Indexed In
- Academic Journals Database
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Scimago
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- MIAR
- University Grants Commission
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Review Article - (2020) Volume 0, Issue 0
Twenty Years of Coronaviruses
Divya Tandon*Received: 18-Sep-2020 Published: 14-Oct-2020, DOI: 10.35248/2157-7560.20.S4.004
Abstract
Coronaviruses have formerly been considered as quite harmless respiratory viruses for humans. After two previous outbreaks of severe respiratory tract infection, caused by two different coronavirus namely the Severe Acute Respiratory Syndrome Coronavirus (SARS-CoV) and the Middle East Respiratory Syndrome Coronavirus (MERSCoV), this is the third time when a totally different type of coronavirus named as COVID-19 emerges and infect human population all over the World. This virus originated in bats and was transmitted to humans through some unknown intermediate species in Wuhan, Hubei province, China in December 2019. The infection of COVID-19 transmits by inhalation or contact with aerosols of infected patient and the incubation period vary from 2 days to 14 days. The symptoms disease are mild in most people and includes Sore throat, cough, fever and fatigue but in some patients (usually the elderly and those with some underlying disease), it may progress to pneumonia, Acute Respiratory Distress Syndrome (ARDS) and multiple organ dysfunction or failure. All these facts brought coronaviruses globally to limelight and also highlighted the necessity of controlling these pathogens.
Keywords
SARS; MERS; COVID-19; ARDS
Introduction
The new coronavirus family member that is named as 2019 novel coronavirus (2019-nCoV) or the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) is rapidly spreading across the globe [1]. Till 06 June 2020 around 6.54 M cases of COVID-19 and 387 K deaths have been reported [2]. India has reported 237 K cases till date. Fortunately so far, In India children have been infrequently affected with no deaths. But some children develop Kawasaki disease like symptoms linked with COVID-19 infection. This article gives panorama about this newly emerged virus.
History
Coronaviruses are largest group of single stranded positive sense RNA viruses that are 125 nm in diameter [3] enveloped, no segmented and composed of four genera (alpha, beta, gamma and delta) [4]. Viral genome contains four proteins namely Membrane [M], Spike [S], Envelope [E] and Nucleocapsid [N] proteins. Among these the spike protein plays the most important role in entry of virus. The Spike protein is the main protein that assists the virus in receptor-binding and its subsequent entry into host cells, and is therefore considered as the major therapeutic target [5]. The Membrane and Envelope proteins play major function in viral assembly, and the Nucleocapsid protein is necessary for RNA synthesis [6].
At the time of initial outburst of Severe Acute Respiratory Syndrome (SARS), very little knowledge about these coronaviruses and their pathogenesis is available to the researchers and they are thought to be the pathogens causing only mild illnesses, such as the common cold [7]. In the year 2003 after SARS pandemic [8], it became clear to the Scientific World that these are not ordinary viruses but they can because deadly infections among humans. Therefore, attention should be given to these new pathogens. The SARS-CoV outbreak started in Guangdong, China, and spread too many countries in Southeast Asia, North America, Europe, and South Africa. SARS CoV after infecting about 8000 people and after taking lives of around 774 patients finally disappeared in 2004. But later it was found that SARS-CoV like infections was seen in bats. It was further demonstrated that these viruses infecting bats have the ability to infect humans also and possibility of the re-emergence of SARS-CoV or SARS-CoV-like viruses.
About nine years later in June 2012 another highly infectious and novel coronavirus appeared in Middle East. This coronavirus also causes respiratory illness and was known as MERS-CoV. MERSCoV was first isolated from the sputum of a male patient who died from acute pneumonia and renal failure in Saudi Arabia [9]. Symptoms associated are non-specific but many patients lost their lives with severe respiratory distress. These patients usually have a travel history and that led to its transmission outside Arabian Penninsula and soon it becomes Global concern [10]. Similar to SARS-CoV, health professionals are the frontliners and are at higher risk of acquiring the infection [11]. However, in comparison with SARS-CoV, the case fatality rate associated with MERS-CoV is much higher. But one major difference exist between these two coronaviruses is that one SARS-CoV infected patient can transmit the disease to approximately four other people but a MERS-CoV infected patient can only infect one person. Both SARS and MERS share similar features like nosocomial mode of transmission, replication in lower respiratory tract.
MERS-CoV possesses larger genome and eight accessory proteins while SARS-CoV has a relatively small genome size and five accessory proteins [12]. These features enable these viruses to evade the host immune system by majorly affecting the innate immune response [13].
Origin of Covid-19
In December 2019, third time a different zoonotic virus emerged that has crossed the species to infect humans. This virus has first reported in Wuhan, China where a cluster of patients developed pneumonia with unknown ethology as reported by the WHO. This virus was provisionally named as 2019-nCoV and then named as novel COVID-19 virus by WHO in February 2020. This virus was initially found different from the last two viruses of coronavirus family and the respiratory disease that this virus causes is much more severe than SARS and MERS CoV [14]. But later studies revealed that the genome sequence of the virus is 75% to 80% identical to the SARS-CoV and even it is show more resemblance to several coronaviruses causing disease in bats [15]. Firstly it was reported by WHO that human-to human transmission was limited or don’t exist, but we now know that such transmission occurs where an infected person can infect the whole community also. This newer version of coronavirus has infected more people than either of its two predecessors. The reason for its rapid spread is that Wuhan from where it is emerged is the major transportation hub of China which increases transmission of this virus from one person to other and also increases the possibility of its transmission to other locations. The genome sequence of the virus is 75% to 80% identical to the SARS-CoV and even it is show more resemblance to several coronaviruses causing disease in bats [15]. The symptoms of COVID-19 include fever, dry cough, and shortness of breath and, in the most critical cases, patient develops pneumonia. The case fatality rate is around 2% to 3%. COVID-19 will cause many more deaths than previous two viruses, even though the mortality rate is lower than MERS-CoV infections. According to a report published by COVID-19 can grow on same cells that are useful for growing SARS-CoV and MERS-CoV but their propagation is much better and rapid in primary human airway epithelial cells [10]. The WHO declared this disease to be a public health emergency of international concern, characterized as a pandemic.
A Public Health Emergency of International Concern (PHEIC) is a formal declaration released by the emergency committee of the WHO in context to an extraordinary episode that will affect global health security and may require coordinated international response. The intention of declaring a PHEIC by the WHO is to prevent the spread of disease internationally and to avoid unnecessary interference with international dealings and trade (Table 1).
| Category | SARS | MERS | COVID-19 |
|---|---|---|---|
| Year of origin | Nov-02 | Jun-12 | Dec-19 |
| Place of origin | China | Saudi Arabia | Wuhan, China |
| Spread | Animal to human first and then human to human. | Animal to human first and then human to human. | Animal to human first and then human to human. |
| Mode of transmission | Airborne, Contact with infected patient. | Airborne, Contact with infected patient. | Airborne, Contact with infected patient. |
| Time for which epidemic remains | 8 months | >39 months | N/A |
| Patient to healthcare worker spread | Present | present | present |
| Status | No cases left | Few cases left | Active |
| Incubation time | 2-14 days | 2-15 days | 4-7 days |
| Host | Bats | Bats | Bats |
| Intermediate host | Civets | Camels | Not known |
| Genome Size | 27.9Kb | 30.1 Kb | 29.9 Kb |
| Receptor | ACE2 | DPP4 | ACE2 |
| Major symptoms | Fever, cough, fatigue, and shortness of breath | Fever, cough, fatigue, shortness of breath, and acute renal failure | Fever, cough, fatigue, and shortness of breath |
| Severe symptoms | Sepsis and septic shock. | Sepsis and septic shock. | Sepsis and septic shock. |
| Lab tests | Abnormal blood counts, abnormal coagulation, multiple organ dysfunction, cytokine storm. | Abnormal blood counts, abnormal coagulation, multiple organ dysfunction, cytokine storm. | Abnormal blood counts, abnormal coagulation, multiple organ dysfunction, cytokine storm. |
| Primary treatment approach. | Early supportive therapy and monitoring | Early supportive therapy and monitoring | Early supportive therapy and monitoring |
| Available treatment | No treatment | No treatment | No treatment yet. |
| Vaccine | No Vaccine | No Vaccine | No Vaccine yet. |
Table 1: Differences between SARS, MERS and COVID-19.
Epidemiology
In December 2019, a cluster of 27 pneumonia cases with unknown etiology were reported in Wuhan, the capital of Hubei province, China. Out of these 27 patients, 7 were severe cases as reported by Wuhan Municipal Health Committee. The only thing common between all these patients is their link with Huanan Seafood Wholesale Market in Wuhan [16]. Later, from these patients a new strain of coronavirus was isolated which was different from SARS-CoV and MERS-CoV, although it shows >70% sequence similarity with SARS-CoV.
Since the COVID-19 infection starts from China, so important epidemiological risks include travel history from Wuhan or contact with a patient suffering from COVID-19 infection. Environmental samples were also tested positive from the Huanan sea food market that signifies that virus originates from China [16]. The number of cases started spreading like a bomb, with some of the cases that have no history of exposure to animal market, suggestive of the fact that human-to-human transmission of this coronavirus was occurring [17]. The main transmission route of transmission of COVID-19 is respiratory droplets or contact [18]. The respiratory droplets can spread 1-2 m and deposit on the surface. Studies have shown that nasal cavity has higher viral load as compared to the throat and there is no difference in viral burden between symptomatic and asymptomatic people [19]. Other possible routes include aerosol or oral-faecal transmission. Elderly patients and those with any underlying diseases are more susceptible to COVID-19 infection. Children especially below 10 years, infants, and pregnant women are also reported to have COVID-19 infection [14-18]. Soon it was also clear that the a. symptomatic cases also act as carriers to transmit the infection. Based on the first 425 confirmed cases, the mean incubation period of the virus calculated is 5.2 days, with a 95th percentile distribution of 12.5 days, and its basic reproductive number is 2.2, which is lower than the 3.0 for SARS-CoV [19]. Also the reproductive number (R0) that is the average number of people that will catch infection from a single infected patient is 1.4–6.47 for COVID-19 [20]. In comparison to this the R0 of SARS-CoV and MERS-CoV is 0.3–1.3 and 2.2–3.7, respectively, that indicates higher transmission capacity of COVID-19 [21]. Primary strategy to limit the spread of COVID-19 infection is isolation and quarantine of infected individuals.
Virology
Coronaviruses are single stranded enveloped, positive-sense RNA viruses. Coronavirus family is further divided into 4 groups, namely alpha, beta, gamma, and delta coronavirus. Several groups are zoonotic viruses that typically causes respiratory and/or digestive tracts illness in mammals including humans [22]. Till now there are 7 coronavirus species discovered and these are HCoV-229E, HCoV-OC43, HCoV-NL63, HCoV-HKU1, SARS-CoV, MERSCoV, and COVID-19. Genetic evolutionary analyses have revealed that COVID-19 is a Beta coronavirus belonging to the Sarbecovirus subgenus of the Coronaviridae family, which is different from its precursors [23,24]. COVID-19 has 86.9% to 96% genome similarity to various variants of bat SARS-like coronaviruses, such as ZC45, ZXC21, and RaTG3 [25]. The cytopathic effects induced by COVID-19 are different from SARS-CoV and MERS-CoV (Figure 1).
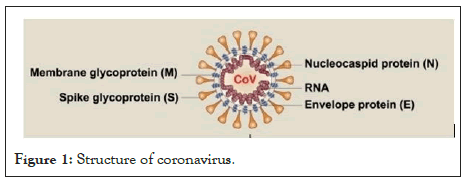
Figure 1: Structure of coronavirus.
The genome of COVID-19 has 10-12 putative Open Reading Frames [25,26]. ORF1 encodes Non-Structural Proteins (NSP). These are multifunctional proteins which are involved in virus processing and replication. The remaining ORFs encodes for viral structural proteins like Spike [S], Envelope [E], Membrane [M], and Nucleocapsid [N]) proteins [25]. During infection Spike protein is cleaved into two subunits: S1 and S2. S1 subunit contains Receptor Binding Doaminwhile S2 subunit contains fusion machinery. These structural proteins help in assembling and releasing new viral copies. The receptor for COVID-19 entry into humans is Angiotensin I-Converting enzyme 2 (ACE2). When COVID-19 infects any individual, its S1 subunit first binds to ACE2 receptor on the host cell surface and then S2 subunit fuses viral and host membranes (Figure 2) [13].
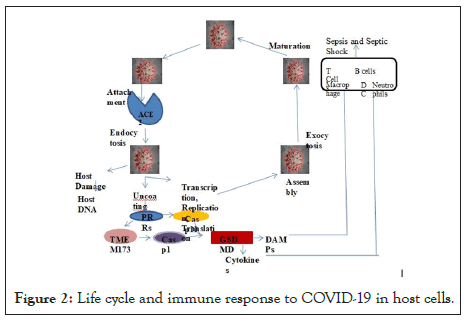
Figure 2: Life cycle and immune response to COVID-19 in host cells.
ACE2 is the host cell receptor that play major role in mediating infection by COVID-19. After endocytosis and subsequent uncoating of virus, the components of COVID-19 can be further used to produce new virus. After this, the virus is released from the host cell by exocytosis. On the other hand, COVID-19 mediated damage of host DNA or the components of COVID-19 can bind various cytosolic PRRs, that leads to the activation of TMEM173 or GSDMD-dependent pyroptosis, which causes release of cytokine and DAMP and this results in inflammation, immunity, and coagulation dysfunction through impairment of various immune cells, like T cells, B cells, dendritic cells, NK cells, macrophages, and neutrophils. This process is involved in the activation of transcription factors, such as IRF3 and NF-κB. If not managed early, it can lead to septic shock, multiple organ failure, and even death [27].
Clinical Features
The clinical presentation of COVID-19 ranges from asymptomatic stage to respiratory distress, multiple organ failure and death. The clinical sign and symptoms are more or less like other respiratory infections like ones caused by SARS and MERs CoV. The common clinical features associated with COVID-19 infection are fever, dry cough, sore throat, fatigue, headache and breathlessness [22,24,28]. The WHO recently added two more symptoms which are loss of smell and loss of taste.
The progression of infection is associated with paramount rise in inflammatory cytokines like IL2, IL7, IL10, GCSF, IP10, MCP1, MIP1A, VEGF and TNFα [29]. The time from onset of symptoms to breathlessness was 5 days, hospitalization 7 days and acute respiratory distress 8 days. Adverse outcomes and deaths are more common in the older patients and those with any underlying disease [30].
Some recent studies have also reported that fever and dry cough are among most common symptoms but some patients remains asymptomatic [28,31].
Diagnosis
The suspected case of COVID-19 is one who has symptoms like fever, sore throat, dry cough or any abroad travel history or contact with confirmed COVID-19 cases. However some cases may be asymptomatic. Infection is only confirmed with a positive molecular test on respiratory samples (throat swab, nasopharyngeal swab, sputum, endotracheal aspirate).
Some COVID-19 infected patient’s blood test report showed decreased or normal white blood cell count, decreased lymphocyte count, increased prothrombin time, increased aspartate aminotransferase, creatinine, creatine kinase, and lactate dehydrogenase etc. All these findings altogether represent coagulation abnormalities and organ dysfunctioning.
The chest X-ray usually presents with bilateral infiltrates but it may be normal in early disease. CT imaging usually shows bilateral patchy shadows or ground glass opacity in the lungs (Table 2) [32].
| Clinical Presentation |
Wang N=138 |
Chen N= 99 |
Guan N= 1099 |
|---|---|---|---|
| Cough | 59.40% | 82% | 67.70% |
| Fever | 98.60% | 83% | 43.10% |
| Fatigue | 69.60% | NA | 38% |
| Dysnea | 31% | 31% | 18.70% |
| Myalgia | 34% | 11% | 14% |
| Diarrheal | 10% | 2% | 3% |
| Dizziness | 9.40% | NA | NA |
| Nausea | 14% | 1% | 5% |
| Anorexia | 39.90% | NA | NA |
| Expectoration | 26.80% | NA | 33.40% |
| Headache | 6.50% | 8% | 13.60% |
| Abdominal Pain | 2.20% | NA | NA |
| ICU Care | 26.10% | NA | 5% |
| Mortality | 4.30% | 11% | 1.36% |
Table 2: Clinical Presentation of COVID-19 patients.
Differential Diagnosis
The differential diagnosis of COVID-19 includes all the respiratory viral infections (like influenza, parainfluenza, adenovirus, human metapneumovirus etc.), mycoplasma infection and bacterial infection. Although it is very difficult to differentiate these infections with COVID-19 infection either clinically or through regular lab tests. So the suspects with some or more COVID-19 symptoms are test for specific coronavirus tests.
Clinical Management
COVID-19 infection ranges from mild illness to severe respiratory illness. Severe illness can lead to Acute Respiratory Distress Syndrome, septic shock or death. WHO released the guidelines for management of novel COVID-19 infection, although countries made some updates in guidelines at their part the management of COVID-19 according to the WHO include:
1. Screening of suspects for early recognition of infection.
2. Immediate implementation of measures for Infection Control and Prevention.
3. Specimen collection for laboratory diagnosis.
4. Management of patients with mildCOVID-19 infection: their treatment and monitoring.
5. Management of severe cases: oxygen therapy and monitoring.
6. Management of Critical patients: ARDS.
7. Prevention of complications associated.
8. Management of Septic shock.
9. Caring of pregnant women’s with infection.
10. Care of infants and breast feeding mothers.
11. Care for older patients with COVID-19 infection.
12. Clinical research and specific anti–COVID-19 treatments [33,34].
All these guidelines are released by the WHO for effective screening, diagnosis and management of patients mild to severe COVID-19 infection. One thing should be noted here that our utmost attention should be on transmission of infection from COVID-19 patients to healthcare workers.
WHO declared COVID-19 as International Public Health Emergency because COVID-19 is an emerging virus and there is no drug or vaccine available for its cure. Till now the treatment is only supportive care, fluid management, antibiotic treatment and oxygen level maintenance in critical patients. Besides this several antiviral drugs, human monoclonal antibodies are still under clinical trials but none is so far successful in the treatment of COVID-19 infection. For example firstly in China combination of two antiviral drugs lopinavir-ritonavir which are used in HIV infected patients is found efficient in COVID-19 patients but later it was found that the benefits of these two drugs are not much [35]. Other drug is Remdesivir that has initially shown promise in treating some patients but the results of ongoing randomized placebo-controlled trials are still not known [36]. Similarly, antibacterial drugs like moxifloxacin, azithromycin, ceftriaxone also failed to provide treatment benefits for COVID-19 patients. Thus the need of the hour is to focus on improved therapies like targeted therapy and vaccine development.
Recently Dexamethasone which is an anti-inflammatory low cost drug reported to reduce the death among one third patients admitted in hospital with acute respiratory complications of COVID-19. UK government authorized this drug on 17th June 2020.
Besides various pharmaceutical companies like Modern, Pfizer, Sino vac Biotech of China, UK Oxford’s Astrazeneca have promised to give the vaccines for COVID-19 by the end of this year.
Possible Therapeutic Targets
Due to severe infection of COVID-19, there is uncontrolled immune response and subsequent sepsis as a result of host response to virus. This leads to immediate release of various immune mediators, especially cytokines and Damage-Associated Molecular Patterns (DAMPs) [37,38]. Keeping all this in mind the treatment strategy may include developing antibodies or inhibitors to block the interplay between COVID-19 and the host ACE2 receptor and administering passive antibodies isolated from serum of COVID-19 patients. Possible immunopathological targets are:
Host cell death
The present study was conducted in Morogoro, Tanzania (6.8278°S, 37.6591°E) at Sokoine University of Agriculture (SUA) in a vector controlled Animal Biosafety Level 2 (ABSL-2) facility and a Biosafety Level 2 (BSL-2) virology laboratory. The animal facility is designed to prevent the entry of arthropods and to provide sanitation measures as well as being equipped with incinerator for disposing animal animal waste. The laboratory is equipped with basic virology and cell culture instruments together with a distiller and an autoclave for autoclaving equipment before use and autoclaving waste materials from the laboratory before exposing the waste to the environment.
Study area
• Among different types of Regulated Cell Death, pyroptosis is the most widely studied type in various infectious diseases including viral infections.
• Caspase 1 and Caspase 11 leads to activation of pyroptosis.
• Activation of pyroptosis leads to cleavage of gasdermin D (GSDMD) that produces an N-terminal domain.
• This N terminal domain (GSDMD-N) triggers cell death and release of pro-inflammatory cytokines and DAMPS.
• So, this GSDMD-N can serve as therapeutic target for infectious diseases like COVID-19 [36].
Damps
1. Damage Associated Molecular Pattern is endogenous molecules released/secreted by cytokines.
2. Among them HMGB1, an important target in several human diseases and pathologic conditions, especially critical illness and septic shock [36]. HMGB1 already proved as potential therapeutic target for SARS CoV infection, so we therefore hypothesize that this may also play a similar protective role in COVID-19 by mediating inflammation and immune dysfunction.
3. Various drugs like chloroquine, an antimalarial drug and Glycyrrhizin work by inhibiting HMGB1 [36].
Important Points to Follow in Indian Scenario to Prevent COVID-19 Infection
• Till now there is no treatment or vaccine available for COVID-19, so prevention of disease using self-safety measures is the only option.
• Although the prevention is also not so easy in this case due to several properties of this virus like non-specific features of the disease, infectivity before onset of symptoms, some patients are asymptomatic but still they can transmit disease, prolonged duration of illness and transmission after recovery from the infection.
• So, home isolation of suspected/confirmed cases with mild symptoms is recommended. For home isolation requirement is proper ventilation, attached toilet with the patient’s room, patient should wear surgical mask and practice cough hygiene. Also the caregiver should wear mask and follow hand hygiene.
• Special attention should be given to protect the healthcare workers to ensure continuity of care and to prevent transmission of infection to other patients.
• At community levels, peoples should be asked not to gather in groups, maintain social distancing protocols. Always wear masks in crowded areas. Practice cough hygiene is also very important. Patients who have respiratory symptoms should be asked to use surgical masks.
Conclusion
COVID-19 is highly pathogenic third member of Coronavirus family that emerged in Wuhan and spread around the World. Among all the types of Coronaviruses this is the most contagious one. This novel coronavirus seems to follow the same host cell entry via receptor—ACE2—similar to SARS-CoV. Every virus has a property to change continuously as the result of natural selection. Keeping the same in mind if we collect epidemiological history and molecular profiles of patients suffering from COVID-19 infection we can get an idea about its evolution and this will help in developing preventive measures and treatment strategies for this viral infection. Patients with mild symptoms usually recover without much treatment, only those with severe symptoms require ICU care. Drug Repuposing may be an emerging strategy against COVID-19 as different pathogenic infections involve same molecular pathways. Random trials in patients on a large scale are required. Finally, the long-term impact of this pandemic on individual, national, and international levels remains to be evaluated after the end of this war with COVID-19.
Acknowledgements
The authors would like to thank Indian Council of Medical Research (ICMR), University Grant Commission (UGC), New Delhi, India and Centre of Excellence, Higher Education, Government of Uttar Pradesh, Lucknow, India for financial support. DST-FIST-PURSE is duly acknowledged for Central Instrumentation Facility. DT acknowledges UGC for postdoctoral fellowship.
REFERENCES
- Wang C, Horby PW, Hayden FG, Gao F. A novel coronavirus outbreak of global health concern. The Lancet. 2020; 395: 470-473.
- Coronavirus Outbreak. 2020.
- Du L, Yang Y, Zhou Y, Lu L, Li F, Jiang S. MERS-CoV spike protein: A key target for antivirals. Expert Opin Ther Targets. 2017; 21: 131- 143.
- Du L, He Y, Zhou Y, Liu S, Zheng B, Jiang S. The spike protein of SARS-CoV—A target for vaccine and therapeutic development. Nat Rev Microbiol. 2009; 7: 226-236.
- Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020; 395: 497-506.
- Zhou P, Yang XL, Wang XG, Hu Ben, Zhang B, Zhang W, et al. Discovery of a novel coronavirus associated with the recent pneumonia outbreak in 2 humans and its potential bat origin. Nature.2020; 579: 270-273.
- Yin Y, Wunderink RG MERS. SARS and other coronaviruses as causes of pneumonia. Respirology .2018; 23: 130–137.
- Drosten C, Gunther S, Preiser W, van der Werf S, Brodt HR, Becker S, et al. Identification of a novel coronavirus in patients with severe acute respiratory syndrome. N Engl J Med .2003; 348:1967-1976.
- Wang Y, Sun J, Zhu A, Zhao J, Zhao J. Current understanding of middle east respiratory syndrome coronavirus infection in human and animal models. J Thorac Dis. 2018; 10: 2260-2271.
- Zhu N, Zhang D, Wang W, Li X, Yang B, Song J. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020; 382: 727-33.
- Xinhua. China’s CDC detects a large number of new coronaviruses in the South China seafood market in Wuhan.2020.
- Menachery V.D, Yount B.J, Debbink K, Agnihothram S, Gralinski L.E, Plante J.A, et al. A SARS-like cluster of circulating bat coronaviruses shows potential for human emergence. Nat Med. 2015; 21: 1508-1513.
- Ge XY, Li JL, Yang XL, Chmura AA, Zhu G, Epstein JH, et al. Isolation and characterization of a bat SARS-like coronavirus that uses the ACE2 receptor. Nature. 2013; 503: 535-538.
- Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020; 395(10226):809-15.
- Porcheddu R, Serra C, Kelvin D, Kelvin N, Rubino S. Similarity in Case Fatality Rates (CFR) of COVID-19/SARS-COV-2 in Italy and China. J Infect Dev Ctries. 2020; 14(2):125-128.
- Bai Y, Yao L, Wei T, Tian F, Jin DY, Chen L, et al. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020; 323(14):1406-1407.
- Wu D, Wu T, Liu Q, Yang Z. The SARS-CoV-2 outbreak: What we know. Int J Infect Dis. 2020; 94:44-48.
- Lu X, Zhang L, Du H, Zhang J, Li YY, Qu J, et al. SARS-CoV-2 Infection in Children. N Engl J Med. 2020; 383:1663-1665.
- Zou L, Ruan F, Huang M, Liang L, Huang H, Hong Z, et al. SARS- CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020; 382(12):1177-1179.
- Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ. HLH Across Speciality Collaboration. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020; 395(10229):1033.
- Matsuyama S, Nao N, Shirato K, Kawase M, Saito S, Takayama I, et al. Enhanced isolation of SARS-CoV-2 by TMPRSS2-expressing cells. Proc Natl Acad Sci U S A. 2020; 117(13):7001-3.
- Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al . Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020; 382(18):1708-1720.
- Walls AC, Park YJ, Tortorici MA, Wall A, McGuire AT, Veesler D. Structure, Function, and Antigenicity of the SARS-CoV-2 Spike Glycoprotein. Cell.2020; 281-292.e6
- Yang Y, Lu Q, Liu M, Wang Y, Zhang A, Jalali N, et al. Epidemiological and clinical features of the 2019 novel coronavirus outbreak in China. MedRxiv. 2020; 26(4):399-400.
- Wu A, Peng Y, Huang B, Ding X, Wang X, Niu P, et al. Genome composition and divergence of the novel coronavirus (2019-nCoV) originating in China. Cell Host & Microbe. 2020.
- Zaki A.M, van Boheemen S, Bestebroer T.M, Osterhaus A.D, Fouchier R.A. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N Engl J Med. 2012; 367: 1814-1820.
- Fehr A.R, Perlman S. Coronaviruses: An overview of their replication and pathogenesis. Methods Mol Biol. 2015; 1282: 1-23.
- Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020; 395.
- Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ, et al. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020; 395: 1033-1034.
- WHO. Clinical management of severe acute respiratory infection when novel coronavirus (2019-nCoV) infection is suspected. 2020.
- Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, et al. First Case of 2019 Novel Coronavirus in the United States. N Engl J Med. 2020; 10: 1056.
- Huang P, Liu T, Huang L, Liu H, Lei M, Xu W, et al. Use of chest CT in combination with negative RT-PCR assay for the 2019 Novel Coronavirus but High Clinical Suspicion. Radiology. 2020; 295(1):22-23.
- Doitsh G, Galloway NL, Geng X, Yang Z, Monroe KM, Zepeda O, et al. Cell death by pyroptosis drives CD4 T-cell depletion in HIV-1 infection. Nature. 2014; 505(7484):509-14.
- Wu F, Zhao S, Yu B, Chen YM, Wang W, Song ZG, et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020; 579(7798):265-9.
- Zhang H, Zeng L, Xie M, Liu J, Zhou B, Wu R, et al. TMEM173 drives lethal coagulation in sepsis. Cell Host Microbe. 2020; 27(4):556-70.
- Kang R, Chen R, Zhang Q, Hou W, Wu S, Cao L, et al. HMGB1 in health and disease. Mol Aspects Med. 2014; 40:1-116.
- Chan JF, Kok KH, Zhu Z, Chu H, To KK, Yuan S, et al. Genomic characterization of the 2019 novel human-pathogenic coronavirus isolated from a patient with atypical pneumonia after visiting Wuhan. Emerg Microbes Infect. 2020; 9(1):221-36.
- Tang D, Comish P, Kang R. The hallmarks of COVID-19 disease. Plos Pathog.2020; 16(5): e1008536.
Citation: Tandon D (2020) Twenty Years of Coronaviruses. J Vaccines Vaccin. S4:004. DOI: 10.35248/2157-7560.20.S4.004
Copyright: © 2020 Tandon D. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

