Indexed In
- Academic Journals Database
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Scimago
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- MIAR
- University Grants Commission
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Review - (2020) Volume 11, Issue 2
Understanding the Lacunae in Knowledge and Attitude Leading to Vaccine Hesitancy
Anirban Dutta Resident Doctor1*, Ahmed Tarek Mohamed Hamdy Mahdy2 and Sonali Sachdeva32Al Andalus polyclinics, Alexandria City, Egypt
3Department of Medicine, Lady Hardinge Medical College, New Delhi, India
Received: 25-Mar-2020 Published: 17-Apr-2020, DOI: 10.35248/2157-7560.20.11.413
Abstract
Vaccine hesitancy is defined as the reluctance or refusal to vaccinate despite the availability of vaccines. The World Health Organization identified Vaccine hesitancy as one of the ‘Ten threats to global health in 2019. Vaccine hesitancy affects not only the individuals but also the society by attributing to a decline in 'Herd Immunity'- a concept central to the success of vaccination campaigns. Despite being refuted by more credible sources, misinformation about vaccines continue to pave way for mistrust upon vaccines, even in economically weaker countries where vaccine coverage is inadequate. Religious beliefs and previous experiences with vaccination influence vaccine seeking behavior. Adverse Events following immunization (AEFI) may be an important factor with respect to newly launched vaccine programs. Numerous strategies have been employed including but not limited to educating target population, employing reminder and follow-up, engaging religious or other influential leaders to promote vaccination, and making vaccination mandatory. While the success of each of these strategies varies from place to place, mandating vaccination has faced some vocal opposition in the past. Vaccine hesitancy is not likely to be noticed by the common healthcare provider unless another disease outbreak attributable to it is noticed. Hence, it is imperative for the medical community to look into this matter with utmost seriousness and identify and devise strategies that cull this dilemma with an approach to understand the lacunae in knowledge or attitude of the recipients.
Keywords
Vaccine hesitancy; Immunization; Anti-vaccination propaganda; Herd immunity
Introduction
People who refuse to vaccinate their kids have been ridiculed on the internet for the past many years. While anti vaccination sentiments have persisted for as long as vaccines have, these scattered voices of distrust have slowly organized themselves into a serious menace. The World Health Organization identified Vaccine hesitancy (defined as: the reluctance or refusal to vaccinate despite the availability of vaccines) as one of the ‘Ten threats to global health in 2019 [1].
Diseases that were nearly eliminated have started making a comeback around the world. Anti-vaccine rallies and online campaigns have caught strength despite being condemned by a large majority of people. A developing tactic in such campaigns is the "promotion of irrelevant research as an active aggregation of several questionable or peripherally related research studies in an attempt to justify the science underlying a questionable claim [2]. The most notorious of these claims is the link of vaccination with autism. This persisting hoax is a result of a fraudulent 1997 article by Andrew Wakefield and his 11 coauthors in The Lancet that claimed to link the MMR (Measles, Mumps and Rubella) vaccine to colitis and autism spectrum disorders [3]. Despite being refuted by more credible studies [4-6]. This piece of misinformation continues to be integral in the anti-vaccination propaganda.
Vaccine hesitancy lies within a spectrum ranging from outright rejection of any form of vaccination to acceptance without reservation or hesitancy. Vaccine hesitant individuals are a heterogeneous group of people who may accept certain vaccines and reject others, skip certain vaccines or may not get them in the designated time period. Vaccine safety concern is only one aspect of vaccine hesitancy and the two must not be equated. Most of the issues underplaying vaccine hesitancy are complex. Past experiences with vaccination (positive or negative) influence willingness for future immunizations. Adverse events following immunization (AEFI) bear importance in such context. Risk of adverse events leading to hesitancy occurred particularly in the context of mass campaigns, and was more likely with newlyintroduced than established, more familiar vaccines [7].
Lack of confidence in vaccines is a serious problem that has stemmed out of misinformation about vaccines. A WHO/ UNICEF Joint Reporting Form (JRF) analysis in 2012 revealed that lack of confidence in vaccines was a significant problem, even in low-income settings. In Uganda, where lack of access was viewed as the main problem in vaccine outreach, as high as 19% of the population lacked confidence on effectiveness of vaccines [7].
Factors
In an era of man-made disasters borne out of greed, vaccine hesitancy poses a challenge different from the rest. At the heart of this menace is an idea that is a very humane- “Every parent wants to do the best for their children. ” This idea is why strategies based on reason may not elicit quick change in people with vaccine hesitancy. For example, during the pH1N1 influenza pandemic, many pregnant women hesitated to obtain pandemic influenza vaccination despite the recommendation by their health care provider and their country ’ s immunization program leaders. Even improved access to receive vaccine did not reliably overcome this [7].
Another concern is the barrier posed by religion. Numerous studies have shown that religion influences decisions on vaccination [8-10], and religious objection is more often that not an excuse used by parents as to avoid the vaccination of their children [11].
There is merit in the question of validity of parental autonomy in a situation where their decision is factually baseless and potentially detrimental to health of the children and the community [12]. The ethical considerations in such situations cannot be limited to those impacting individuals; it is necessary to consider the policy in a public health ethics context [13].
The society benefits from universal vaccination in more way than one. Unlike other medicines, vaccines are beneficial to the individual and the community at the same time. ‘ Herd Immunity’ is a concept fundamental to success of vaccination campaigns. Outbreaks of highly contagious diseases like Measles may be attributed to local decline in Herd Immunity. The outbreak of Measles in California, USA (2014-15) is a recent example of the same [12].
The problem has not gone unnoticed, however. WHO ’ s Increasing Vaccination Model (Figure 1) is a succinct illustration of the process of utilization of vaccines in the society.
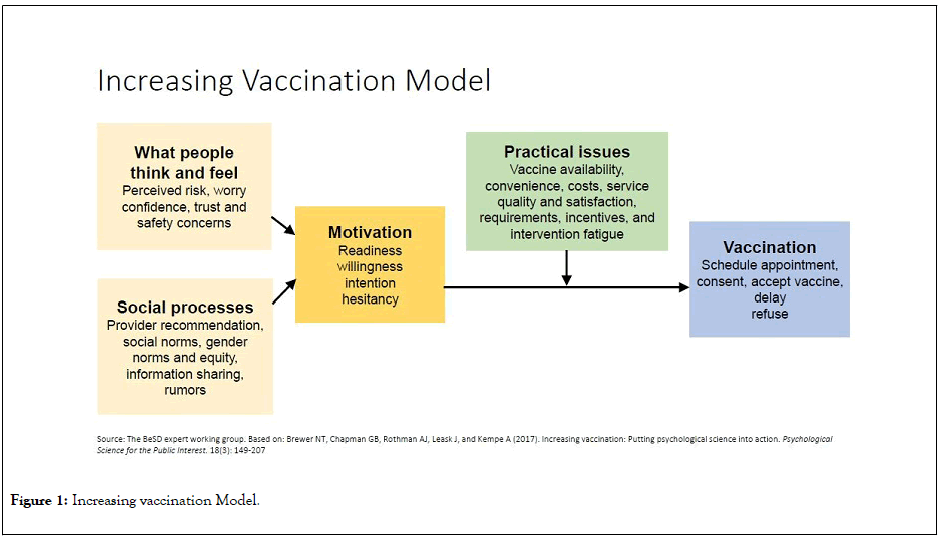
Figure 1: Increasing vaccination Model.
A WHO SAGE working group study on strategies for addressing vaccine hesitancy focused on interventions that were successful in improving vaccine uptake and shaping a positive outlook towards vaccination. It found that the introduction of education initiatives, particularly those that embed new knowledge into a more tangible process (e.g., hospital procedures, individual action plans), were more successful at increasing knowledge and awareness and changing attitudes [14]. Interventions like improving convenience and access to vaccination; mandating vaccinations or imposing sanctions for non-vaccination; employing reminder and follow-up; and engaging religious or other influential leaders to promote vaccination in the community proved effective in encouraging a more positive outcome [14].
But making vaccination mandatory has faced opposition in the past. The California Senate Bill 277 mandated vaccination of children prior to admission in any elementary or secondary school, daycare facility, nursery school or development facility [15]. This bill faced stiff and sometimes foul resistance by a small but vocal group of people. The chief issue in such a scenario is the resistance to forced vaccination.
Research in the issue of vaccine hesitancy is new and with time, strategies that work best locally will be more intelligible. Present findings tell that although a variety of strategies can be applied to tackle vaccine hesitancy, success of the individual strategies vary widely among the target populations. Strategies that incorporate multiple approaches and those strategies that are dialogue based tend to perform better [14,15]. Pre-natal visits provide a great opportunity to address concerns of parents regarding vaccination. Counseling them and facilitating parents to educational resources for further understanding of vaccination is a simple method that can be adapted by all clinicians. Addressing public health issues without affecting the anecdotal judgments-benignly intended, but lacking scientific substantiation should not be allowed to override common sense, reasoned consideration, and rational public health policy [16].
A recent bill passed by the state of New York repealed all non-medical exemptions from vaccination prior to admission into schools [17].
Conclusion
Vaccine hesitancy is not likely to be noticed by the common healthcare provider unless another disease outbreak attributable to vaccine hesitancy is noticed. Hence, it is imperative for the medical community to look into this matter with utmost seriousness and identify and devise strategies that cull this dilemma with an approach to understand the lacunae in knowledge or attitude of the recipients.
REFERENCES
- Ten health issues WHO will tackle this year. WHO. 2019.
- Foster, Craig A.; Ortiz, Sarenna M. Vaccines, Autism, and the Promotion of Irrelevant Research: A Science-Pseudoscience Analysis. Skeptical Inquirer. 2020;41: 44-48.
- Wakefield D, Murch S, Anthony A, Linnell J, Casson D, Malik M. Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children. The lancet. 1998;351:637-641.
- Measles, mumps, and rubella (MMR) vaccine. Centers for Disease Control and Prevention. 2008.
- Institute of Medicine (US) Immunization Safety Review Committee. Immunization safety review: vaccines and autism. InImmunization Safety Review: Vaccines and Autism. 2004.
- Demicheli V, Rivetti A, Debalini MG, Di Pietrantonj C.Vaccines for measles, mumps and rubella in children. The Cochrane Database of Systematic Reviews. 2012;2: CD004407.
- Repici A, Maselli R, Colombo M, Gabbiadini R, Spadaccini M, AnderloniA,et al. Coronavirus (COVID-19) outbreak: what the department of endoscopy should know. Gastrointestinal Endoscopy. 2020.
- Shelton RC, Snavely AC, De Jesus M, Othus MD, Allen JD. HPV vaccine decision-making and acceptance: does religion play a role?. J relighealt. 2013;52:1120-1130.
- Ruijs WL, Hautvast JL, van der Velden K, de Vos S, Knippenberg H, Hulscher ME. Religious subgroups influencing vaccination coverage in the Dutch Bible belt: an ecological study. BMC public health. 2011;11:102.
- Ruijs WL, Hautvast JL, Kerrar S, Van der Velden K, Hulscher ME. The role of religious leaders in promoting acceptance of vaccination within a minority group: a qualitative study. BMC public health. 2013;13:511.
- Yang YT, Silverman RD. Legislative prescriptions for controlling nonmedical vaccine exemptions. JaMa. 2015;313:247-248.
- Hendrix KS, Sturm LA, Zimet GD, Meslin EM. Ethics and childhood vaccination policy in the United States. American journal of public health. 2016;106:273-278.
- Silverman RD, Hendrix KS. Point: should childhood vaccination against measles be a mandatory requirement for attending school? Yes. Chest. 2015;148:852-854.
- Strategies addressing vaccine hesitancy. WHO. 2019.
- Bill Text - SB-277 Public health: vaccinations. An act to amend Sections 120325, 120335, 120370, and 120375 of, to add Section 120338 to, and to repeal Section 120365 of, the Health and Safety Code, relating to public health. 2019.
- Touyz SJ, Touyz LZ. The kiss of death: HPV rejected by religion. Cur Oncol. 2013;20:e52.
- Bill Text- S2994A. The New York State Senate. 2019.
Citation: Dutta A, Sonali S, Ahmed TMHM (2020) Understanding the Lacunae in Knowledge and Attitude Leading to Vaccine Hesitancy, India. J Vaccines Vaccin.11:413 DOI: 10.35248/2157-7560.20.11.413
Copyright: © 2020 Dutta A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

