Indexed In
- Open J Gate
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- International Scientific Indexing
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2023) Volume 12, Issue 5
Underserved Rural Areas: A Systematic Review of Primary Care Geographical Access using Gravity Models
Christian Simoneau*Received: 18-Sep-2023, Manuscript No. JGRS-23-23080; Editor assigned: 21-Sep-2023, Pre QC No. JGRS-23-23080 (PQ); Reviewed: 05-Oct-2023, QC No. JGRS-23-23080; Revised: 12-Oct-2023, Manuscript No. JGRS-23-23080 (R); Published: 19-Oct-2023, DOI: 10.35248/2469-4134.23.12.312
Abstract
Background: Health services are important for quality of life and employment, but are often seen as an expense, not an investment. Canadians in rural areas have lower health levels than urban residents and higher mortality rates for several diseases and conditions. The lack of healthcare services in remote areas leads to poor health, worsened by difficulty accessing primary care doctors and specialists.
Aim: We analyzed literature on geographic access methods to primary care in non-urban settings and conducted a systematic review to assess studies using gravity models. The goal was to explore the use, application, and operationalization of Floating Catchment Area (FCA) methods and their ability to identify variations in access in non-urban areas.
Methods: We completed a systematic review based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) method of all published studies on geographical access to primary care in advanced economies in six databases: ABI/INFORM, MEDLINE, Science Direct, Scopus, Web of Science and Wiley Online Library. Two forms were developed for data synthesis: a data extraction form with 14 categories, and a quality evaluation form based on the Consolidated Standards of Reporting Trials (CONSORT) model with 19 categories. These forms collected information on various factors, including author, title, publication year, country, geographic zone, primary care definition, primary care provider supply, method, census subdivision, catchment size, distance type, space decay, access index, main results, concept definitions, conflict of interest, and others.
Results: This review includes 32 papers on physical access to primary care. Most studies used secondary data and the Enhanced Two-Step Floating Catchment Area (E2SFCA) method, which was found to be more sensitive in identifying deficits in rural access. However, many studies lacked clear definitions and there was no clear consensus concerning the definition of a primary care provider. A limitation of this study was that the articles were primarily written in English.
Conclusion: Healthcare policymakers and providers should consider rural populations’ unique transportation needs when designing healthcare access initiatives. Barriers to improving access may include a lack of political will, funding, or understanding of rural needs. The E2SFCA method is more sensitive than Physician-to-Population Ratios (PPR) in identifying underserved rural populations, but has not been widely used in Quebec. Future research should compare these methods and develop recommendations for improving access to primary care for rural populations.
Keywords
Systematic review; Geographic access; Primary care; Floating catchment area method; Health disparities
Introduction
The healthcare sector represents a rapidly expanding economic industry in advanced economies, including peripheral regions. According to Bailly and Périat this industry has the potential to become the largest employer, thereby significantly impacting the economic development of these regions [1]. In Canada, for instance, 13.5% of the workforce is employed in the healthcare industry with this proportion rising to 23% in rural areas such as Gaspésie-Iles-de-la-Madeleine [2]. The significance of health services extends beyond their role in public expenditure; they contribute to both quality of life and employment. Bloom and Canning argue that improved health can be as influential as increased income in enhancing quality of life [3]. Despite this, health services are often perceived as an expense rather than an investment, even though improved health is associated with increased individual productivity [4].
In market-based health systems, the distribution of doctors is not socially optimal resulting in territorial disparities in access to care [5,6]. Consequently, the state must redistribute the various services offered, raising concerns about distribution and access to services in remote areas with more dispersed populations. Social inequalities remain spatially distributed, with the distribution of inequalities varying across different environments [7].
The presence of inequalities within a geographical space does not necessarily indicate the direction of the relationship or the mechanism by which inequalities are produced [8]. These inequalities manifest as lower levels of health among Canadians residing in rural areas compared to their urban counterparts [9-13]. Aging significantly impacts rural communities, where access to services is often limited [14]. In this regard, a higher prevalence of diabetes is noteworthy. Additionally, rural areas exhibit higher mortality rates for several pathologies, including: +15% for lung cancer, +9.2% for ischemic heart disease, +6.6% for cerebrovascular disease, +15.4% for chronic lung disease, +64.4% for suicide (with predominance among men), +202.9% for motor vehicle accidents, and +28.9% for infant mortality.
Due to its vast size, Quebec faces unique challenges in providing adequate healthcare services, particularly in rural and remote communities [9]. Access to healthcare services is a significant issue in these areas, where residents must travel longer distances to access care and often face shortages of professionals [15,16]. As notes, “these communities have difficulty attracting and retaining nurses, doctors, and other healthcare providers”. Consequently, distance and challenging socio-economic conditions create a friction effect that limits access to first-line care, the supply of which is fragile.
The scarcity of healthcare services in remote areas contributes to the poor health of populations residing far from major centres compounded by difficulties in accessing primary care physicians and specialists [9,17]. Numerous studies and government reports have noted the shortage of healthcare providers in rural areas [18-20]. The absence of clinicians is a significant concern for residents of these areas, as general practitioners often serve as the first point of contact with the healthcare system. The availability of primary care physicians has been shown to reduce mortality overall, particularly from cancer, heart disease, stroke, and infant mortality.
Significant disparities exist in the delivery of primary healthcare in Quebec. While nearly 90% of the rural and remote population has access to a family physician or CLSC (Centre Local de Services Communautaires) within a 15-minute drive, the number of healthcare providers decreases from urban to rural areas. Many rural areas, particularly in northern and eastern Quebec, experience a shortage of physicians. The number of emergency room visits appears to corroborate the unavailability of family physicians (VGQ, 2020), with 71% of visits related to non-urgent consultations (2019) and 72% of patients who consulted the emergency room having a family physician. Additionally, the wait time to obtain a family doctor is increasing annually, reaching 477 days in December 2019. For the Quebec population as a whole, 82% are registered with a family physician, while 7% remain on a registration list awaiting one. This indicates that nearly 20% of the population lacks access to primary healthcare in Quebec and must resort to emergency rooms or private clinics. In reality, this number could be higher and particularly problematic in population centres farther from urban hubs.
Measuring health presents a significant challenge, as it is multidimensional and often subject to random measurement errors due to inadequate assessment (e.g., insufficient equipment, staff training, or field documentation) or variability in measurements resulting from the timing of data collection (e.g., blood pressure, epidemics). Regardless of the approach employed (medical, self-reported, or functional), ill-health is considered a deviation from a pre-established norm across any dimension of well-being (physical, mental, or social). Researchers from various fields (public health, health research, or health economics) develop their own sets of health indicators, few of which are satisfactorily measured [21]. Most health indicators used in the literature focus on a single dimension of population health, either mortality (based on life expectancy) or disease/injury (morbidity indicators) [22]. When administrative borders are used “as is” in these measurements, cumulative errors can increase and diminish the utility of the data collected.
The aim of this review was to analyse the current literature on geographic access methods to primary care and identify the most appropriate method for use in non-urban settings. To this end, a systematic review was conducted to assess recent studies that explicitly employed gravity models as their theoretical framework. The broader rationale for this review was to explore: The use of different FCA methods; the application and operationalization of FCA methods; and evidence for influencing factors concerning the capacity and sensitivity of such methods to identify variations in access, primarily in non-urban areas.
Literature Review
The urban-rural divide in access to healthcare has been extensively studied in developed economies. In this study, rural areas are defined as non-metropolitan areas. Several studies have found that rural areas typically have reduced access to healthcare services [23-25]. However, few studies have examined the impact of location remoteness on access to healthcare, particularly variations between urban and rural contexts. Salze highlighted the importance of rurality in reducing access in France, while Hausdorf noted lower satisfaction with access to healthcare among residents of remote areas [25,26]. Laditka reported increased hospitalization rates with increasing rurality, and Sibley and Weiner (2011) found that individuals living in the most rural areas had the lowest odds of having a physician [23,27]. Populations residing in these areas typically face increased challenges in accessing primary care and emergency rooms with reduced access to healthcare services generally attributed to fewer clinicians and longer travel times [28]. Other factors, such as transportation availability, can also influence perceptions of access and the use of health services [29,30]. Multiple studies have confirmed the link between rural residence and decreased access to and use of health services [25,31,32].
In addition to structural barriers, such as a shortage of health professionals, geographical barriers, such as distance, also exist [10]. These access difficulties can foster resignation among underserved populations and contribute to a lack of interest in seeking medical attention resulting in lower prevalence of examinations and screening tests [17,33]. Numerous studies confirm that geographic access to health services strongly impacts service utilization, although it is not always the only determinant [29,34-36]. For example, Gao examined the relationship between place of residence and the likelihood of receiving a kidney transplant among Aboriginal patients [37].
However, many studies assume that rural areas are homogeneous, whereas it is more relevant to consider local realities and subdivide them into sub-regions due to wide variations in size, population density, and road infrastructure availability. While the health status of rural populations is generally lower than that of their urban counterparts, these populations are not always considered vulnerable by researchers. For instance, Champagne mentioned access issues for young and elderly patients or those with developmental/mental health issues but did not consider challenges linked to distance within rural areas [28].
While the definition of urban territory is generally accepted, the definition of rural territory is less clear. The concept of rurality is not unanimously accepted in Canada, and no precise definition has emerged [38]. Often, it is defined as a negative version of the urban (i.e., non-urban). Criteria such as population thresholds, density, and distance to an urban centre, type of employment, or travel to work are sometimes used to determine what is considered rural. However, these approaches create a divide between urban and rural without recognizing an intermediate zone. It is therefore preferable to define rurality according to the problem at hand, insofar as it is “operationalizable.”
While the presence of health services does not guarantee the overall health status of a population, these services play a significant role in promoting well-being by maintaining and promoting health, preventing disease, restoring health and function, and contributing to population health. Healthcare is a continuum, from prevention to treatment. However, without access to such services in non- urban settings, their effects cannot be realized, exacerbating health inequalities.
Measuring proximity and accessibility
According to the Joseph and Phillips framework, measures of potential access can be classified into two categories: regional availability and regional accessibility [39]. The regional availability approach, also known as the provider-to-population ratio measures potential access within strict administrative units and has been widely used in government initiatives and literature to identify health shortage areas [40-43]. Population-provider ratios are relatively easy to interpret and provide a straightforward analysis of spatial access values. However, they are limited by two major assumptions: they only account for variations within strict geopolitical boundaries and assume that individuals do not seek services outside their administrative unit [39,43,44].
In response to the limitations of regional availability measures, a range of techniques known as gravity models have been developed [45]. These models predict the potential interaction between population location and all available service points within a reasonable distance providing a measure that accounts for both proximity and availability [39,43]. Broadly speaking, gravity models examine flows or movements between two sites, such as a patient’s residential location and a doctor’s office. As the distance between the provider and consumer increases, the number of interactions decreases, diminishing the attractiveness of a service and increasing travel impedance. These techniques reveal more spatial variation by utilizing finer-resolution spatial data and removing issues of rigidly defined borders since “regional availability measures do not reveal the spatial variation within the boundary, nor do they account for the interaction between supply and demand across the boundary” [46].
Gravity-based models have been frequently used in studies, mainly in Canada and the United States of America, and preferentially in urban settings. In other countries, such as Germany and Belgium, there has been recent increased awareness and use of these models. In recent health literature, population demand is typically represented by the geographic or population-weighted centroid of an area while physician supply is determined by the actual location of services, typically geocoded to a specific address or zip code aggregation [47].
The Floating Catchment Area (FCA) method uses circular buffers around census tract population centroids to compute a physician- to-population ratio from the number of enclosed facilities. Through this methodology, the buffer radius represents catchment and reveals the distance individuals are willing to travel to access healthcare services. Services falling within the catchment area are considered fully available within that catchment. The FCA method was criticized for only considering supply while ignoring demand since “access” remains unconsidered. Radke and Mu addressed this issue with the development of a spatial decomposition method later termed the Two-Step Floating Catchment Area (2SFCA) method by Luo and Wang (Figure 1) [48,49]. The 2SFCA method has been employed in multiple recent studies measuring healthcare accessibility [47,50-54].
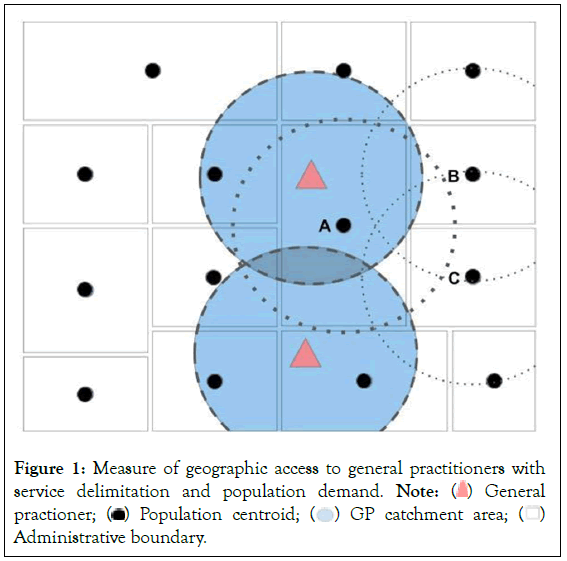
Figure 1: Measure of geographic access to general practitioners with
service delimitation and population demand. Note:  General practioner;
General practioner;  Administrative boundary.
Administrative boundary.
Since spatial accessibility must capture both proximity and availability, two distinct elements are used:
a) The location of primary care services and the population;
b) The quantity of services and population size at each location.
The 2SFCA method treats distance (i.e., time) impedance as a dichotomous measure, with any distance within a threshold considered equally accessible and any distance beyond the threshold considered equally inaccessible. The first step of the 2SFCA is to determine the population within the catchment of each service provider (i.e., the potential population size being “served”). The second step is to allocate services to the population by identifying the services within the catchment area for each population radius. The calculation of both steps produces a familiar population-to- provider ratio, specifically, the number of physicians per population within the defined area. Consequently, it maintains most of the advantages of a gravity model while also being intuitive to interpret, as it essentially generates a special form of physician-to-population ratio [49].
Since the original 2SFCA method was limited by the assumption of equal access within catchments and that locations outside the catchment have no access, an updated method incorporating a distance-decay parameter was later proposed. Luo and Qi developed the E2SFCA (Enhanced two-step floating catchment area) method by incorporating a distance decay function into both algorithmic steps [52]. By assigning weights to step one and step two within the 2SFCA method (hence “enhanced”), the model resolved issues previously identified in health service literature. Each catchment is divided into multiple sub-catchments with varying weights differentiating travel time zones (defined by a Gaussian weight function) that can be adjusted depending on the type or importance of a service. This strategy acknowledges that services closer to the census tract centroid are more accessible. Additionally, the magnitude of Gaussian weights used during analyses can vary according to research context or service type (e.g., primary care, specialized care) in a Christallerian approach. The advantage of the E2SFCA method is that multiple distance decay weights replace the dichotomous 0 and 1 in 2SFCA. Consequently, it solves the issue of not differentiating accessibility within catchments and is theoretically more analogous to gravity models, improving its finer discrimination analysis capacity. As such, localized over-or under-served areas can be identified. The E2SFCA method treats more distant providers as less accessible through distance decay coefficients while measuring distance in travel time through actual road networks.
An alternative to the E2SFCA is the Three-Step Floating Catchment Area (E3SFCA) method. This model is based on a more reasonable assumption of healthcare demand for medical services, as it assumes that a local population’s demand at a nearby service site is affected by travel cost to that site as well as travel costs to adjacent service sites. This is logical, as demand for a particular medical site will decrease when adjacent sites are also available to the population. To achieve this, the method assigns a travel time-based competition weight to each pair of population-clinic sites, which is used to calculate demand for service sites, thereby minimizing overestimation. While this method integrates a third aggregation step with the existing two-step method to calculate neighbourhood accessibility, it also generates a single numerical value representing “access” to primary healthcare services of a specific type for each neighbourhood [55].
These methods have important limitations when applied in non- urban contexts. Notably, the 2SFCA method does not consider distance decay within catchments and relies on fixed catchment sizes for all physician (i.e., supply) and population (i.e., demand) locations [24]. Distance decay is assumed to be negligible within a catchment, which is not the case in large geographical regions with widely dispersed populations and extensive catchments. This effect is most pronounced in rural areas, where catchment sizes for supply and demand are not differentiated between densely populated metropolitan areas and sparsely populated rural or remote areas.
Another major limitation is the assumption that all residents of a catchment area use services equally, regardless of population characteristics. This falsely assumes constant demand, as people’s demand at one service site can decrease when other sites are available simultaneously. The 2SFCA method may overestimate demand for some service sites, with the overestimation effect increasing when more service sites are available (e.g., in urban areas with densely concentrated medical sites). Large or irregularly shaped study areas are more susceptible to this problem, potentially leading to underestimation of accessibility in larger (i.e., rural) study areas and overestimation in smaller (i.e., urban) study areas. 2SFCA-based studies published to date assume that people travel to healthcare facilities via a single transport mode, typically a car. Weaknesses can be overcome by including both a distance-decay (impedance) function and a catchment capping function in more densely populated areas. Notably, the enhanced Two-Step Floating Catchment Area (E2SFCA) method by Luo and Qi and the Three-Step Floating Catchment Area (3SFCA) method by Wan should be more sensitive to primary care access in rural areas than the original 2SFCA.
Methodology
This systematic review was conducted to assess recent studies that explicitly employed gravity models as their theoretical framework. The broader rationale for this review was to explore: The use of different FCA methods; the application and operationalization of FCA methods; and evidence for influencing factors concerning the capacity and sensitivity of such methods to identify variations in access, primarily in non-urban areas (Table 1).
| Limits activated | English Publication Date from 2000/01/01 to 2021/12/31 |
|---|---|
| AND | "Physician" or "doctor" or "MD" or "DO" or "medical practitioner" or "GP" or "general practitioner" or "family doctor" or "family physician" or "primary care provider" or "PCP" or "medical" or "medicine" or "health" |
| AND | "access" |
| AND | "Spatial" or "Geographical" or "Physical" |
Table 1: Search strategy access to primary healthcare.
This systematic review followed the PRISMA statement, with minor modifications [56]. The PRISMA statement provides guidelines to increase the integrity and reproducibility of systematic reviews, using a checklist of twenty-seven items and a 4-step flow diagram that must be included in the Abstract, Introduction, Methodology, and Discussion sections of the study. Conducted in 2022, this systematic review aimed to analyze the physical access measurement methods used for primary healthcare access.
Literature search and study selection
Six databases were used for this systematic review: ABI/INFORM, MEDLINE, Science Direct, Scopus, Web of Science, and Wiley Online Library. Using multiple databases ensured increased coverage of articles and studies and is essential for producing a systematic review [57]. The search strategy aimed to identify articles published in English between 2000 and 2021 that used a geographical-access method to measure population access to primary healthcare within developed countries (United States of America, Canada, United Kingdom, Australia, New Zealand, Belgium, and Germany) to achieve comparability (Table 1). To ensure all potentially relevant articles were identified, search terms included the names of methods used as well as terminology employed in geographical healthcare access.
Selection
The selection of articles followed a systematic review methodology and was performed as follows: Title, Abstract and Full text. Inclusion and exclusion criteria were defined prior to each step (Table 2). Of the initial 147 studies retrieved through the six databases, 32 papers met all the inclusion criteria (Figure 2).
| S. No | Step | Inclusion criteria | Exclusion criteria | Hits |
|---|---|---|---|---|
| 1 | Selection by title | 1. Studies related to healthcare access 2. Use of a geographical or physical or spatial access method |
1. Studies not primarily related to healthcare access 2. Focus on specific health problems such as cancer, kidney failure, AIDS 3. Specific study population (veterans, immigrants, specific ethnic group) 4. Specific healthcare sector (dental, rheumatology physical therapy, nursing homes, intensive care, emergency rooms) 5. Studies not conducted in a developed country 6. Studies on children or on the elderly |
147 |
| 2 | Selection by abstract | - | - | 55 |
| 3 | Selection by full-text | - | Additional exclusion criterion: 1. Using only professional-to-population ratio |
32 |
Table 2: Inclusion and exclusion criteria used for study selection.
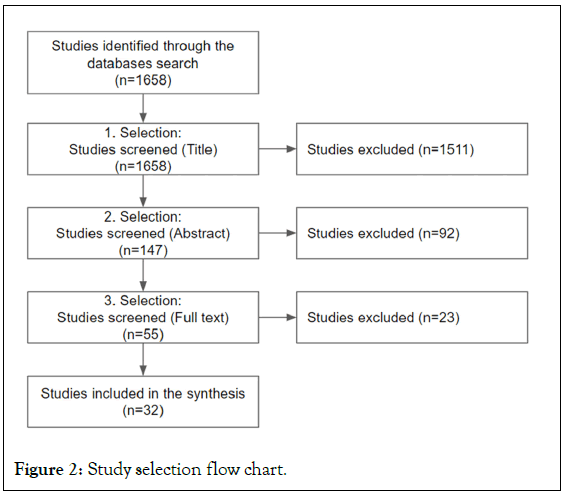
Figure 2: Study selection flow chart.
Data analysis
In preparation for data synthesis, two forms were developed: a data extraction form with 14 categories, collecting information on author, title, publication year, country, geographic zone, primary care definition, primary care provider supply, method, census subdivision, catchment size, distance type, space decay, access index, and main results; and a quality evaluation form based on the CONSORT model with 19 categories collecting information on concept definitions, method used, conflict of interest, and other factors [58-60].
Subsequently, the original categories were further collated into five categories that formed the basis for presenting results in this review:
1. Study characteristics (year of publication, country of origin, primary care provider, and study quality).
2. Setting and scale (area scope, context setting, census resolution level).
3. Aim of the study (methodological improvement, empirical testing, and method comparison).
4. Use of the floating catchment method (base-method for main study design: 2SFCA, E2SFCA or 3SFCA).
5. Main results (no difference, reduced access for urban areas, equal access, reduced access for rural areas).
To present quantitative data, categories were selected as summary measures. Central themes and topics (methods, aims and settings) were extracted from the studies, summarized and presented according to their frequency of occurrence within such studies.
Results
Study characteristics
The main characteristics of the 32 papers included in this review are detailed in Table 3, along with relevant article identification numbers (AIDs-see Table 3 for detailEed reference). These studies were published between 2000 and 2021 and conducted in Canada (n=11), the United States of America (n=9), the United Kingdom (n=4), Australia (n=4), Germany (n=2), New Zealand (n=1), and Belgium (n=1). Countries with more expansive landscapes, such as Canada and the United States of America, appear to have greater interest in geographical access measurement. Almost all studies (n=29) used secondary data, primarily from national surveys and medical boards. Two studies collected data from medical records (AID: 2,32), while the Montreal study (AID: 21) used data from the Canadian Community Health Survey (2005-2006) (Figure 3).
| Article Id (AID) | Author’s, Publication year | Country | Census resolution | Family Method | Distance type | Maximum catchment | Conclusion |
|---|---|---|---|---|---|---|---|
| 1 | (Amiri et al., 2020) [60] | United States of America | Block group population weighted centroid | E2SFCA | Network time | 120 minutes | Better access to PCPs was associated with lower mortality from all-causes, cancers, and heart disease. The 2-step floating catchment area approach can help with the identification of PCP shortage areas, the development of rural residency programs, and the expansion of the physician workforce in Washington State and other regions. |
| 2 | (Barrett, 2016) [61] | Canada | Dissemination area population weighted centroid | E2SFCA | Network time | 120 minutes | The proposed method consistently shows better and more accurate results. The alternative methods often underestimate accessibility, especially in remote areas. |
| 3 | (Bauer et al., 2018) [62] | United Kingdom | Lower layer super output area level population weighted centroid | 3SFCA | Network time | 60 minutes | This study showed substantially differing GP accessibility throughout England. However, socially deprived areas did not have poorer spatial access to GPs. |
| 4 | (Bauer and Groneberg, 2016) [50] | Germany | Administrative district population weighted centroid | 3SFCA | Network time | 60 minutes | The proposed integrated FCA method integrates recent improvements on shortcomings regarding earlier FCA-methods and therefore takes relevant influencing factors into account. A case study demonstrated the general fit of the proposed method. |
| 5 | (Bell et al., 2012) [63] | Canada | Dissemination area population weighted centroid | 3SFCA | Network time | 3 Km | If there is no street address that can be used to select among tied points within a postal code then the MEP product is not beneficial to the geocoding process. There are patterns among the three cities; a one-way ANOVA indicated no significant differences between the six methods in the City of Saskatoon, whereas there were significant differences in Edmonton and Mississauga. |
| 6 | (Bell et al., 2013) [64] | Canada | Dissemination area population weighted centroid | 3SFCA | Network time | 3 Km | Potential access significantly differs between neighborhoods for all spatial and aspatial dimensions of access. Accessibility is considerably reduced for linguistic minorities and for those who might not have a dedicated family physician as compared to the general population. |
| 7 | (Bissonnette et al., 2012) [65] | Canada | Dissemination area population weighted centroid | 3SFCA | Network time | 3 Km | Neighbourhood-level potential access to primary care is dependent on spatial and aspatial dimensions of access selected for examination and potential accessibility is reduced for linguistic minorities as well as for recent immigrant populations who appear, on the surface, to have better access to walk-in clinics than dedicated physicians. T |
| 8 | (Crooks and Schuurman, 2012) [66] | Canada | Dissemination block population weighted centroid | E2SFCA | Network time | 120 minutes | Future applications of the modified gravity model are needed in order to refine the recommendations we provide on interpreting its results. It is important that studies are undertaken that can help administrators, policy-makers, researchers, and others with characterizing the state of access to PHC, including potential spatial access. |
| 9 | (Cui, 2014) [67] | Australia | Mesh blocks residential centroid | E2SFCA | Network distance | 4 Km | The study has revealed fine resolution spatial variations in accessibility to primary health care facilities and identified spatial clusters of residential areas with poor spatial accessibility to the facilities in the MMA. |
| 10 | (Dewulf et al., 2013) [68] | Belgium | Census tract centroid | The major disadvantage of PPR methods is its aggregated approach, masking subtle local variations. Some simple GIS methods overcome this issue, but have limitations in terms of conceptualisation of physician interaction and distance decay. | 5 Km | ||
| 11 | (Donohoe et al., 2016) [51] | United States of America | Census block population weighted centroid | E2SFCA | Network time | 60 minutes | The findings of this study suggest that using a relative 2SFCA approach, the spatial access ratio method, when detailed patient travel data are unavailable. The 2SFCA method shows promise for measuring access to care in Appalachia, but more research on patient travel preferences is needed to inform implementation. |
| 12 | (Higgs et al., 2017) [69] | United Kingdom | Lower layer super output area level population weighted centroid | E2SFCA | Network distance | 15 minutes | The direction and strength of the association between deprivation and accessibility measures varies by mode of travel, the main differences are actually across measures of accessibility. This has important implications for studies of potential inequalities in health service accessibility and suggests there is a need to develop consistent measures of accessibility if we are to truly understand the relationship between demand and supply |
| 13 | (Langford and Higgs, 2006) [47] | United Kingdom | Output area population dasymetrically distributed | 2SFCA | Network time | 10 minutes | The bus-riding cohort of each census tract experiences much lower accessibility levels than those estimated by an undifferentiated (car-only) model. Car drivers' accessibility may also be misrepresented in an undifferentiated model because they potentially profit from the lower demand placed upon service provision points by bus riders. |
| 14 | (Langford et al., 2016) [70] | United Kingdom | Output area population weighted centroid | E2SFCA | Network time | 15 minutes | The dasymetric model yields lower accessibility scores than a standard pro rata model. More importantly, the difference is spatially disproportionate, suggesting that the degree of disadvantage experienced in rural areas may be greater than has previously been recognized. |
| 15 | (Luo and Qi, 2009) [52] | United States of America | Census block population weighted centroid | E2SFCA | Network time | 30 minutes | Spatial accessibility pattern that is more consistent with intuition and delineates more spatially explicit health professional shortage areas. It is easy to implement in GIS and straightforward to interpret. |
| 16 | (Luo and Wang, 2003) [49] | United States of America | Census block population weighted centroid | E2SFCA | Network time | 50 minutes | The variation of spatial accessibility to primary care in the Chicago region, and analyzes the sensitivity of results by experimenting with ranges of threshold travel times in the FCA method and travel friction coefficients in the gravity model. |
| 17 | (Luo and Whippo, 2012) [46] | United States of America | Census block population weighted centroid | E2SFCA | Network time | 60 minutes | The new method is effective in determining the appropriate catchment sizes across the urban to suburban/ rural continuum and has revealed greater detail in spatial variation of accessibility compared to results using fixed catchment sizes. |
| 18 | (McGrail, 2012) [53] | Australia | Collection district population weighted centroid | E2SFCA | Network time | 60 minutes | Study assesses recent ‘improvements’ to the 2SFCA when applied over large geographic regions of both large and small populations. Its findings demonstrate the necessary combination of both a distance-decay function and variable catchment size function in order for the 2SFCA to appropriately measure healthcare access across all geographical regions. |
| 19 | (McGrail and Humphreys, 2009) [24] | Australia | Collection district population weighted centroid | E2SFCA | Network time | 60 minutes | Despite their recognised weaknesses, the Australian government uses broad geographical classifications as proxy measures of access to underpin significant rural health funding programs. This new index of access could provide a more equitable means for resource allocation. |
| 20 | (Naylor et al., 2019) [71] | United States of America | Zip code tabulated area population weighted centroid | E2SFCA | Network time | 60 minutes | The Variable-distance Enhanced 2 step Floating Catchment Area method is a viable approach to measure spatial accessibility at the national scale. |
| 21 | (Andre and Apparicio, 2011) [72] | Canada | Dissemination area clinic users weighted centroid weighted by last year usage | 2SFCA | Network distance | 500 meters | Results of this study suggest that a greater effort must be made to ameliorate spatial accessibility to medical clinics in Montreal. To ensure that health resources are allocated in the interest of the population, health planners and the government should consider a strategy in the sitting of future clinics which would provide spatial access to the greatest number of people. |
| 22 | (Roeger et al., 2010) [54] | Australia | Mesh blocks residential centroid | 2SFCA | Unknown | 8 Km | Residents of metropolitan Adelaide have low GP ratios. However, an inequitable spatial distribution of GPs within metropolitan Adelaide was found, with ~16% of residents considered to be living in areas of GP workforce shortage. |
| 23 | (Shah et al., 2015) [73] | Canada | Dissemination area population weighted centroid | 3SFCA | Network distance | 25 Km | Model incorporates a distance decay function that better represents relative spatial access to PHC. The results of the modified gravity model demonstrate greater nuance with respect to potential access scores. While variability in access to PHC physicians across the test province of Nova Scotia is evident, the gravity model better accounts for real access by assuming that people can travel across artificial census boundaries. |
| 24 | (Shah et al., 2017a) [74] | Canada | Dissemination area population weighted centroid | 3SFCA | Network distance | 25 Km | This comparative analysis between the spatial distributions of PTs and FPs demonstrates reduced services in a number of rural and urban Saskatchewan communities. |
| 25 | (Shah et al., 2017b) [75] | Canada | Dissemination area population weighted centroid | 3SFCA | Network distance | 50 Km | Nurse practitioner services are likely addressing primary care access gaps due to reduced numbers of family physician services in certain geographical areas. Combined access scores reveal inequalities in the distribution of primary health care services relative to the proportion of population aged 65 + across both provinces, particularly in rural and remote communities. |
| 26 | (Shah et al., 2020) [76] | Canada | Dissemination area population weighted centroid | E2SFCA | Network time | 30 minutes | Measuring accessibility to rural and remote healthcare services is not without technical challenges. The results of GIS approaches vary considerably depending on choice of input data, geographical area unit of analysis, and accessibility method. These methodological issues have implications for determining levels of accessibility to healthcare services (or where there is reduced access) that can impact decisions regarding health human resource decisions and policies related to rural and remote health service accessibility. |
| 27 | (Schuurman et al., 2010) [77] | Canada | Dissemination block population weighted centroid | E2SFCA | Network time | 120 minutes | Southwestern Ontario has slightly better geographic accessibility to primary care providers than the provincial average, but there remain areas with provider shortages. Primary care provider distribution is unequal across the urban‐rural continuum, with lowest accessibility in rural and small population centres within the Census Metropolitan Area. There is a mismatch between the distribution of primary care providers and high proportions of seniors, necessitating many seniors to travel long distances to access health care |
| 28 | (Subal et al., 2021) [78] | Germany | 100 m × 100 m grid | 3SFCA | Network time | 30 minutes | The application of the MH3SFCA method on small-scale data can provide an overview of accessibility for the whole study area. As many factors have to be taken into account, the outcomes are too complex for a direct and clear interpretation of why indices are low or high. The MH3SFCA method can be used to detect differences in accessibility on a small scale. |
| 29 | (Wan et al., 2012) [55] | United States of America | Census tract and census block | 3SFCA | Network time | 60 minutes | The study concludes that 3SFCA is a promising method to provide health professionals and decision makers with useful healthcare accessibility information. |
| 30 | (Wang and Luo, 2005) [79] | United States of America | Census tract population weighted centroids | 2SFCA | Network time | 30 minutes | The method presented in this paper defines HPSAs in a systematic way using quantitative criteria that are consistent, precise and flexible. The method may help the DHHS and state health departments improve current practice of HPSA designation. This research |
| 31 | (Luo and Whippo, 2012) [46] | United States of America | Census tract population weighted centroids | E2SFCA | Network time | 30 minutes | Despite its advantages, significant limitations have been highlighted within rural areas. To account for this, a cap function was introduced to the 2SFCA method to limit catchment sizes within urban areas. Results using dynamic catchment sizes in northern and southern Illinois have revealed more detailed spatial access values overall and greater variability of catchment size within rural and urban environments. |
| 32 | (Whitehead et al., 2020) [80] | New Zealand | Statistical area 2 | E2SFCA | Network distance | 45 Km | Catchment sizes vary across rural and urban areas. Further, incorporating variable data-driven population catchments recognises patient travel patterns and appears to improve spatial accessibility results in a mixed urban-rural context, although further modification may be necessary. |
Table 3: Study characteristics of 32 papers.
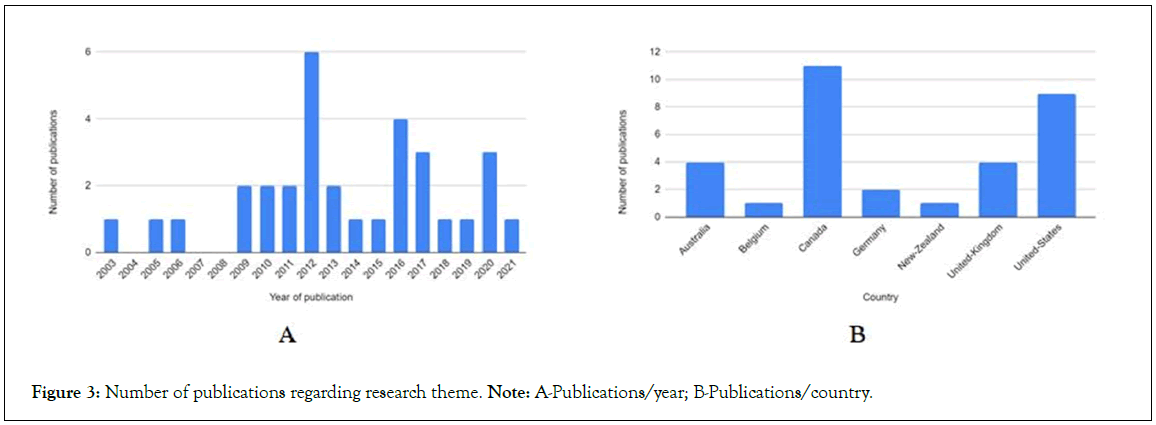
Figure 3: Number of publications regarding research theme. Note: A-Publications/year; B-Publications/country.
The type of primary care providers was mentioned in most studies (n=26) but varied across studies. Several studies included paediatricians and internists (AID: 11,15,16,19), while the most prevalent healthcare professionals were general practitioners or family physicians (as primary care providers) (n=14). Others included specialists practicing general medicine, such as paediatricians or obstetricians (n=5), and two studies compared access between family physicians and physical therapists. One study investigated access between family physicians and nurses, but only data regarding the family physician was retained.
The quality of the studies, assessed using the CONSORT method, was divided into four categories: A (AID: 4,18,29), B (AID: 1,3,9,11,12,15,17,19-21,24,28,32), C (AID: 2,8,10,14,16,23,26,30,31), and D (AID: 5-7,13,22,25,27) (Figure 4). Approximately half of the studies did not include the name of the method used in their title (n=16) or summary (n=11). Only two studies included their stated objective and hypothesis in their summary and three mentioned the limits and biases of their studies. Most studies mentioned their financing, support and conflict of interest (n=24), and all provided selection criteria and justification.
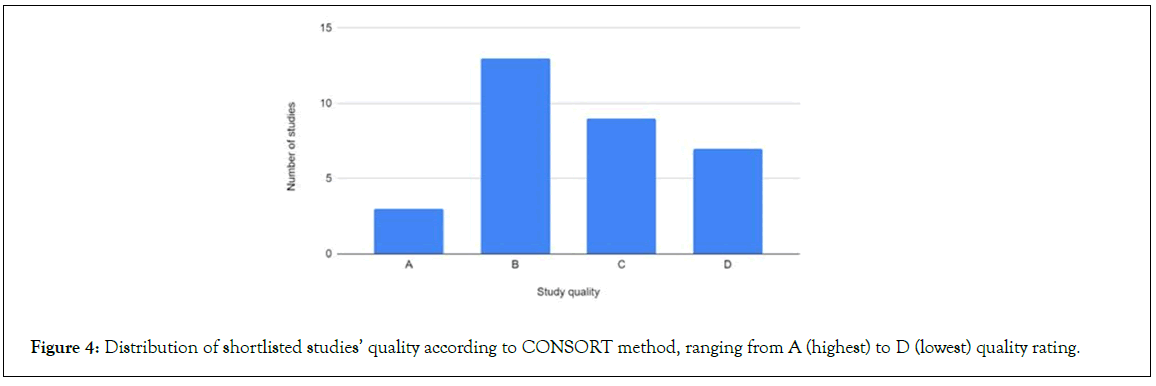
Figure 4: Distribution of shortlisted studies’ quality according to CONSORT method, ranging from A (highest) to D (lowest) quality rating.
Setting and scale
The scale of the area in the studies varied, with three studies conducted nationwide (AID: 3,11,21), 13 at the state or province level (AID: 1,2 8,12,13,18,19,23-25,27,30,31), nine at the regional or local level (AID: 11,14,15-17,26,28,29,32), and seven within city limits (AID: 4-7,9,21,22). One regional study was performed in a dense urban setting (AID: 28), bringing the total number of urban settings to nine out of the 32 studies. The remaining 23 studies were conducted in mixed environments. No study was performed solely within a rural area, indicating a lack of interest in this type of territory. As such, the most appropriate method for use in such a context cannot be assessed solely from the raw data (Figure 5).
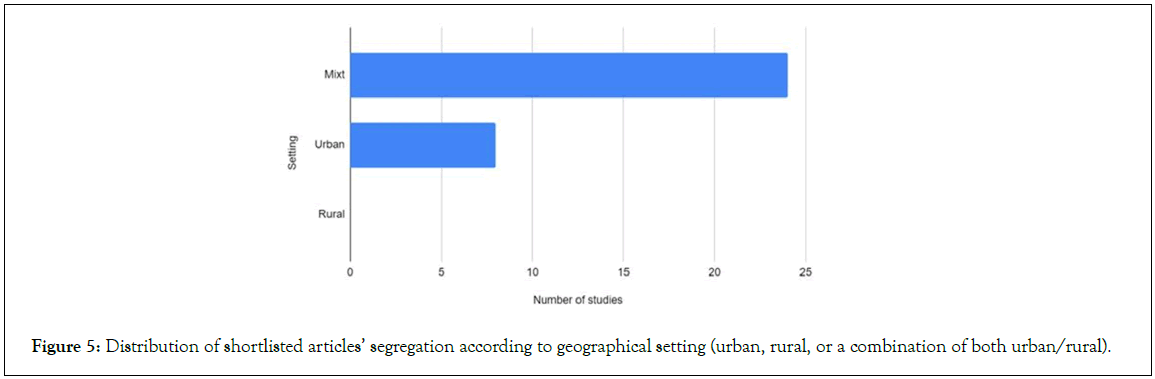
Figure 5: Distribution of shortlisted articles’ segregation according to geographical setting (urban, rural, or a combination of both urban/rural).
The size of the implemented population unit varied, with some studies using dissemination areas (or equivalent, under 1000 people) (AID: 2,5-9,13,14,21-28), others using census tracts (or equivalent,>000 but<10,000) (AID: 1-3,10-12,15-19,29-31), and some using census subdivisions ( ≥ 10,000) (AID: 20,32).
Aim of the study: Almost half of the shortlisted studies (n=15) modified part of the original method design to improve upon it (AID: 2,4,12-14,16-19,21,28-32), while nine studies compared different methods (AID: 5-7,9-11,15,24,27), and eight used one method to investigate access scores solely (AID: 1,3,8,20,22,23,25,26).
Floating catchment area family method and details: Most studies were based on the E2SFCA method (n=17) (AID: 1,2,8- 10,12,14,15,17-22,26,27,30), while ten used the 3SFCA method (AID: 3-7,23-25,28,29) and four employed the 2SFCA method (AID: 11,13,16,31). The type of distance used (time (AID: 1-8,11,13- 20,26-31) or distance (AID: 9,10,12,21,23-25,32)) was mentioned in all but one study (AID: 22) (Figure 6). The original 2SFCA and E2SFCA methods (Luo and Wang, 2003; Luo and Qi, 2009) suggest using time to improve the representation of population access, as distance alone cannot account for travel speed and speed limits and complicates the use of different transport methods [49,52].
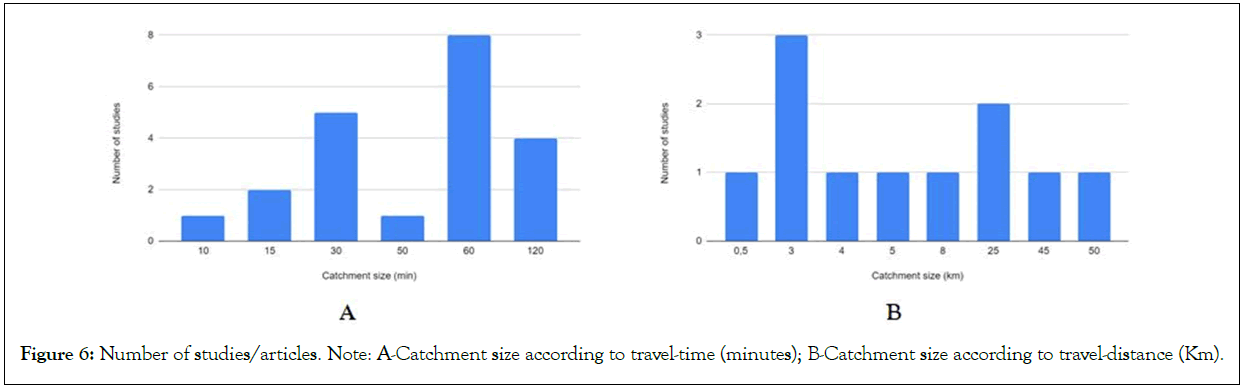
Figure 6: Number of studies/articles. Note: A-Catchment size according to travel-time (minutes); B-Catchment size according to travel-distance (Km).
When distance decay was used, only one study did not specify it (AID: 11). Depending on the method used, the distance decay could be none existing (AID: 5-7,13,16,17,22-24,30,31), discrete (AID: 2,10,15,18,20,21,32) or continuous (AID: 1,3,4,8,9,12,14,19,25-29). The maximum catchment size, while given in time unit, varied from 10 minutes (AID: 13), to 15 (AID: 12,14), 30 (AID: 15,26,28,30,31), 50 (AID: 16), 60 (AID: 3,4,11,17-20,29) or even 120 (AID: 1,2,8,27). When given in a distance unit, it varied from 500 m (AID: 21), to 3 Km (AID: 5-7), 4 Km (AID: 9), 5 Km (AID: 10), 8 Km (AID: 22), 25 Km (AID: 23,24), 45 Km (AID: 32) up to 50 Km (AID: 25). When a maximum catchment size was based on a population limit, 100 clinics (AID: 19), 500 000 people (AID: 17) and 700 000 people (AID: 31) were used.
Outcomes and main results
Comparing rural access to urban access was not the goal of most of those studies. Consequently, many did not compare access rate by type of territory, and several studies were only conducted in an urban environment (AID: 1,4-7,9,12,21,22,28). Nonetheless, when access was measured across an entire region that encompassed both types of environments, most of these studies observed a reduced access in rural areas (AID: 3,8,10,11,13-20,23-27,29, 31,32), while only one study observed the inverse pattern (AID: 30), and one measured identical access levels (AID: 2) (Table 4).
| Article Id (AID) | Studies including this criteria | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 | 25 | 26 | 27 | 28 | 29 | 30 | 31 | 32 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Method in the title | 14 | X | X | X | X | X | X | X | X | X | X | X | X | X | X | ||||||||||||||||||
| Detailed summary | 21 | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | |||||||||||
| Context | 32 | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Goal and hypothesis | 2 | X | X | ||||||||||||||||||||||||||||||
| Detailed method description | 19 | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | |||||||||||||
| Selection criteria | 32 | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Setting | 32 | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Reproducibility | 32 | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Index definition | 32 | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Justification | 32 | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Boundary delimitation | 32 | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Whole area analysis | 32 | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Results comparison | 18 | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | ||||||||||||||
| Comparative analysis | 25 | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | ||||||
| Study limits | 29 | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | |||
| Generalization | 32 | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Advantages | 32 | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Accessible protocol | 3 | X | X | X | |||||||||||||||||||||||||||||
| Disclosures | 25 | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | |||||||
| Criteria included in the study | 15 | 15 | 15 | 18 | 12 | 13 | 12 | 14 | 16 | 15 | 15 | 15 | 13 | 16 | 16 | 15 | 16 | 17 | 17 | 16 | 16 | 13 | 14 | 12 | 15 | 14 | 14 | 16 | 18 | 14 | 15 | 15 |
Table 4: Comprehensiveness of geographical primary care access studies.
When conducting an analysis of access rates by territory, the Enhanced Two-Step Floating Catchment Area (E2SFCA) method was found to be more sensitive in identifying deficits in rural access compared to other methods. This was determined through the assignment of a mean value of 2.44, based on a scale ranging from 1 to 3, where 1 indicated less access in urban settings, 2 indicated equal access, and 3 indicated less access in rural areas. The E2SFCA method takes into account both the availability of healthcare providers and the population’s spatial accessibility to these providers, making it a more comprehensive measure of healthcare access. Furthermore, when examining studies conducted in mixed environments, the E2SFCA method remained the most sensitive in identifying underserved rural areas. A Bayes Factor Approach also provided evidence that the E2SFCA method is the most probable means of identifying underserved rural access areas. This approach compares the likelihood of different hypotheses and provides a measure of the strength of evidence in favour of one hypothesis over another.
Discussion
This systematic review examined physical access to primary care in advanced economies using various Floating Catchment Area (FCA) methods. The FCA methods used in this review include the Two-Step Floating Catchment Area (2SFCA), Enhanced Two- Step Floating Catchment Area (E2SFCA), and Three-Step Floating Catchment Area (3SFCA). The 2SFCA method is a special case of a gravity model of spatial interaction that was developed to measure spatial accessibility to primary care physicians. It can also be used to measure other accessibility such as accessibility to jobs, to cancer care facilities, etc. The E2SFCA method is an enhancement of the 2SFCA method by considering distance decay within catchments. The 3SFCA method is another variation of the FCA methods.
Factors such as current geographical access measurement methods, setting and scale, type of environment, catchment size, census resolution level, outcomes, research approach, and study designs were considered in this review. The results indicated that the E2SFCA method is the most appropriate and sensitive means of identifying underserved access areas in extra-urban territories. The majority of the shortlisted studies examined study aim characteristics, including methodological improvement, comparison between methods, and empirical testing. Most were conducted with the intention of improving current methods.
Notably, no study was conducted purely in an extra-urban setting where transportation can be of particular interest. Rural areas often face limited seasonal access due to extreme weather or roads only open during the summer and are more dependent on automobile access than urban dwellers [81]. According to McGrail and Humphreys (2009), car travel accounts for more than 80% of trips taken in these areas. This can create financial stress for those who must drive long distances, particularly for the elderly and peo- ple with disabilities who may not have access to an adapted public transportation system.
In terms of study quality, many studies lacked clear definitions of what was being investigated and measured. Additionally, there was no clear consensus concerning the definition of a primary care provider. As such, it is unclear whether the implementation of the E2SFCA method by healthcare governing boards would improve access to primary care in rural areas. Future studies should examine whether rural populations who currently experience comparatively lower primary care access are able to better access these services once changes have been implemented through the E2SFCA method.
There is a strong need for international primary studies that apply the Enhanced Two-Step Floating Catchment Area (E2SFCA) method and adequately operationalize its complexity. The E2SFCA method is an enhancement of the Two-Step Floating Catchment Area (2SFCA) method by considering distance decay within catchments. Such studies should enable researchers to move beyond examinations and descriptions of simple indicators to gain a deeper understanding of the associations between geographical access and population healthcare. This would allow researchers to investigate the impact of geographical access on rural populations and determine whether the implementation of the E2SFCA method can improve access to primary care in these areas.
During the study selection process, it became apparent that FCA methods had been applied to a wide range of health services. However, most of the initially identified studies had to be excluded due to their focus on niche health service topics such as nursing homes, HIV, veterans, and cancer patients. This made it challenging to draw conclusions from comparisons between studies.
Another limitation of this study was that the articles were primarily written in English. It is possible that geographical access to healthcare methods may be discussed in articles or databases in other languages, which could provide additional insights into the topic. Additionally, the majority of shortlisted studies utilized secondary data analysis, meaning that the authors selected from datasets collected within primary studies. The dominance of certain elements and limits, such as census resolution level, may be the result of either recurring theoretical or pragmatic decisions. A follow-up literature review should compare similarities and differences in geographical access to healthcare in developing economies to gain a more comprehensive understanding of the topic.
Conclusion
The findings of this systematic literature review underscore the importance of conducting research dedicated to access to primary care for non-urban populations. There is a need for future population health research to examine the unique geographic characteristics of isolated rural communities, particularly the role of transportation in primary care access for more vulnerable populations. For instance, in some areas of the province, road access may be restricted or limited seasonally, preventing individuals from accessing health services. Access to healthcare services is, therefore, also dependent on the availability of transportation, and the mode of transportation can influence travel time. In most rural areas of Canada, the automobile is the only means of accessing services, as public transportation is generally unavailable. As such, if services are not provided locally, they are effectively inaccessible to those without a car, which can disproportionately impact already disadvantaged populations. In urban areas, public transportation is better developed, making health services more accessible to all. However, urban researchers often assume that the entire population has access to a car (INSPQ, 2009). Additionally, certain groups of individuals may not be able to use private transportation independently, such as the elderly (in some cases), children, young adolescents, people with disabilities, or those whose health conditions prevent them from driving.
These challenges highlight the need for healthcare policymakers and providers to consider the unique transportation needs and limitations of rural populations when designing and implementing healthcare access initiatives. This may include expanding public transportation options or providing subsidies for private transportation to ensure that rural residents can access necessary healthcare services. Additionally, telemedicine and other remote healthcare delivery methods may be effective in improving access to primary care for rural populations who face transportation barriers.
Despite improvements in geographic access methods’ ability to identify underserved areas over the past decade, barriers to healthcare policy changes persist due to shifting political and economic interests. The significance of these barriers should not be overlooked in ongoing research. This is particularly relevant for rural areas with limited access to advanced medical settings and infrastructure. Further studies are needed to address the challenges faced by vulnerable members of the Canadian population who are disadvantaged by the status quo that favours the use of convenient administrative boundaries at the expense of non-urban dwellers’ health.
These barriers may include a lack of political will or funding to implement changes, resistance from vested interests, or a lack of understanding of the unique needs and challenges faced by rural populations. To overcome these barriers, it is essential for researchers, policymakers, and healthcare providers to engage in ongoing dialogue and collaboration to develop and implement effective solutions. This may involve conducting additional research to better understand the specific needs and challenges faced by rural populations, advocating for policy changes at the local, provincial, and national levels, and working with community organizations and other stakeholders to develop and implement targeted interventions. By taking a collaborative and evidence-based approach, it may be possible to overcome these barriers and improve access to primary care for rural populations.
Finally, although the Enhanced Two-Step Floating Catchment Area (E2SFCA) method appears to be the most sensitive means of identifying underserved populations in rural areas that Physician- to-Population Ratios (PPR) cannot detect, this method has not been widely used in the province of Quebec except in some urban settings. The E2SFCA method takes into account both the availability of healthcare providers and the population’s spatial accessibility to these providers, making it a more comprehensive measure of healthcare access. Future research should apply this method and compare it with the standard PPR used by healthcare governing boards for resource allocation and physician allocation programs (plans régionaux d’effectifs médicaux).
Such research could provide valuable insights into the relative strengths and weaknesses of these two methods in identifying underserved populations and informing healthcare resource allocation decisions. By comparing the results obtained using the E2SFCA and PPR methods, researchers may be able to identify areas where one method is more effective than the other and develop recommendations for how these methods can be used in combination to improve access to primary care for rural populations. Additionally, this research could inform the development of new healthcare policies and programs aimed at improving access to primary care for underserved populations in rural areas.
References
- Bailly A, Périat M. Activités de santé et développement régional: Une approche médicométrique. Géocarrefour. 2003;78(3):235-238.
- Bollman R. Rural and small town Canada. 2001.
- Bloom DE, Canning D. Global demographic change: Dimensions and economic significance. Popul Dev Rev. 2008;34:17–51.
- Gubler T, Larkin I, Pierce L. Doing well by making well: The impact of corporate wellness programs on employee productivity. Management Science. 2018;64(11):4967-4987.
- Mougeot M, Naegelen F. Achieving a fair geographical distribution of health-care resources. Regional Science and Urban Economics. 2018;70:384-392.
- Bertolucci M, Tiberghien B, Saint Jonsson A, Alfano N. Access to healthcare services in medical wastelands: the «first-aid line» as a tension absorber? The case of the french fire departments. 2018.
- Alix C, Blaser C, Lo E. Disparities in premature mortality in Quebec and its regions: Different measures, different perspectives. Espaces-Populations-Societes. 2018;1-2.
- Rojas Lopez J, Pulido N. Hétérogénéité territoriale, inégalité sociale et développement local : un débat en cours. Sud-Ouest européen. Revue géographique des Pyrénées et du Sud-Ouest. 2013;(35):85-94.
- Romanow RJ. Guidé par nos valeurs: l'avenir des soins de santé. Saskatoon: Commission sur l'avenir des soins de santé au Canada. 2002.
- Martinez J, Pampalon R, Hamel D, Raymond G. Does living in rural communities rather than cities really make a difference in people's health and wellness? Institut national de santé publique du Québec. 2004.
- Ricketts TC, Goldsmith LJ, Holmes GM, Randy MR, Lee R, Taylor DH, et al. Designating places and populations as medically underserved: A proposal for a new approach. Journal of Health Care for the Poor and Underserved. 2007;18(3):567-589.
- White D. Development of a rural health framework: Implications for program service planning and delivery. Healthcare Policy. 2013;8(3):27.
[Crossref] [Google Scholar] [PubMed]
- Général du Québec V. Rapport du Vérificateur général du Québec à l’Assemblée nationale pour l’année 2008-2009. 2009.
- Arpin-Simonetti E. Regional development: A Quebec in pieces. Relationships. 2018;(798):14-16.
- DesMeules M, Pong R, Lagacé C, Heng D, Manuel D, Pitblado R, et al. How healthy are rural Canadians? An assessment of their health status and health determinants. Canadian Institute for Health Information. 2006.
- Browne A. Issues affecting access to health services in northern, rural and remote regions of Canada. Northern Article Series. Prince George, BC: University of Northern British Columbia. 2010.
- Starfield B. Measurement of outcome: a proposed scheme. The Milbank Quarterly. 2005;83(4).
- Nagarajan KV. Rural and remote community health care in Canada: Beyond the Kirby Panel Report, the Romanow Report and the federal budget of 2003. Canadian Journal of Rural Medicine. 2004;9(4):245.
[Google Scholar] [PubMed]
- Pong RW. Geographic distribution of physicians in Canada. desLibris. 2005.
- Pampalon R, Hamel D, Gamache P. Health inequalities in urban and rural Canada: comparing inequalities in survival according to an individual and area-based deprivation index. Health and place. 2010;16(2):416-420.
[Crossref] [Google Scholar] [PubMed]
- Murray CJ, Frenk J. Health metrics and evaluation: Strengthening the science. The Lancet. 2008;371(9619):1191-1199.
[Crossref] [Google Scholar] [PubMed]
- Audibert M, Brun JF, Mathonnat J, Henry MC. Effets économiques du paludisme sur les cultures de rente: l’exemple du café et du cacao en Côte d’Ivoire. Revue d’économie du développement. 2009;(1):145-166.
- Laditka JN, Laditka SB, Probst JC. Health care access in rural areas: Evidence that hospitalization for ambulatory care-sensitive conditions in the United States may increase with the level of rurality. Health and place. 2009;15(3):761-770.
[Crossref] [Google Scholar] [PubMed]
- McGrail MR, Humphreys JS. A new index of access to primary care services in rural areas. Australian and New Zealand journal of public health. 2009;33(5):418-423.
[Crossref] [Google Scholar] [PubMed]
- Hausdorf K, Rogers C, Whiteman D, Newman B, Coxeter P, Youl P, et al. Rating access to health care: Are there differences according to geographical region? Australian and New Zealand journal of public health. 2008;32(3):246-249.
[Crossref] [Google Scholar] [PubMed]
- Salze P, Banos A, Oppert JM, Charreire H, Casey R, Simon C, et al. Estimating spatial accessibility to facilities on the regional scale: An extended commuting-based interaction potential model. International journal of health geographics. 2011;10:1-6.
[Crossref] [Google Scholar] [PubMed]
- Sibley LM, Weiner JP. An evaluation of access to health care services along the rural-urban continuum in Canada. BMC health services research. 2011;11(1):1-1.
[Crossref] [Google Scholar] [PubMed]
- Champagne F, Contandriopoulos AP, Ste-Marie G, Chartrand E. L’accessibilité aux services de santé et aux services sociaux au Québec. 2018:1-48.
- Arcury TA, Preisser JS, Gesler WM, Powers JM. Access to transportation and health care utilization in a rural region. The Journal of Rural Health. 2005;21(1):31-38.
[Crossref] [Google Scholar] [PubMed]
- Jordan H, Roderick P, Martin D, Barnett S. Distance, rurality and the need for care: access to health services in South West England. International journal of health geographics. 2004;3(1):1-9.
[Crossref] [Google Scholar] [PubMed]
- Al-Taiar A, Clark A, Longenecker JC, Whitty CJ. Physical accessibility and utilization of health services in Yemen. International journal of health geographics. 2010;9:1-8.
[Crossref] [Google Scholar] [PubMed]
- Farrington J, Farrington C. Rural accessibility, social inclusion and social justice: Towards conceptualisation. Journal of Transport geography. 2005;13(1):1-2.
- Girard JP. Our health system differently. Groupe Fides Inc. 2017.
- Bentham G, Haynes R. Health, personal mobility and the use of health services in rural Norfolk. Journal of rural studies. 1985;1(3):231-239.
- Fone DL, Christie S, Lester N. Comparison of perceived and modelled geographical access to accident and emergency departments: A cross-sectional analysis from the Caerphilly Health and Social Needs Study. International journal of health geographics. 2006;5:1-10.
[Crossref] [Google Scholar] [PubMed]
- Pagano E, Di Cuonzo D, Bona C, Baldi I, Gabriele P, Ricardi U, et al. Accessibility as a major determinant of radiotherapy underutilization: a population based study. Health policy. 2007;80(3):483-491.
[Crossref] [Google Scholar] [PubMed]
- Gao S, Manns BJ, Culleton BF, Tonelli M, Quan H, Crowshoe L, et al. Access to health care among status Aboriginal people with chronic kidney disease. Cmaj. 2008 Nov 4;179(10):1007-1012.
[Crossref] [Google Scholar] [PubMed]
- Duplessis V, Beshiri R, Bollman RD, Clemenson H. Rural and small town Canada analysis bulletin. 2002; 3(3):1-17.
- Joseph AE, Phillips DR. Accessibility and utilization: Geographical perspectives on health care delivery. J R Coll Gen Pract. 1984;34(265): 452.
- Kindig DA, Schmelzer JR, Hong W. Age distribution and turnover of physicians in nonmetropolitan counties of the United States. Health services research. 1992;27(4):565.
[Google Scholar] [PubMed]
- Atmore C. Population need and geographical access to general practitioners in rural New Zealand. The New Zealand Medical Journal. 2004;117(1201):U1063.
[Google Scholar] [PubMed]
- Rosenthal MB, Zaslavsky A, Newhouse JP. The geographic distribution of physicians revisited. Health services research. 2005;40(6p1):1931-1952.
[Crossref] [Google Scholar] [PubMed]
- Guagliardo MF. Spatial accessibility of primary care: Concepts, methods and challenges. International journal of health geographics. 2004;3(1):1-3.
[Crossref] [Google Scholar] [PubMed]
- Luo W. Using a GIS-based floating catchment method to assess areas with shortage of physicians. Health and place. 2004;10(1):1-1.
[Crossref] [Google Scholar] [PubMed]
- Huff DL. Don’t misuse the Huff model in GIS. Business Geographies. 2000;8(8):12.
- Luo W, Whippo T. Variable catchment sizes for the two-step floating catchment area (2SFCA) method. Health & place. 2012;18(4):789-795.
[Crossref] [Google Scholar] [PubMed]
- Langford M, Higgs G. Measuring potential access to primary healthcare services: The influence of alternative spatial representations of population. The Professional Geographer. 2006;58(3):294-306.
- Radke J, Mu L. Spatial decompositions, modeling and mapping service regions to predict access to social programs. Geographic Information Sciences. 2000;6(2):105-112.
- Luo W, Wang F. Measures of spatial accessibility to health care in a GIS environment: Synthesis and a case study in the Chicago region. Environment and planning B: planning and design. 2003;30(6):865-884.
[Crossref] [Google Scholar] [PubMed]
- Bauer J, Groneberg DA. Measuring spatial accessibility of health care providers–introduction of a variable distance decay function within the floating catchment area (FCA) method. PloS one. 2016;11(7):e0159148.
[Crossref] [Google Scholar] [PubMed]
- Donohoe J, Marshall V, Tan X, Camacho FT, Anderson RT, Balkrishnan R. Spatial access to primary care providers in Appalachia: Evaluating current methodology. Journal of Primary Care & Community Health. 2016;7(3):149-158.
[Crossref] [Google Scholar] [PubMed]
- Luo W, Qi Y. An enhanced two-step floating catchment area (E2SFCA) method for measuring spatial accessibility to primary care physicians. Health & place. 2009;15(4):1100-1107.
[Crossref] [Google Scholar] [PubMed]
- McGrail MR. Spatial accessibility of primary health care utilising the two step floating catchment area method: An assessment of recent improvements. International journal of health geographics. 2012;11(1):1-2.
[Crossref] [Google Scholar] [PubMed]
- Roeger LS, Reed RL, Smith BP. Equity of access in the spatial distribution of GPs within an Australian metropolitan city. Australian Journal of Primary Health. 2010;16(4):284-290.
- Wan N, Zou B, Sternberg T. A three-step floating catchment area method for analyzing spatial access to health services. International Journal of Geographical Information Science. 2012;26(6):1073-1089.
- Zaugg V, Savoldelli V, Sabatier B, Durieux P. Improving practice and organization of care: methodology for systematic reviews. Sante Publique. 2014;26(5):655-667.
[Crossref] [Google Scholar] [PubMed]
- Xiao Y, Watson M. Guidance on conducting a systematic literature review. Journal of planning education and research. 2019;39(1):93-112.
- Begg C, Cho M, Eastwood S, Horton R, Moher D, Olkin I, et al. Improving the quality of reporting of randomized controlled trials: the CONSORT statement. Jama. 1996;276(8):637-639.
[Crossref] [Google Scholar] [PubMed]
- Moher D, Schulz KF, Altman DG, CONSORT Group. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomized trials. Annals of internal medicine. 2001;134(8):657-662.
[Crossref] [Google Scholar] [PubMed]
- Amiri S, Espenschied JR, Roll JM, Amram O. Access to primary care physicians and mortality in Washington state: Application of a 2‐step floating catchment area. The Journal of Rural Health. 2020;36(3):292-299.
[Crossref] [Google Scholar] [PubMed]
- Barrett O. Measuring Accessibility to Primary Health Care Across the Urban-rural Continuum in the Province of Alberta. 2016.
- Bauer J, Müller R, Brüggmann D, Groneberg DA. Spatial accessibility of primary care in England: A cross‐sectional study using a floating catchment area method. Health Services Research. 2018;53(3):1957-1978.
[Crossref] [Google Scholar] [PubMed]
- Bell S, Wilson K, Shah TI, Gersher S, Elliott T. Investigating impacts of positional error on potential health care accessibility. Spatial and spatio-temporal epidemiology. 2012;3(1):17-29.
[Crossref] [Google Scholar] [PubMed]
- Bell S, Wilson K, Bissonnette L, Shah T. Access to primary health care: does neighborhood of residence matter? Annals of the Association of American Geographers. 2013;103(1):85-105.
- Bissonnette L, Wilson K, Bell S, Shah TI. Neighbourhoods and potential access to health care: The role of spatial and aspatial factors. Health and place. 2012;18(4):841-853.
[Crossref] [Google Scholar] [PubMed]
- Crooks VA, Schuurman N. Interpreting the results of a modified gravity model: examining access to primary health care physicians in five Canadian provinces and territories. BMC Health Services Research. 2012;12(1):1-3.
[Crossref] [Google Scholar] [PubMed]
- Cui Y. A GIS-based approach to the characterization of spatial accessibility to primary health care facilities in the Melbourne metropolitan area. Dissertation. RMIT University; 2014.
- Dewulf B, Neutens T, De Weerdt Y, Van de Weghe N. Accessibility to primary health care in Belgium: An evaluation of policies awarding financial assistance in shortage areas. BMC Family Practice. 2013;14(1):1-3.
[Crossref] [Google Scholar] [PubMed]
- Higgs G, Zahnow R, Corcoran J, Langford M, Fry R. Modelling spatial access to general practitioner surgeries: Does public transport availability matter? Journal of Transport & Health. 2017;6:143-154.
- Langford M, Higgs G, Fry R. Multi-modal two-step floating catchment area analysis of primary health care accessibility. Health & place. 2016;38:70-81.
[Crossref] [Google Scholar] [PubMed]
- Naylor KB, Tootoo J, Yakusheva O, Shipman SA, Bynum JP, Davis MA. Geographic variation in spatial accessibility of US healthcare providers. Plos one. 2019;14(4):e0215016.
[Crossref] [Google Scholar] [PubMed]
- Ngui AN, Apparicio P. Optimizing the two-step floating catchment area method for measuring spatial accessibility to medical clinics in Montreal. BMC health services research. 2011;11(1):1-2.
[Crossref] [Google Scholar] [PubMed]
- Shah TI, Bath B, Milosavljevic S. Comparing geographical distribution of community‐based physiotherapists and family physicians across Saskatchewan. The Canadian Geographer/Le Géographe Canadien. 2015;59(4):461-473.
- Shah TI, Milosavljevic S, Bath B. Measuring geographical accessibility to rural and remote health care services: Challenges and considerations. Spatial and spatio-temporal epidemiology. 2017;21:87-96.
[Crossref] [Google Scholar] [PubMed]
- Shah TI, Milosavljevic S, Bath B. Determining geographic accessibility of family physician and nurse practitioner services in relation to the distribution of seniors within two Canadian Prairie Provinces. Social Science and Medicine. 2017;194:96-104.
[Crossref] [Google Scholar] [PubMed]
- Shah TI, Clark AF, Seabrook JA, Sibbald S, Gilliland JA. Geographic accessibility to primary care providers: Comparing rural and urban areas in Southwestern Ontario. The Canadian Geographer/Le Géographe canadien. 2020;64(1):65-78.
- Schuurman N, Berube M, Crooks VA. Measuring potential spatial access to primary health care physicians using a modified gravity model. The Canadian Geographer/Le Geographe Canadien. 2010;54(1):29-45.
- Subal J, Paal P, Krisp JM. Quantifying spatial accessibility of general practitioners by applying a modified huff three-step floating catchment area (MH3SFCA) method. International Journal of Health Geographics. 2021;20:1-4.
[Crossref] [Google Scholar] [PubMed]
- Wang F, Luo W. Assessing spatial and non-spatial factors for healthcare access: Towards an integrated approach to defining health professional shortage areas. Health & place. 2005;11(2):131-146.
[Crossref] [Google Scholar] [PubMed]
- Whitehead J, Pearson AL, Lawrenson R, Atatoa-Carr P. Defining general practitioner and population catchments for spatial equity studies using patient enrolment data in Waikato, New Zealand. Applied Geography. 2020;115:102137.
[Crossref] [Google Scholar]
- Dalmas L, Leandri M, Rouzier R, Héquet D. Environmental costs linked to transport in the economic evaluation of a care pathway: Application to the management of breast cancer in the west of the Paris region. Journal of Regional and Urban Economy. 2022;(4):563-586.
Citation: Simoneau C (2023) Underserved Rural Areas: A Systematic Review of Primary Care Geographical Access using Gravity Models. J Remote Sens GIS. 12:312.
Copyright: © 2023 Simoneau C. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.