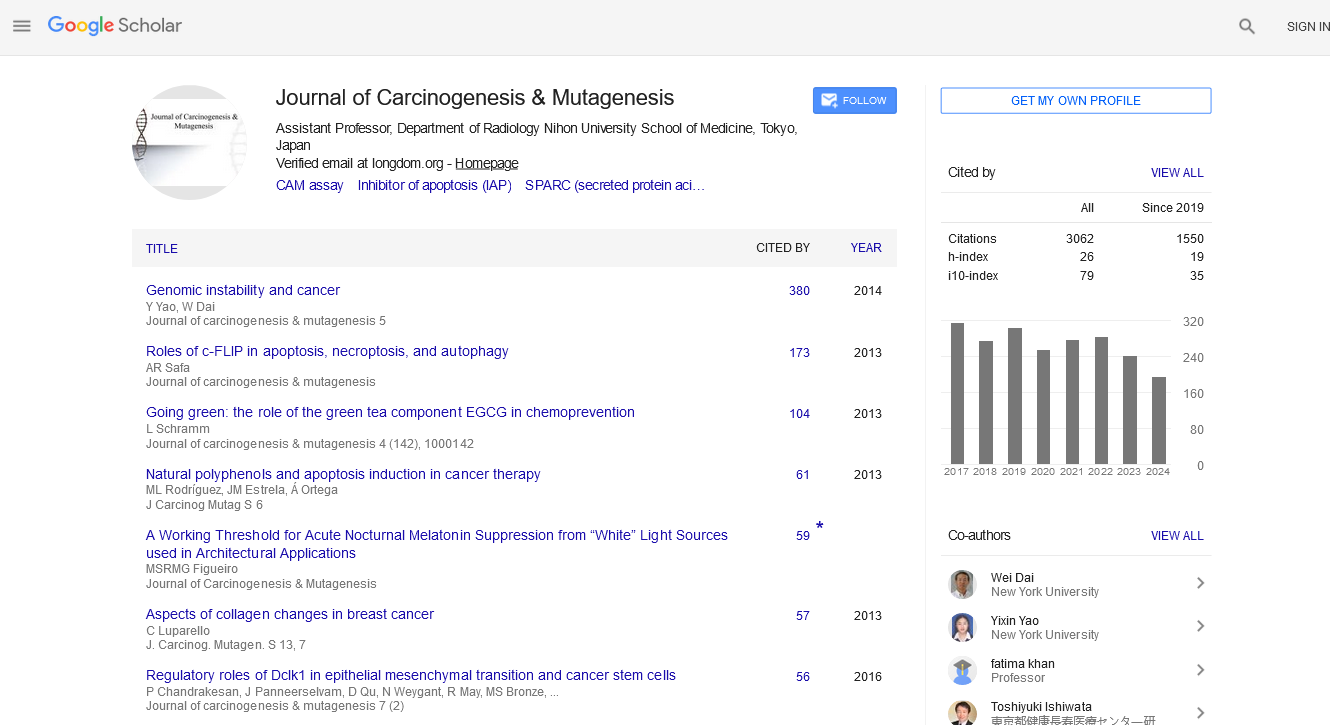
Indexed In
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Short Communication - (2024) Volume 0, Issue 0
Treatment Resistance: Understanding the Neoadjuvant Chemotherapy in Rectal Cancer
Vanessa Scotti*Received: 02-Apr-2024, Manuscript No. JCM-24-25645; Editor assigned: 05-Apr-2024, Pre QC No. JCM-24-25645 (PQ); Reviewed: 19-Apr-2024, QC No. JCM-24-25645; Revised: 25-Apr-2024, Manuscript No. JCM-24-25645 (R); Published: 02-May-2024, DOI: 10.35248/2157-2518.24.S43.005
Description
Rectal cancer, a formidable opponent in the field of oncology, often necessitates a multi-faceted treatment approach to achieve optimal outcomes. Neoadjuvant chemotherapy, a fundamental of modern rectal cancer management, aims to shrink tumors, improve surgical resectability, and reduce the risk of recurrence. However, despite advancements in treatment protocols, a subset of patients fails to respond adequately to neoadjuvant chemotherapy, posing significant clinical challenges [1].
Understanding neoadjuvant chemotherapy in rectal cancer
Neoadjuvant chemotherapy, often administered in conjunction with radiotherapy, serves as a critical component of the multimodal treatment approach for locally advanced rectal cancer. By initiating systemic therapy prior to surgical resection, neoadjuvant chemotherapy aims to downsize tumors, eradicate micro metastases, and enhance the probability of achieving negative surgical margins. Additionally, neoadjuvant chemotherapy facilitates sphincter preservation in select cases, thereby improving quality of life outcomes for patients [2].
Despite its proven efficacy in improving oncological outcomes and facilitating sphincter-sparing surgeries, the response to neoadjuvant chemotherapy among patients with rectal cancer is heterogeneous. While many patients experience significant tumor regression and favourable responses, a subset demonstrates resistance to treatment, with tumors exhibiting limited or no response to chemotherapy. This phenomenon of non-response presents a formidable challenge in the clinical management of rectal cancer and highlights the need for a deeper understanding of its underlying mechanisms [3].
Exploring factors contributing to non-response
The non-response of rectal cancer to neoadjuvant chemotherapy is multifactorial in nature, with various biological, molecular, and clinical factors contributing to treatment resistance. Tumor heterogeneity, characterized by genetic and phenotypic diversity within the tumor microenvironment, plays a pivotal role in determining treatment response. Certain tumor subtypes may inherently possess resistance mechanisms that provide them less susceptible to chemotherapy-induced cytotoxicity [4].
Moreover, alterations in key signaling pathways, such as the PI3K/AKT/mTOR pathway and the Wnt/β-catenin pathway, can present resistance to chemotherapy agents commonly used in the treatment of rectal cancer [5]. Additionally, tumor microenvironment factors, including hypoxia, angiogenesis, and immune evasion mechanisms, may create a pleasant environment that interfere with the delivery and efficacy of chemotherapy drugs.
Clinical factors such as tumor stage, histological grade, and patient-related factors, including age, comorbidities, and performance status, also influence treatment response [6]. Patients with advanced-stage disease or aggressive tumor histology may exhibit diminished response to neoadjuvant chemotherapy compared to those with early-stage or less aggressive tumors.
Emerging strategies to overcome non-response
Addressing the challenge of non-response in rectal cancer requires a multifaceted approach that integrates advances in molecular profiling, targeted therapies, and personalized treatment strategies. Biomarker-driven treatment selection holds potential in identifying patients who are more likely to benefit from specific chemotherapy regimens [7]. Molecular profiling of tumors can identify actionable genetic alterations or biomarkers predictive of chemotherapy response, enabling the selection of altered treatment approaches [8].
Furthermore, the integration of novel targeted therapies, such as immune checkpoint inhibitors and molecularly targeted agents, into neoadjuvant treatment regimens provides the potential approach to enhance treatment efficacy and overcome resistance. Immunotherapy, in particular, has emerged as a potential therapeutic modality in rectal cancer, understanding the strength of the immune system to eradicate cancer cells and improve treatment outcomes [9].
In addition to targeted therapies, innovative treatment strategies, such as dose intensification, combination therapies, and treatment sequencing, warrant exploration to overcome non-response. Combinatorial approaches that target multiple signaling pathways simultaneously or exploit synthetic lethal interactions may provide the synergistic effects and overcome resistance mechanisms [10].
Conclusion
The non-response of rectal cancer to neoadjuvant chemotherapy poses a significant clinical challenge, highlights the complexity of this disease entity and the need for personalized treatment approaches. While substantial progress has been made in elucidating the underlying mechanisms of treatment resistance, further research is needed to identify novel biomarkers, therapeutic targets, and treatment strategies to overcome nonresponse and improve outcomes for patients with rectal cancer. By embracing a multidisciplinary approach and understanding the latest advances in oncology research, more effective and personalized treatment paradigms that maximize therapeutic benefit and minimize treatment-related morbidity for patients fighting against this formidable disease.
References
- Kim S, Huh JW, Lee WY, Yun SH, Kim HC, Cho YB, et al. Predicting survival in locally advanced rectal cancer with effective chemoradiotherapy response. Eur J Surg Oncol. 2024:108361.
[Crossref] [Google Scholar] [PubMed]
- Brière R, Martin AG, Letarte F, Fournier FR, Bouchard P, Drolet S. Surgical management of rectal cancer with synchronous treatment of prostate cancer. Langenbeck's Arch. Surg. 2024;409(1):1-8.
[Crossref] [Google Scholar] [PubMed]
- Sullo FG, Passardi A, Gallio C, Molinari C, Marisi G, Pozzi E, et al. Advancing personalized medicine in the treatment of locally advanced rectal cancer. J Clin Med. 2024;13(9):2562.
[Crossref] [Google Scholar] [PubMed]
- Chen Z, Zou Z, Qian M, Xu Q, Xue G, Yang J, et al. A retrospective cohort study of neoadjuvant chemoradiotherapy combined with immune checkpoint inhibitors in locally advanced rectal cancer. Transl Oncol. 2024;44:101955.
[Crossref] [Google Scholar] [PubMed]
- Chiloiro G, Cintoni M, Palombaro M, Romano A, Reina S, Pulcini G, et al. Impact of body composition parameters on radiation therapy compliance in locally advanced rectal cancer: A retrospective observational analysis. Clin Transl Radiat Oncol. 2024:100789.
[Crossref] [Google Scholar] [PubMed]
- Liu M, Cui N, Sun C, Gong X, Wang B, Yang D, et al. A prospective study on using shear wave elastography to predict the ypT0 stage of rectal cancer after neoadjuvant therapy: A new support for the watch-and-wait approach? Front mol biosci. 2024 Apr 26;11:1402498.
[Crossref] [Google Scholar] [PubMed]
- Guo X, He Y, Yuan Z, Nie T, Liu Y, Xu H. Association analysis between intratumoral and peritumoral MRI radiomics features and overall survival of neoadjuvant therapy in rectal Cancer. J Magn Reson Imaging. 2024.
[Crossref] [Google Scholar] [PubMed]
- Yu G, Chi H, Zhao G, Wang Y. Tumor regression and safe distance of distal margin after neoadjuvant therapy for rectal cancer. Front. oncol. 2024;14:1375334.
[Crossref] [Google Scholar] [PubMed]
- Williams H, Thompson HM, Lee C, Rangnekar A, Gomez JT, Widmar M, et al. Assessing endoscopic response in locally advanced rectal cancer treated with total neoadjuvant therapy: Development and validation of a highly accurate convolutional neural network. Ann. Surg. Oncol. 2024:1-9.
[Crossref] [Google Scholar] [PubMed]
- Bratu LD, Schenker M, Stovicek PO, Schenker RA, Mehedințeanu AM, Berisha TC, et al. Retrospective evaluation of the efficacy of total neoadjuvant therapy and chemoradiotherapy neoadjuvant treatment in relation to surgery in patients with rectal cancer. Medicina. 2024;60(4):656.
[Crossref] [Google Scholar] [PubMed]
Citation: Scotti V (2024) Treatment Resistance: Understanding the Neoadjuvant Chemotherapy in Rectal Cancer. J Carcinog Mutagen. S43:005.
Copyright: © 2024 Scotti V. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.