Citations : 2345
Dentistry received 2345 citations as per Google Scholar report
Indexed In
- Genamics JournalSeek
- JournalTOCs
- CiteFactor
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- Directory of Abstract Indexing for Journals
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Mini Review - (2024) Volume 14, Issue 4
Update on the Efficacy of the Dermal Apron Technique: Increasing Peri-Implant Mucosal Thickness and Tissue Stabili
Barry P. Levin*Received: 16-Dec-2024, Manuscript No. DCR-24-27798; Editor assigned: 18-Dec-2024, Pre QC No. DCR-24-27798 (PQ); Reviewed: 02-Jan-2025, QC No. DCR-24-27798; Revised: 09-Jan-2025, Manuscript No. DCR-24-27798 (R); Published: 16-Jan-2025, DOI: 10.35248/2161-1122.24.14.704
Abstract
Beyond immediate implant placement, including implant selection, position and prosthetic connection, measures to counter negative hard and soft tissue changes associated with toot-extraction are critical to achieving long-term stability of health and esthetics. This often includes bone grafting and soft tissue augmentation. Particulate bone allografts, xenografts, alloplasts and combinations are often inserted within the “gap” between the inner facial wall of extraction sockets and the implant. Further research advocates placing bone grafts not only within this “bone zone”, but also within the “soft tissue zone” between the inner lining of the soft tissue sulcus and the anatomically formed provisional restoration or custom healing abutment. This method of grafting is referred to as “dual zone” bone grafting. Implementing dual zone bone grafting techniques can better preserve ridge dimensions and produce greater soft tissue volume compared to non-grafted controls. Addition of soft tissue grafts, often of autogenous origins can further improve esthetics and preserve peri-implant, marginal bone levels. Another technique, the dermal apron technique® utilizing allogeneic dermis as an alternative to autogenous, intra-oral soft tissue, reduces morbidity, treatment time and costs. The dermal apron technique® also includes the use of a dual zone bone graft, consisting of 80% mineralized bone allograft and 20% bone xenograft. This procedure has demonstrated comparable soft tissue thickness to sub-epithelial, connective tissue grafts. Multiple comparative studies demonstrate the advantages of the dermal apron technique® over non-grafted controls and equivalence to autogenous grafts in this regard.
Keywords
Immediate implant placement; Dermal allograft; Esthetics; Dermal apron technique®
Introduction
The dermal apron technique® was first introduced in 2016. The procedure was born of difficulties associated with achieving predictable, stable outcomes of esthetic and physiologic stability of peri-implant hard and soft tissues. The historic transition of immediate implant placement and provisionalization from a more invasive procedure, including reflection of full thickness flaps and more traditional membrane incorporation to a flapless technique is critical for improved results. Though less invasive, this involves a meticulous procedure, including preservation of the thin facial bone, often associated with maxillary anterior teeth, during extraction. Bone augmentation is confined to “internal” grafting, within the confines of the extraction socket. Soft tissue grafting is also more technique sensitive, without the advantage of flap elevation to more easily position soft tissue grafts on the facial aspect of the socket wall and implant/ abutment surfaces. It has been demonstrated in human and animal studies, that immediate implant placement alone in inadequate in terms of preventing dynamic negative changes such as gingival margin height and facial-palatal ridge dimensions. The goal of achieving adequate facial bone and soft tissue thickness is critical for the long term stability of peri- implant hard and soft tissues. This strategy implements both bone and mucosal augmentation, performed simultaneous with immediate implant placement and temporization, known as “Immediate Tooth-Replacement Therapy” or ITRT. Most commonly, various particulate bone grafts obturate the “gap” between the palatal positioned implant and autogenous, sub- epithelial, connective tissue grafts. Though highly-successful, there are incidences of graft failure and morbidity associated with this step. Harvesting of autogenous mucosal grafts also increases treatment time and costs for the patient. An alternative to this step is the utilization of a dermal graft of allogeneic origin. The graft, composed of sub-epidermal connective tissue, with a uniform thickness of 0.4-0.8 mm. It can be trimmed to accommodate the individual site and easily adapted between the overlying mucosa and the bone graft within the soft tissue zone.
Literature Review
Immediate placement of dental implants into fresh extraction sockets presents several challenges, especially in esthetically critical sites. These anterior teeth often present with thin (approximately 1.0 mm) soft tissues [1]. Increasing the volume of peri-implant mucosa is one goal of implant therapy. It has been demonstrated over the past several decades, that radiographic levels of marginal bone and alveolar ridge dimensions are better preserved in the presence of robust mucosal dimensions compared to sites exhibiting thin (0.2 mm) soft tissues [2,3]. Speculation relates this phenomenon to establishment of a supra-crestal biologic width or supra-crestal, soft tissue dimension, occurring in a more coronal position related to the implant platform and implant-abutment junction. In sites with thin mucosa, it is theorized that marginal bone will physiologically remodel to a more apical location to compensate for the re-establishment of 3-5 mm of supra-crestal, soft tissue dimensions.
For these reasons, a strategies geared towards increasing the peri- implant mucosal volume, as early as possible in the course of active therapy, are advocated [4,5]. Though several studies consider autogenous, connective tissue grafts as the “gold standard” for increasing soft tissue thickness, this technique is associated with increased morbidity, operation time and risk of complications [6].
Another advantage of the presence of thicker peri-implant mucosa is the esthetic improvement, compared to sites with thinner soft tissue. Animal and human studies have demonstrated the efficacy of thicker soft tissue preventing esthetic compromise due to color changes induced by the “shine through” of metallic and ceramic abutments visualized through thinner mucosa [7]. Evidence indicates that a minimal soft tissue thickness of 2-3 mm is necessary to prevent these negative color changes.
A novel technique, the dermal apron technique®, introduced by the author in 2016, combines immediate implant therapy with a dual-zone bone grafting technique and soft tissue augmentation utilizing a dermal allograft with a thickness of 0.4-0.8 mm in place of autogenous connective tissue grafts, reduces post- operative discomfort, treatment time and costs [8]. A comparative clinical study, comparing the dermal apron technique® to historical controls consisting of similar ITRT without any hard of soft tissue grafting demonstrated significantly thicker peri-implant mucosal (2.81 mm vs. 2.10 mm) [9]. Two subsequent studies evaluated the identical technique, with the only variable between the studies being the use of a bone level implant with a built-in, Sub-Crestal prosthetic Angle Correction (SAC) [10,11]. Interestingly, the thickness of the peri- implant mucosa, measured 2.0 mm apical to the facial gingival margin, increased approximately one millimeter in sites receiving SAC implants compared to the uniaxial implants placed in Part I of the series, with both SAC cohorts achieving average soft tissue thickness over 3.70 mm, compared to 2.81 mm for the sites receiving uniaxial implants. This would indicate a synergistic relationship between SAC implants and the dermal apron technique® in terms of increasing soft tissue volume. It is important to note, that SAC implants feature a greater disparity in the implant platform-abutment connection or platform switch, known as Variable Platform Switching (VPS).
Discussion
The dermal apron technique consists of several key steps being followed during the surgical phase of ITRT. First, following careful, flapless tooth extraction and socket debridement, implant placement is performed with a palatal bias within the extraction socket (Figure 1). This insures maximum engagement of apical, palatal and proximal bone while avoiding apical socket perforation of the facial cortex. The long-axis of the implant trajectory is that of the incisal edge of the planned restoration. The SAC component of the implant therefore insures a cingulum position of the abutment screw channel, negating the need for Angle Correcting (ASC) abutments. Dual zone bone grafting as described by Chu et al., is performed with the modification of including approximately 20% xenograft with the 80% mineralized bone allograft [4] (Figure 2). Provisionalization is then performed via screw-retention and a dermal allograft is trimmed and pierced with a sharp circular biopsy punch (Figure 3). This allows the dermal allograft to be adapted around the abutment portion of the one-piece, screw- retained provisional crown.
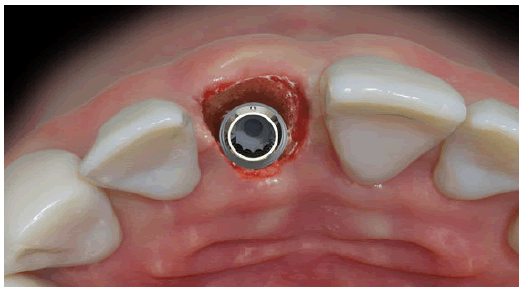
Figure 1: Implant with sub-crestal angle correction placed with a palatal bias in a central incisor and extraction socket.
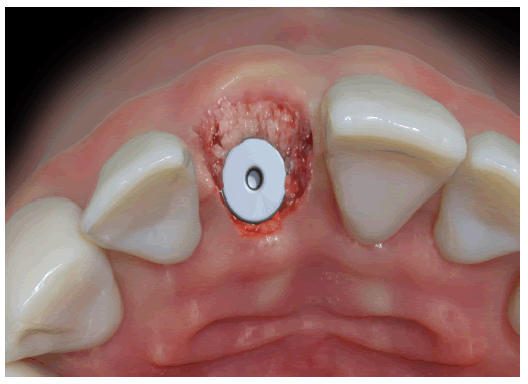
Figure 2: Composite particulate bone graft consisting of 80% cortical/cancellous bone allograft and 20% xenograft. The graft is gently placed into the bone zone of the extraction socket and in the tissue Czone ranging from the crestal bone to the gingival margin.

Figure 3: Dermal allograft hydrated in sterile saline for 5 min and then trimmed with a round opening created with a biopsy punch.
The basement membrane side of the dermal allograft is oriented in a manner where it will be placed in direct contact with the particulate bone graft in the tissue zone and the facial, osseous cortex approximately 3-5 mm apical to the facial crest. The lamina propria side of the dermis is oriented such that if will be in direct contact with the periosteum of the gently reflected coronal gingiva (Figure 4). Conceptually, this orientation should allow for rapid incorporation of the more porous side of the dermal allograft into the surrounding mucosa, though this is empirical. After tightening of the abutment screw and radiographic confirmation of the complete seating of the temporary crown, a monofilament, resorbable 5-0 suture (Monocryl, Ethicon) is placed in a horizontal mattress configuration [12-15].

Figure 4: Dermal allograft adapted around the abutment portion of the screw-retained, provisional crown. The basement membrane side is upwards, to be placed against the facial coronal cortex and lamina propria facing the crown will be oriented against the periosteum of the coronal soft tissue.
Conclusion
Many factors contribute to successful ITRT. Case selection, implant selection, biomaterials and surgical technique are all critical to achieving long-lasting success. The palatal positioning of the implant, geared towards preserving a “gap” of several millimeters between the facial implant surface and the inner wall of the extraction socket is critical. This strategy facilitates placement of biomaterials within this gap, to preserve horizontal and vertical ridge dimensions. Achieving primary implant stability allows for opportunity to place provisional restorations at the time of immediate implant placement. This often necessitates using a wide diameter implant. Wider, tapered implants are more capable of achieving primary stability. Unfortunately, wider implants occupy a significantly greater portion of the extraction socket, with proximity of the implant platform to the thin facial cortex. This would seem counterintuitive to the goal of preserving the “gap” and inhibiting the placement of bone allograft within the gap. Narrower implants better respect this strategy, but at the expense of achieving higher levels of primary stability. These challenges have been answered by utilizing an implant with an Inverted Body Design (IBDD). The author has demonstrated the efficacy of this implant design circumventing the challenges of preserving the peri-implant gap and achieving high levels of primary stability. Management of the hard and soft tissues, with a goal of tissue preservation and augmentation counters significant diminutive changes in the alveolus post-extraction. Increasing the thickness of peri-implant soft tissues enhances hard tissue levels and esthetic outcomes. The “gold standard” for soft tissue augmentation in dentistry is the autogenous, sub-epithelial connective tissue graft or the free gingival graft, depending on the objective of therapy. For ITRT cases, the sub-epithelial, connective tissue graft is most commonly chosen for the purpose of soft tissue augmentation and increasing ridge contour volume. Though highly predictable, did report the possibility of graft failure. The dermal apron technique® is selected as an alternative to autogenous soft tissue grafts in specific situations. It must be confirmed that coronal repositioning of the facial gingival margin is not a goal of therapy. Pre-existing gingival asymmetry or recession must be identified prior to treatment and stability of the level of the gingival margin is the goal of therapy.
This is due to the avascular nature of the dermal allograft and its inability to remain partially exposed and not simply slough over time. In these case, a sub-epithelial connective graft, capable of re-vascularization and survival when not completely covered by overlying soft tissue, should be the selected method of soft tissue augmentation. In Elian Class I and II sockets, where the facial gingival margin pre-operatively is at an acceptable level, the dermal apron technique® can be chosen as a viable alternative to autogenous grafts.
References
- Rungcharassaeng K, Kan JY, Yoshino S, Morimoto T, Zimmerman G. Immediate implant placement and provisionalization with and without a connective tissue graft: An analysis of facial gingival tissue thickness. Int J Periodontics Restorative Dent. 2012;32(6):657.
[Google Scholar] [PubMed]
- Linkevicius T, Apse P, Grybauskas S, Puisys A. The influence of soft tissue thickness on crestal bone changes around implants: A 1-year prospective controlled clinical trial. Int J Oral Maxillofac Implants. 2009;24(4):712-719.
[Google Scholar] [PubMed]
- Tarnow DP, Chu SJ, Salama MA, J Stappert CF, Salama H, Garber DA, et al. Flapless postextraction socket implant placement in the esthetic zone: Part 1. The effect of bone grafting and/or provisional restoration on facial-palatal ridge dimensional change-a retrospective cohort study. Int J Periodontics Restorative Dent. 2014;34(3):323-331.
[Crossref] [Google Scholar] [PubMed]
- Chu SJ, Saloma MA, Salama H, Garter DA, Saito H, Sarnachiaro GO, et al. The dual-zone therapeutic concept of managing immediate implant placement and provisional restoration in anterior extraction sockets. Compend Contin Educ Dent. 2012;33(7):524-534.
[Google Scholar] [PubMed]
- Grunder U. Crestal ridge width changes when placing implants at the time of tooth extraction with and without soft tissue augmentation after a healing period of 6 months: Report of 24 consecutive cases. Int J Periodontics Restorative Dent. 2011;31:9-17.
[Google Scholar] [PubMed]
- Yoshino S, Kan JY, Rungcharassaeng K, Roe P, Lozada JL. Effects of connective tissue grafting on the facial gingival level following single immediate implant placement and provisionalization in the esthetic zone: A 1-year randomized controlled prospective study. Int J Oral Maxillofac Implants. 2014;29:432-440.
[Crossref] [Google Scholar] [PubMed]
- Jung RE, Holderegger C, Sailer I, Khraisat A, Suter A, Hammerle CH. The effect of all-ceramic and porcelain-fused-to-metal restorations on marginal peri-implant soft tissue color: A randomized controlled clinical trial. Int J Periodontics Restorative Dent. 2008;28:357-365.
[Google Scholar] [PubMed]
- Levin BP. The dermal apron technique for immediate implant socket management: A novel technique. J Esthet Restor Dent. 2016;28(1):18-28.
[Crossref] [Google Scholar] [PubMed]
- Levin BP, Chu SJ. Changes in peri-implant soft tissue thickness with bone grafting and dermis allograft: A case series of 15 consecutive patients. Int J Periodontics Restorative Dent. 2018;38(5):719-727
[Crossref] [Google Scholar] [PubMed]
- Levin BP, Saito H, Reynolds MA, Chu SJ. Changes in peri-implant soft tissue thickness with bone grafting and dermis allograft. Part II: A comparative retrospective case series using a subcrestal angle correction implant design. Int J Periodontics Restorative Dent. 2020;40(4):539-547.
[Crossref] [Google Scholar] [PubMed]
- Levin BP, Saito H, Chu S, Rubin J, Chu SJ. Changes in peri-implant soft tissue thickness with bone grafting and dermis allograft. Part III: A case series using a novel, hybrid implant design with a subcrestal angle correction. Int J Periodontics Restorative Dent. 2022;42(6):723-729.
[Crossref] [Google Scholar] [PubMed]
- Crespi R, Cappare P, Gastaldi G, Gherlone EF. Buccal-lingual bone remodeling in immediately loaded fresh socket implants: A cone beam computed tomography study. Int J Periodontics Restorative Dent. 2018;38(1):43-49.
[Crossref] [Google Scholar] [PubMed]
- Bressan E, Guazzo R, Tomasi C, Gutierrez Pena T, Galindo-Moreno P, Caponio VCA, et al. Influence of soft tissue thickness on marginal bone level around dental implants: A systematic review with meta-analysis and trial-sequential analysis. Clin Oral Implants Res. 2023;34(5):405-415.
[Crossref] [Google Scholar] [PubMed]
- Ferrari M, Carrabba M, Vichi A, Goracci C, Cagidiaco MC. Influence of abutment color and mucosal thickness on soft tissue color. Int J Oral Maxillofac Implants. 2017;32(2);393-399.
[Crossref] [Google Scholar] [PubMed]
- Elian N, Cho S, Froum S, Smith RB, Tarnow DP. A simplified socket classification and repair technique. Pract Proced Aesthet Dent. 2007;19(2):99-104.
[Google Scholar] [PubMed]
Citation: Levin BP (2024). Update on the Efficacy of the Dermal Apron Technique: Increasing Peri-Implant Mucosal Thickness and Tissue Stability. J Dentistry. 14:704.
Copyright: © 2024 Levin BP. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

