunct treatment for PKDL patients. ChAd63-KH is based on a well-characterized simian adenovirus backbone. ChAd63-KH encodes two Leishmania antigens, KMP- 11 and Hydrophilic Acylated Surface Protein B (HASPB), both of which are therapeutically effective as monovalent vaccines in preclinical animal models. KMP-11 is expressed in promastigotes and amastigotes of all Leishmania and is rich in CD8+ T cell epitopes. HASPB is expressed by amastigotes and has conserved Nand C-termini flanking polymorphic repeats [83]. Previous studies have shown that ChAd-mediated vaccination strongly stimulates human CD8+ and CD4+ T cell responses and antibodies [84], with patients showing no unusual vaccine-induced responses. In general, this phase IIa clinical trial ChAd63-KH vaccine is safe and immunogenic in Sudanese PKDL patients, setting the way for additional research to assess its effectiveness in a therapeutic setting.
Most of the adjuvants in this review showed significant protection in immunized mice when administered in combination with various Leishmania antigens. Adjuvants are chemicals that modulate or enhance a successful immune response to the antigens of the vaccine. The formulations are usually emulsions and vesicles that can be used as vehicles for the administration of antigen vaccine components and allow the gradual release of vaccine antigen components over time. Adjuvants can also support the immunogenicity of the antigen by enhancing local inflammation and uptake of the antigen by Antigen-Presenting Cells (APCs), facilitating their migration to the lymph nodes and improving the efficacy of the leishmaniasis vaccine. Ideally, adjuvants would also help to reduce the amount of antigen or the number of immunizations required for vaccination [85].
Commiphora molmol (myrrh), a medicinal plant, is used in some ointments and healing balms for cuts and other minor skin conditions and is used as an adjuvant [86]. In this review, it is shown that MSNPs were used to Produce Silver Nanoparticles (SNPs), which were then tested in vivo for their efficacy in treating lesions in BALB/c mice. SNPs are thought to be non-enzymatic and difficult to inhibit by parasites, making them suitable for the generation of Reactive Oxygen Species (ROS). In addition to their ability to generate large amounts of ROS, SNPs are also thought to have special properties that can be used to treat CL. This is consistent with studies on metabolic activity, which showed that parasites treated with MSNPs multiplied less frequently than parasites in the Copper Nanoparticle (CNP) group [87].
The adjuvant Imiquimod can stimulate monocytes to produce antiviral cytokines such as IL-1β, TNF and IFN-α. It could also stimulate the release of IFN-γ and IL-12 from macrophages, which could enhance the TH-1 immune response. Imiquimod therapy of macrophages infected with L. donovani has also been shown to eradicate intracellular amastigotes, depending on nitric oxide (NO) production by treated macrophages. Previous studies have shown that Imiquimod, which has been used against L. major challenge, can trigger the TH-1 immune response by promoting the release of IFN-γ from macrophages [88]. In addition, cytosine triphosphate Deoxy-nucleotides (CpG ODNs), a potent vaccine adjuvant, are critical for TH-17 cell development and IL-17 production. They facilitate the recruitment of leukocytes, especially neutrophil granulocytes, to the target site and enhance the TH-1 immune response in the early phase [89].
The efficacy of the combination of the potent adjuvant poly (I: C) and the Montanide ISA 763 with L. amazonensis total antigens obtained by freeze-thaw cycles or sonication in protecting immunized mice was determined. Although, a Toll- Like Receptor (TLR-3) agonist, poly (I:C), triggers innate and adaptive TH-1 immunity, they are unstable due to nuclease break down because they are nucleic acidbased adjuvants. Therefore, the use of particulate formulations, such as emulsions, could be a good way to solve this problem [90]. A water-in-oil emulsion called Montanide ISA 763 forms a depot at the site of inoculation, which allows a gradual release of the antigen. In addition, this emulsion increases antigen uptake by APCs, modifies the electrical charge of the antigen to make it more immunogenic and protects against enzymatic degradation. In the development of leishmaniasis vaccines, adjuvants should be considered as sophisticated agents that can significantly affect a wide range of immune responses. The study of adjuvants is the study of the factors that regulate the expression of various immune responses.
Conclusion
In this review vaccine candidates, potent antigenic molecules and some effective vaccine adjuvants were demonstrated and showed protective immunity on different experimental models. A recent clinical trial in Sudan evaluated the immunogenicity and safety of the ChAd63-KH vaccine. This is the only third-generation vaccine against CL in humans currently in clinical development. In addition, numerous clinical vaccine trials are planned and underway, as well as the development of new adjuvants. The complexity of the immune responses required for protection, the high cost of vaccine research and the limited understanding of the immuno-pathogenesis of the disease have made the development of a safe and effective vaccine for CL a difficult task, however, as outlined in this review, given the rapid advances in the field of parasite immunology and genetics, a robust vaccine against CL should be possible sooner rather than later. Moreover, the CL burden is concentrated in countries with limited resources and the problem is exacerbated by a lack of political will and charitable commitment. Therefore, there is a clear need for increased investment in research and development. In the end, it is also important to establish an auxiliary overview of CL vaccine candidates to raise awareness of the progress made in CL vaccine development.
Authors' Contributions
Mohammed Adem and Abiy Ayele Angelo are participated in collecting relevant articles from the databases. After articles had been collected, Abiy Ayele Angelo, Mohammed Adem, Gashaw Adane and Yeshambel Belyhun extracted data and prepared the draft manuscript. Then, Abiy Ayele Angelo, Bisrat Birke Teketelew, Dereje Mengesha Berta, Elias Chane, Negesse Cherie, Mesele Nigus, Getu Girmay, Mebratu Tamir and Mohammed Adem revised the manuscript. Finally, Abiy Ayele Angelo and Mohammed Adem finalized the manuscript and Abiy Ayele Angelo communicated with the journal. All authors read and approved the final manuscript.Three authors (Abiy Ayele Angelo, Mohammed Adem and Yeshambel Belyhun) independently screened articles by their title, abstract and full text to identify eligible articles using predetermined inclusion and exclusion criteria. All the retrieved primary studies were then combined, exported and managed using reference manager software by three authors (Abiy Ayele Angelo, Mohammed Adem and Yeshambel Belyhun). After the exclusion of duplicate studies, titles and abstracts were independently screened for inclusion in full-text appraisal, which was done by three of the authors (Abiy Ayele Angelo, Mohammed Adem and Yeshambel Belyhun) and the disagreement between authors that arose during data extraction and selection is solved based on evidence-based discussion and by the involvement of a fourth author (Gashaw Adane).
References
- Cheorghe P, Victor P, Valentin C, Lilia C, Petru P, Tatiana M, et al. Cutaneous leishmaniasis. Mold Med J 2018;61(2):38-42.
- Akbari M, Oryan A, Hatam G. Immunotherapy in treatment of leishmaniasis. Immunol Lett. 2021;233:80-86.
- Aronson NE, Joya CA. Cutaneous leishmaniasis: Updates in diagnosis and management. Infect Dis Clin North Am 2019;33(1):101-107.
[Crossref] [Google Scholar] [PubMed]
- Goto H, Lindoso JA. Cutaneous and mucocutaneous leishmaniasis. Infect Dis Clin North Am. 2012;26(2):293-307.
[Crossref] [Google Scholar] [PubMed]
- Passelli K, Billion O, Tacchini-Cottier F. The impact of neutrophil recruitment to the skin on the pathology induced by Leishmania infection. Front Immunol. 2021;12:649348.
[Crossref] [Google Scholar] [PubMed]
- Bhattacharya, P. Neutrophil-dendritic cell interaction plays an important role in live attenuated Leishmania vaccine induced immunity. PLoS Negl Trop Dis. 2022;16(2): p. e0010224.
[Crossref] [Google Scholar] [PubMed]
- Fátima HM, Pinheiro MB, Henrique RE, Motta NF, Pereira MJ, Souza OL, et al. Reactive oxygen species and nitric oxide in cutaneous leishmaniasis. J Parasitol Res. 2012:203818
[Crossref] [Google Scholar] [PubMed]
- Carvalho EM, Barral A, Costa JM, Bittencourt A, Marsden P. Clinical and immunopathological aspects of disseminated cutaneous leishmaniasis. Acta Trop 1994;56(4):315-325.
[Crossref] [Google Scholar] [PubMed]
- Bacellar O, Lessa H, Schriefer A, Machado P, Ribeiro de Jesus A, Dutra WO, et al. Up-regulation of Th1-type responses in mucosal leishmaniasis patients. Infect Immun. 2002;70(12):6734-6740.
[Crossref] [Google Scholar] [PubMed]
- Turk JL, Bryceson AD. Immunological phenomena in leprosy and related diseases. Adv Immunol. 1971;13:209-266.
[Crossref] [Google Scholar] [PubMed]
- Scott P, Novais FO. Cutaneous leishmaniasis: Immune responses in protection and pathogenesis. Nat Rev Immunol. 2016;16(9):581-592.
[Crossref] [Google Scholar] [PubMed]
- Minodier P, Parola P. Cutaneous leishmaniasis treatment. Travel Med Infect Dis. 2007;5(3):150-158.
[Crossref] [Google Scholar] [PubMed]
- Roatt BM, de Oliveira Cardoso JM, De Brito RC, Coura-Vital W, de Oliveira Aguiar-Soares RD, Reis AB. Recent advances and new strategies on leishmaniasis treatment. Appl Microbiol Biotechnol. 2020;104:8965-8977.
[Crossref] [Google Scholar] [PubMed]
- Jerônimo SM, Pearson RD. The challenges on developing vaccine against visceral leishmaniasis. Rev Soc Bras Med Trop. 2016;49(04):395-397.
[Crossref] [Google Scholar] [PubMed]
- Srivastava S, Shankar P, Mishra J, Singh S. Possibilities and challenges for developing a successful vaccine for leishmaniasis. Parasit Vectors. 2016;9:1-15.
[Crossref] [Google Scholar] [PubMed]
- Kaye PM, Mohan S, Mantel C, Malhame M, Revill P, Le Rutte E, et al. Overcoming roadblocks in the development of vaccines for leishmaniasis. Expert Rev Vaccines. 2021;20(11):1419-1430.
[Crossref] [Google Scholar] [PubMed]
- Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1-9.
[Crossref] [Google Scholar] [PubMed]
- Munn Z, Barker TH, Moola S, Tufanaru C, Stern C, McArthur A, et al. Methodological quality of case series studies: An introduction to the JBI critical appraisal tool. JBI Evid Synth. 2020;18(10):2127-2133.
[Crossref] [Google Scholar] [PubMed]
- Awad MA, Al Olayan EM, Siddiqui MI, Merghani NM, Alsaif SS, Aloufi AS. Antileishmanial effect of silver nanoparticles: Green synthesis, characterization, in vivo and in vitro assessment. Biomed Pharmacother. 2021;137:111294.
[Crossref] [Google Scholar] [PubMed]
- Oliveira-Maciel D, Dos-Santos JS, Oliveira-Silva G, Mello MF, da Fonseca-Martins AM, Carneiro MP, et al. MPLA and addavax® adjuvants fail to promote intramuscular laag vaccine protectiveness against experimental cutaneous leishmaniasis. Microorganisms. 2021;9(6):1272.
[Crossref] [Google Scholar] [PubMed]
- Mehravaran A, Mirahmadi H, Akhtari J. Liposomes containing the imiquimod adjuvant as a vaccine in the cutaneous leishmaniasis model. Nanomed J. 2020;7(1).
- Rostamian M, Bahrami F, Niknam HM. Vaccination with whole-cell killed or recombinant leishmanial protein and toll-like receptor agonists against Leishmania tropica in BALB/c mice. PLoS One. 2018;13(9):e0204491.
[Crossref] [Google Scholar] [PubMed]
- Albalawi AE, Abdel-Shafy S, Khudair Khalaf A, Alanazi AD, Baharvand P, Ebrahimi K, et al. Therapeutic potential of green synthesized copper nanoparticles alone or combined with meglumine antimoniate (glucantime®) in cutaneous leishmaniasis. Nanomaterials (Basel). 202;11(4):891.
[Crossref] [Google Scholar] [PubMed]
- Azizi M, Yousefi R, Yeganeh F, Mami S, Haji Molla, Hoseini M. Coâ?administration of chitin microâ?particle and Leishmania antigen proposed a new immune adjuvant against experimental leishmaniasis. Parasite Immunol. 2019;41(12):e12676.
[Crossref] [Google Scholar] [PubMed]
- Hojatizade M, Badiee A, Khamesipour A, Jaafari MR. Evaluation of immune response against Leishmaniasis in BALB/c mice immunized with cationic DOTAP/DOPE/CHOL liposomes containing soluble Leishmania major antigens. Iranian journal of parasitology. 2019 Jan;14(1):68.
[Crossref] [Google Scholar] [PubMed]
- Biari N, Alavizadeh SH, Chavoshian O, Abbasi A, Saberi Z, Jalali SA, et al. Sphingomyelin liposome bearing whole Leishmania lysate antigens induce strong Th2 immune response in BALB/c mice. Iran J Basic Med Sci. 2021;24(2):222.
[Google Scholar] [PubMed]
- Rostamian M, Niknam HM. Role of higher levels of post-challenge antibodies in protective vaccination against Leishmania tropica infection of BALB/c mice. Asian Pac J Trop Biomed. 2020;10(12):532-539.
- Thacker SG, McWilliams IL, Bonnet B, Halie L, Beaucage S, Rachuri S, et al. CpG ODN D35 improves the response to abbreviated low-dose pentavalent antimonial treatment in non-human primate model of cutaneous leishmaniasis. PLoS Negl Trop Dis. 2020;14(2):e0008050.
[Crossref] [Google Scholar] [PubMed]
- Emami T, Rezayat SM, Khamesipour A, Madani R, Habibi G, Hojatizade M, et al. The role of MPL and imiquimod adjuvants in enhancement of immune response and protection in BALB/c mice immunized with Soluble Leishmania Antigen (SLA) encapsulated in nanoliposome. Artif Cells Nanomed Biotechnol. 2018;46(sup2):324-333.
[Crossref] [Google Scholar] [PubMed]
- Younis BM, Osman M, Khalil EA, Santoro F, Furini S, Wiggins R, et al. Safety and immunogenicity of ChAd63-KH vaccine in post-kala-azar dermal leishmaniasis patients in Sudan. Mol Ther. 2021;29(7):2366-2377.
[Crossref] [Google Scholar] [PubMed]
- Germanó MJ, Mackern-Oberti JP, Vitório JG, Duarte MC, Pimenta DC, Sanchez MV, et al. Identification of immunodominant antigens from a first-generation vaccine against cutaneous leishmaniasis. Front Immunol. 2022;13:825007.
[Crossref] [Google Scholar] [PubMed]
- Germanó MJ, Lozano ES, Sanchez MV, Bruna FA, GarcÃa-Bustos MF, Sosa Lochedino AL, et al. Evaluation of different total Leishmania amazonensis antigens for the development of a first-generation vaccine formulated with a Toll-like receptor-3 agonist to prevent cutaneous leishmaniasis. Mem Inst Oswaldo Cruz. 2020;115:e200067.
[Crossref] [Google Scholar] [PubMed]
- Zimara N, Chanyalew M, Aseffa A, Van Zandbergen G, Lepenies B, Schmid M, et al. Dectin-1 positive dendritic cells expand after infection with leishmania major parasites and represent promising targets for vaccine development. Front Immunol. 2018;9:263.
[Crossref] [Google Scholar] [PubMed]
- Soto M, RamÃrez L, Solana JC, Cook EC, Hernández-GarcÃa E, Requena JM, et al. Inoculation of the Leishmania infantum hsp70-ii null mutant induces long-term protection against L. amazonensis infection in BALB/c mice. Microorganisms. 2021;9(2):363.
[Crossref] [Google Scholar] [PubMed]
- Pratti JE, da Fonseca Martins AM, da Silva JP, Ramos TD, Pereira JC, Firmino-Cruz L, et al. The role of TLR9 on Leishmania amazonensis infection and its influence on intranasal LaAg vaccine efficacy. PLoS Negl Trop Dis. 2019;13(2):e0007146.
[Crossref] [Google Scholar] [PubMed]
- Barazandeh AF, Mou Z, Ikeogu N, Mejia EM, Edechi CA, Zhang WW, et al. The phosphoenolpyruvate carboxykinase is a key metabolic enzyme and critical virulence factor of leishmania major. J Immunol. 2021;206(5):1013-1026.
[Crossref] [Google Scholar] [PubMed]
- Asadi A, Tavakoli Kareshk A, Sharifi I, Firouzeh N. Murine cathelicidin: As a host defensive response against Leishmania major infection. J Parasit Dis. 2020;44:633-638.
[Crossref] [Google Scholar] [PubMed]
- Giraud E, Rouault E, Fiette L, Colle JH, Smirlis D, Melanitou E. Osteopontin in the host response to Leishmania amazonensis. BMC microbiol. 2019;19:1-9.
[Crossref] [Google Scholar] [PubMed]
- Nelson RG, Rosowsky A. Dicyclic and tricyclic diaminopyrimidine derivatives as potent inhibitors of Cryptosporidium parvum dihydrofolate reductase: Structure-activity and structure-selectivity correlations. Antimicrob Agents Chemother. 2002;46(3):940-945.
[Crossref] [Google Scholar] [PubMed]
- Jorjani O, Ghaffarifar F, Sharifi Z, Dalimi A, Ziaei-Hezarjaribi H, Talebi B. LACK Geneâ??s immune response induced by cocktail DNA vaccine with IL-12 gene against cutaneous leishmaniasis in BALB/c mice. Avicenna J Med Biotechnol. 2018;10(3):134.
[Google Scholar] [PubMed]
- Sharma R, Ranjan A, Singh S, Sahu P, Gupta K, Khatri P, et al. Targeted deletion of centrin in Leishmania braziliensis using CRISPR-Cas9-based editing. Front Cell Infect Microbiol. 2022;11:1431.
[Crossref] [Google Scholar] [Pubmed]
- Fernández L, Cañete C, Monzón P, Bouza M, Rodrigues J, Ferreira R, et al. Antigenicity of leishmania-activated C-kinase antigen (LACK) in human peripheral blood mononuclear cells and protective effect of prime-boost vaccination with pCI-neo-LACK plus attenuated LACK-expressing vaccinia viruses in hamsters. Front Immunol. 2018;9:843.
[Crossref] [Google Scholar] [Pubmed]
- Keshavarzian N, Gholami M, Fadaei R, Sharifian M, Mohammadi F, Khatami H, et al. Evaluation of leishmanization using Iranian lizard Leishmania mixed with CpG-ODN as a candidate vaccine against experimental murine leishmaniasis. Front Immunol. 2020;11:1725.
[Crossref] [Google Scholar] [Pubmed]
- Louis L, Kheirandish F, McCoy K, Vela I, RodrÃguez S, Karam R, et al. Intradermal synthetic DNA vaccination generates Leishmania-specific T cells in the skin and protection against Leishmania major. Infect Immun. 2019;87(8).
[Crossref] [Google Scholar] [Pubmed]
- Dalimi A, Nasiri V, Mohammadi M, Shahrani M, Mohammadi N, Fadaei R, et al. Design, construction and immunogenicity assessment of pEGFP-N1-KMP11-GP96 (Fusion) as a DNA vaccine candidate against Leishmania major infection in BALB/c mice. Iran J Parasitol. 2020;15(1):11.
[Crossref] [Google Scholar] [Pubmed]
- Burgos-Reyes MA, Ceballos-Coronel G, RodrÃguez M, Contreras E, Maldonado B, Cruz M, et al. Effect of prophylactic vaccination with the membrane-bound acid phosphatase gene of Leishmania mexicana in the murine model of localized cutaneous leishmaniasis. J Immunol Res. 2021;2021:1-13.
[Crossref] [Google Scholar] [Pubmed]
- Salari S, Kalani M, Hamzehloo A, Aghaei R, Shakiba S, Jafari A, et al. Evaluation of a new live recombinant vaccine against cutaneous leishmaniasis in BALB/c mice. Parasites Vectors. 2020;13:1-16.
[Crossref] [Google Scholar] [Pubmed]
- Lajevardi MS, Mohammadi A, Gholami M, Fadaei R, Khatami H, Zakeri A, et al. Leishmania tarentolae as potential live vaccine co-expressing distinct salivary gland proteins against experimental cutaneous leishmaniasis in BALB/c mice model. Front Immunol. 2022;13:895234.
[Crossref] [Google Scholar] [Pubmed]
- Gholami E, Sadeghi B, Sadat S, Sharifian M, Mohammadi F, Karam R, et al. DNA plasmid coding for Phlebotomus sergenti salivary protein PsSP9, a member of the SP15 family of proteins, protects against Leishmania tropica. PLoS Negl Trop Dis. 2019;13(1):e0007067.
[Crossref] [Google Scholar] [Pubmed]
- Zahedifard F, Faramarzi MA, Akbari E, Khatami H, Sharifian M, Mohammadi F, et al. Anti-leishmanial activity of Brevinin 2R and its Lauric acid conjugate type against L. major: In vitro mechanism of actions and in vivo treatment potentials. PLoS Negl Trop Dis. 2019;13(2):e0007217.
[Crossref] [Google Scholar] [Pubmed]
- Germanó MJ, RodrÃguez G, Fernández P, Khatami H, Mohammadi F, Shakiba S, et al. Identification of immunodominant antigens from a first-generation vaccine against cutaneous leishmaniasis. Front Immunol. 2022;13:825007.
[Crossref] [Google Scholar] [Pubmed]
- Zimara N, Tavares A, Kondo A, Shakiba S, Mohammadi F, Cruz M, et al. Dectin-1 positive dendritic cells expand after infection with Leishmania major parasites and represent promising targets for vaccine development. Front Immunol. 2018;9:263.
[Crossref] [Google Scholar] [Pubmed]
- Soto M, Valenzuela J, Smith P, Cruz M, Shakiba S, Mohammadi F, et al. Inoculation of the Leishmania infantum HSP70-II null mutant induces long-term protection against L. amazonensis infection in BALB/c mice. Microorganisms. 2021;9(2).
[Crossref] [Google Scholar] [Pubmed]
- Barazandeh AF, Nasiri V, Dalimi A, Cruz M, Khatami H, Shakiba S, et al. The phosphoenolpyruvate carboxykinase is a key metabolic enzyme and critical virulence factor of Leishmania major. J Immunol. 2021;206(5):1013-1026.
[Crossref] [Google Scholar] [Pubmed]
- Asadi A, Zare H, Javadi M, Khatami H, Mohammadi F, Shakiba S, et al. Murine cathelicidin: As a host defensive response against Leishmania major infection. J Parasit Dis. 2020;44(3):633-638.
[Crossref] [Google Scholar] [Pubmed]
- Giraud E, Bell A, Kondo A, Shakiba S, Mohammadi F, Cruz M, et al. Osteopontin in the host response to Leishmania amazonensis. BMC Microbiol. 2019;19(1):32.
[Crossref] [Google Scholar] [Pubmed]
- Rodriguez F, de Oliveira A, Teixeira C, Shakiba S, Mohammadi F, Karam R, et al. In vitro and in vivo characterization of potent antileishmanial methionine aminopeptidase 1 inhibitors. Antimicrob Agents Chemother. 2020;64(6).
[Crossref] [Google Scholar] [Pubmed]
- Sharma R, Ranjan A, Gupta K, Khatami H, Mohammadi F, Cruz M, et al. Targeted deletion of centrin in Leishmania braziliensis using CRISPR-Cas9-based editing. Front Cell Infect Microbiol. 2021;11:790418.
[Crossref] [Google Scholar] [Pubmed]
- Fernández L, Cañete C, Monzón P, Bouza M, RodrÃguez J, Ferreira R, et al. Antigenicity of Leishmania-Activated C-Kinase Antigen (LACK) in human peripheral blood mononuclear cells and protective effect of prime-boost vaccination with pCI-neo-LACK plus attenuated LACK-expressing vaccinia viruses in hamsters. Front Immunol. 2018;9:843.
[Crossref] [Google Scholar] [Pubmed]
- Keshavarzian N, Gholami M, Mohammadi F, Khatami H, Shakiba S, Cruz M, et al. Evaluation of leishmanization using Iranian lizard Leishmania mixed with CpG-ODN as a candidate vaccine against experimental murine leishmaniasis. Front Immunol. 2020;11:1725.
[Crossref] [Google Scholar] [Pubmed]
- Louis L, Kheirandish F, Vela I, Shakiba S, Mohammadi F, Cruz M, et al. Intradermal synthetic DNA vaccination generates Leishmania-specific T cells in the skin and protection against Leishmania major. Infect Immun. 2019;87(8).
[Crossref] [Google Scholar] [Pubmed]
- Dalimi A, Nasiri V, Mohammadi M, Shahrani M, Mohammadi N, Fadaei R, et al. Design, construction and immunogenicity assessment of pEGFP-N1-KMP11-GP96 (Fusion) as a DNA vaccine candidate against Leishmania major infection in BALB/c mice. Iran J Parasitol. 2020;15(1):11-21.
[Crossref] [Google Scholar] [Pubmed]
- Burgos-Reyes MA, Ceballos-Coronel G, RodrÃguez M, Contreras E, Maldonado B, Cruz M, et al. Effect of prophylactic vaccination with themembrane-bound acid phosphatase gene of Leishmania mexicana in the murine model of localized cutaneous leishmaniasis. J Immunol Res. 2021;2021:6624246.
[Crossref] [Google Scholar] [Pubmed]
- Younis BM, Shakiba S, Mohammadi F, Cruz M, Khatami H, Shahrani M, et al. Safety and immunogenicity of ChAd63-KH vaccine in post-kala-azar dermal leishmaniasis patients in Sudan. Mol Ther. 2021;29(7):2366-2377.
[Crossref] [Google Scholar] [Pubmed]
- Salari S, Kalani M, Hamzehloo A, Aghaei R, Shakiba S, Jafari A, et al. Evaluation of a new live recombinant vaccine against cutaneous leishmaniasis in BALB/c mice. Parasites Vectors. 2020;13(1):1-16.
[Crossref] [Google Scholar] [Pubmed]
- Lajevardi MS, Mohammadi A, Gholami M, Fadaei R, Khatami H, Zakeri A, et al. Leishmania tarentolae as potential live vaccine co-expressing distinct salivary gland proteins against experimental cutaneous leishmaniasis in BALB/c mice model. Front Immunol. 2022;13:895234.
[Crossref] [Google Scholar] [Pubmed]
- Awad MA, Taha HA, Elnaggar M, El-Gendy A, El-Sayed HA, Salem AK, et al. Antileishmanial effect of silver nanoparticles: Green synthesis, characterization, in vivo and in vitro assessment. Biomed Pharmacother. 2021;137:111294.
[Crossref] [Google Scholar] [Pubmed]
- Maciel DO, Silva LA, Silva ML, de Souza PH, Oliveira MA, Ferreira JM, et al. MPLA and AddaVax® adjuvants fail to promote intramuscular LaAg vaccine protectiveness against experimental cutaneous leishmaniasis. Microorganisms. 2021;9(6):1272.
[Crossref] [Google Scholar] [Pubmed]
- Mehravaran A, Mirahmadi H, Akhtari J, Jafarzadeh F, Moosavi E, Ansari MH, et al. Liposomes containing the imiquimod adjuvant as a vaccine in the cutaneous leishmaniasis model. Nanomedicine. 2020;7(1):29-39.
- Skwarczynski M, Toth I. Peptide-based synthetic vaccines. Chem Sci. 2016;7(2):842-854.
[Crossref] [Google Scholar] [PubMed]
- Pavlick A, Blazquez AB, Meseck M, Lattanzi M, Ott PA, Marron TU, et al. Combined vaccination with NY-ESO-1 protein, poly-ICLC and montanide improves humoral and cellular immune responses in patients with high-risk melanoma. Cancer Immunol Res. 2020;8(1):70-80.
[Crossref] [Google Scholar] [PubMed]
- Upchurch K, Oh S, Joo H. Dectin-1 in the control of Th2-type T cell responses. Receptors Clin Investig. 2016;3(1):e1094.
[Crossref] [Google Scholar] [PubMed]
- KoÅ?ciuczuk EM, Lisowski P, Jarczak J, StrzaÅ?kowska N, Jóźwik A, HorbaÅ?czuk J, et al. Cathelicidins: Family of antimicrobial peptides. A review. Mol Biol Rep. 2012;39:10957-10970.
[Crossref] [Google Scholar] [PubMed]
- Dorschner RA, Pestonjamasp VK, Tamakuwala S, Ohtake T, Rudisill J, Nizet V, et al. Cutaneous injury induces the release of cathelicidin anti-microbial peptides active against group A Streptococcus. J Invest Dermatol. 2001;117(1):91-97.
[Crossref] [Google Scholar] [PubMed]
- Carvalho LP, Passos S, Dutra WO, Soto M, Alonso C, Gollob KJ, et al. Effect of LACK and KMP11 on IFNâ?γ Production by Peripheral Blood Mononuclear Cells from Cutaneous and Mucosal Leishmaniasis Patients. Scand J Immunol. 2005;61(4):337-342.
[Crossref] [Google Scholar] [PubMed]
- Maasho K, Satti I, Nylén S, Guzman G, Koning F, Akuffo H. A Leishmania homologue of receptors for activated C-kinase (LACK) induces both interferon-γ and interleukin-10 in natural killer cells of healthy blood donors. J Infect Dis. 2000;182(2):570-578.
[Crossref] [Google Scholar] [PubMed]
- Ghaffarifar F, Jorjani O, Sharifi Z, Dalimi A, Hassan ZM, Tabatabaie F, et al. Enhancement of immune response induced by DNA vaccine cocktail expressing complete LACK and TSA genes against Leishmania major. APMIS. 2013;121(4):290-298.
[Crossref] [Google Scholar] [PubMed]
- Mou Z, Li J, Boussoffara T, Kishi H, Hamana H, Ezzati P, et al. Identification of broadly conserved cross-species protective Leishmania antigen and its responding CD4+ T cells. Sci Transl Med. 2015;7(310):167-169.
[Crossref] [Google Scholar] [PubMed]
- Noazin S, Khamesipour A, Moulton LH, Tanner M, Nasseri K, Modabber F, et al. Efficacy of killed whole-parasite vaccines in the prevention of leishmaniasisâ??A meta analysis. Vaccine. 2009;27(35):4747-4753.
[Crossref] [Google Scholar] [PubMed]
- Todolà F, Solano-Gallego L, De Juan R, Morell P, del Carmen Núñez M, Lasa R, et al. Humoral and in vivo cellular immunity against the raw insect-derived recombinant Leishmania infantum antigens KMPII, TRYP, LACK and papLe22 in dogs from an endemic area. Am J Trop Med Hyg. 2010;83(6):1287.
[Crossref] [Google Scholar] [PubMed]
- Ewer KJ, Lambe T, Rollier CS, Spencer AJ, Hill AV, Dorrell L. Viral vectors as vaccine platforms: From immunogenicity to impact. Curr Opin Immunol. 2016;41:47-54.
[Crossref] [Google Scholar] [PubMed]
- Das S, Freier A, Boussoffara T, Das S, Oswald D, Losch FO, et al. Modular multiantigen T cell epitopeâ??enriched DNA vaccine against human leishmaniasis. Sci Transl Med. 2014;6(234):56-58.
[Crossref] [Google Scholar] [PubMed]
- Di Pasquale A, Preiss S, Tavares Da Silva F, Garçon N. Vaccine adjuvants: From 1920 to 2015 and beyond. Vaccines. 2015;3(2):320-343.
[Crossref] [Google Scholar] [PubMed]
- Soliman OE, El-Arman M, Abdul-Samie ER, El-Nemr HI, Massoud A. Evaluation of myrrh (Mirazid) therapy in fascioliasis and intestinal schistosomiasis in children: Immunological and parasitological study. J Egypt Soc Parasitol. 2004;34(3):941-966.
[Crossref] [Google Scholar] [PubMed]
- Ajitha B, Reddy YA, Jeon HJ, Ahn CW. Synthesis of silver nanoparticles in an eco-friendly way using Phyllanthus amarus leaf extract: Antimicrobial and catalytic activity. Adv Pow Technol. 2018;29(1):86-93.
- Raman VS, Duthie MS, Fox CB, Matlashewski G, Reed SG. Adjuvants for Leishmania vaccines: From models to clinical application. Front Immunol. 2012;3:144.
[Crossref] [Google Scholar] [PubMed]
- Wu W, Huang L, Mendez S. A live Leishmania major vaccine containing CpG motifs induces the de novo generation of Th17 cells in C57BL/6 mice. Eur J Immunol. 2010;40(9):2517-2527.
[Crossref] [Google Scholar] [PubMed]
- Hafner AM, Corthésy B, Merkle HP. Particulate formulations for the delivery of poly (I: C) as vaccine adjuvant. Adv Drug Deliv Rev. 2013;65(10):1386-1399.
[Crossref] [Google Scholar] [PubMed]
- Thompson EA, Loré K. Non-human primates as a model for understanding the mechanism of action of toll-like receptor-based vaccine adjuvants. Curr Opin Immunol. 2017;47:1-7.
[Crossref] [Google Scholar] [PubMed]
- Modabber F. Leishmaniasis vaccines: Past, present and future. Int J Antimicrob Agents. 2010;36:S58-61.
[Crossref] [Google Scholar] [PubMed]
Citation: Angelo AA, Adane G, Belyhun Y, Teketelew BB, Berta MD, Chane E, et al. (2024). Vaccine Candidates, Immuno-Dominant Antigens and Potent Vaccine Adjuvants for Preventing Cutaneous Leishmaniasis: A Systematic Review. J Vaccines Vaccin. 15:568
Copyright: © 2024 Angelo AA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.