Indexed In
- Open J Gate
- Academic Keys
- JournalTOCs
- ResearchBible
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2024) Volume 12, Issue 3
The Use of an Information-Theory based Diagnostic Rule for Hip Fracture Evaluation and Prediction
David Blokh1,2, Ilia Stambler1*, Joseph Gitarts3 and Eliyahu H. Mizrahi12Department of Medicine, C.D. Technologies Ltd., Beer Sheba, Israel
3Department of Medicine, Efi Arazi School of Computer Science, Herzliya, Israel
Received: 20-Apr-2020, Manuscript No. JASC-24-3933 ; Editor assigned: 23-Apr-2020, Pre QC No. JASC-24-3933 (PQ) ; Reviewed: 07-May-2020, QC No. JASC-24-3933 ; Revised: 15-Jul-2024, Manuscript No. JASC-24-3933 (R); Published: 12-Aug-2024, DOI: 10.35248/2329-8847.24.12.377
Abstract
Objective: The present work explores the application of a new methodology, based on an information theoretical measure, the normalized mutual information, for hip fracture risk evaluation and prediction.
Methods: A dataset on geriatric hip fracture patients was analyzed, including diagnostic parameters routinely available to physicians, such as physiological, biochemical, immunological and hematological parameters. Information-theory based methods were utilized to establish correlations between the parameters and to construct a diagnostic decision rule for hip fracture risk evaluation at different age groups.
Results: The use of information-theoretical methods, utilizing normalized mutual information, revealed the exact amount of information that various diagnostic parameters contained about the presence of hip fracture at different ages. Based on those exact informative values for hip fracture evaluation, we constructed a diagnostic rule (a decision tree) to estimate a person’s risk for hip fracture at different ages. We established a risk group for hip fracture at a relatively “younger” age (below 80 years old). We developed an algorithm (decision tree) that can be used to evaluate whether a subject can be categorized as belonging to the risk group for hip fracture under 80 years old. The algorithm’s sensitivity was 58.8% and its specificity was 54.6%.
Conclusion: With the addition of further data and validation, algorithms constructed by this methodology can be used to help predict the risks of hip fracture in elderly subjects, in order to optimize preventive interventions.
Keywords
Information theory; Hip fracture; Diagnostic rule; Normalized mutual information; Prediction
Introduction
Hip fractures (breakage of femur bone close to the hip joint) are a highly frequent and severe problem of the geriatric population. The incidence of hip fractures in the US was estimated at about 1000 per 100,000 in women and up to 500 per 100,000 in men. With aging, the incidence increases dramatically. In patients over 80 it can reach up to 2000 in men and 3000 in women per 100,000. The mortality from this condition is also very high. About 30% of people with a hip fracture will die in the following year. The majority of the subjects will experience severe functional disability. The costs of treatment of this condition are also very high. Thus, in the US, a typical patient with a hip fracture will expend US $40000 in the first year after hip fracture for direct medical costs and almost $5000 in the years after that. Notably, hip fracture is not a stand-alone condition, but manifests and can result from a variety of other age-related comorbidities and adverse conditions, such as osteoporosis, sarcopenia, reduced vision or mobility, balance problems, additional age-related diseases (cancer, neurodegenerative diseases) and more. Thus, clearly, the ability to mitigate this condition by early detection and prediction to enable early preventive intervention can have enormous medical and economic significance. The present study develops a new diagnostic decision rule methodology to facilitate such early detection and prediction of hip fractures, utilizing informationtheoretical measures [1].
The present work explores the application of an informationtheoretical measure, the normalized mutual information, for hip fracture evaluation and prediction. The use of informationtheoretical measures provides important methodological advantages over the use of regular (linear) statistics for the study of age-related diseases and disabilities. Among other advantages, such measures make it possible to estimate non-linear correlations between biological parameters and indicate the exact quantitative strength of those correlations, both for individual and multiple parameters. Moreover, they can show cumulative, synergistic or holistic effects of multiple parameters. Here we illustrate those capabilities utilizing a dataset on geriatric hip fracture patients, including diagnostic parameters routinely available to physicians, such as physiological, biochemical, immunological and hematological parameters [2].
The information-theoretical measure of normalized mutual information determined the precise amount of information (informative value) that different diagnostic parameters contained about the presence of hip fracture within specified age ranges. Based on those exact informative values for hip fracture evaluation, we constructed a diagnostic rule (a decision tree algorithm) to evaluate a person’s risk for hip fracture at a particular age range. Specifically, we established the definitions for a risk group for patients that could develop hip fracture at a relatively “younger” age (less than 80 years old). The algorithm (decision tree), that we developed, can be used to evaluate whether a subject can be categorized as belonging to the risk group for hip fracture within this particular age range. Such algorithms, based on the proposed methodology, can be utilized to define risk groups for hip fracture at any other age range, or according to other defining characteristics [3].
Materials and Methods
Mathematical analysis
In the present work, the chosen information-theoretical measure of correlation of diagnostic parameters with the age of hip fracture occurrence is the Normalized Mutual Information (NMI), which is also termed "uncertainty coefficient". In contrast to the evaluation of parameters’ correlations using the linear correlation coefficient, the normalized mutual information enables the investigators to determine non-linear correlations of the diagnostic evaluation parameters of interest with the presence of disease. Moreover, normalized mutual information value provides the exact amount of information (or informative value) that each diagnostic parameter contains about the presence of hip fracture at a particular age.
We calculate the normalized mutual information according to the standard procedure. Thus, we assume X to be a discrete random value having the following distribution function [4].
| X | x1 | x2 | ....... | xn |
| Q | p1 | p2 | ....... | pn |
Here X can be any diagnostic evaluation parameter of interest, n is the number of categories of the evaluation parameter, pi designates the frequency of the category xi. The Entropy of a random value X is determined by the formula:
We assume X and Y to be discrete random values (evaluation parameters). The algorithms for the calculation of normalized mutual information between parameters or parameter combinations have been described earlier. Here, we build on these methods, to create a new information-theory based methodology for risk group attribution for hip fractures [5].
In short, for the parameters X and Y, the value of normalized mutual information c is calculated by the standard formula:
where H(X), H(Y), H(X,Y) are, respectively, the entropies of random values X, Y and X × Y. The values of normalized mutual information approaching zero signify a weaker correlation value, whereas the normalized mutual information approaching unity shows a stronger correlation between evaluation parameters.
It is important to emphasize that normalized mutual information measures the precise amount of information that each evaluation parameter contains about the presence of hip fracture. Based on such exact quantities of information or informative weights/values of all the parameters, it is possible to create a diagnostic rule for the evaluation of the person’s risk to develop hip fracture at a particular age, categorizing the subjects into risk groups according to the strength of correlation. In the present work we use a decision tree as a determinant diagnostic rule. The application and algorithm for the construction of decision trees have been presented earlier. Here we build on these methodologies to create a new method for risk group attribution for hip fractures [6].
The decision tree can be useful in clinical evaluation practice, mainly for two reasons: A decision tree diagnostic model closely follows the description of clinical decision making and it can be easily theoretically justified and interpreted. In the present work, we built the decision rule about the risk of hip fracture above or below 80 years of age using a small set of diagnostic parameters routinely available to treating physicians. This way, we were able to demonstrate the potential common applicability of information-theoretical methodology to assess the risk of hip fracture.
Case materials
This research comprised 206 hip fracture patients, hospitalized at the Shmuel Harofe geriatric medical center, in Beer Yaakov, Israel. The patients' data were accessed retrospectively, according to the principles of the declaration of Helsinki. The study was approved by the institutional review board of Shmuel Harofe geriatric medical center (IRB Approval No. 53). The patient data used in this research were anonymized prior to the study [7].
The patients, aged 63 to 97, included 130 females and 76 males. 66 patients were younger than 80 years old and 140 were 80 years old and older. For the illustration of the proposed methodology, we selected a group of diagnostic evaluation parameters commonly available to treating physicians, mainly obtained from routine blood tests. The parameters represented different types of blood biomarkers, including: Cellular and/or immunological parameters (numbers of white blood cells, lymphocytes and neutrophils), microelement levels (Calcium-Ca, Potassium-K, Sodium-Na), hematological parameters (hemoglobin, number of platelets), common metabolites (glucose, total cholesterol, urea, albumin, total protein, triglycerides, folic acid), enzymes (creatinine, Alkaline Phosphatase-ALP), physiological indicators (heart rate, systolic blood pressure, diastolic blood pressure) and a few selected medical conditions (ischemic heart disease, hyperliplidemia). For the construction of the diagnostic model, we used the data gathered at the patient's admission to the hospital, rather than at the discharge, in order to exclude the effects of intervention (surgery). Gender was also included as an indispensable distinguishing parameter. Thus, altogether 23 diagnostic parameters were evaluated. The risk of hip fractures at a particular age range (below 80 y.o. vs., at 80+ y.o.) was considered as the diagnosed/predicted outcome [8].
For the application of the information-theoretical model, all the data must be discretized. The discretization thresholds (boundaries) were determined according to the algorithm for physiological boundaries evaluation by maximizing normalized mutual information for all the patients. The discretization boundaries are shown in Table 1. In the decision tree, values equal to or above the boundary were designated as 1 for the algorithm construction or coded as red line in the decision tree shown in Figure 1. Values below the boundary were designated as 0 or blue line in the decision tree (Figure 1). Male subjects were designated as 0 or blue and females as 1 or red. The presence of particular medical conditions (e.g. hyperlipidemia, ischemic heart disease) was coded as 1 or red, the absence of those conditions as 0 or blue. Proceeding along the lines of the decision tree, we establish the presence of the diagnosed/ predicted value, namely the occurrence of hip fracture below age 80 (R, Risk of an earlier hip fracture) vs., 80+ (N, no risk).
| Parameter | Boundary | NMI | |
|---|---|---|---|
| 1 | Albumin | 3.31 g/dL | 0.09587 |
| 2 | Urea | 42 mg/dL | 0.06333 |
| 3 | Hemoglobin | 10.4 g/dL | 0.04806 |
| 4 | Ca | 9 mg/dL | 0.02723 |
| 5 | Gender | 1/0 | 0.01983 |
| 6 | White blood cells | 8500 1/μL | 0.01832 |
| 7 | Triglycerides | 128 mg/dL | 0.01719 |
| 8 | Total protein | 5.98 g/dL | 0.01252 |
| 9 | Diastolic blood pressure | 66.5 mmHg | 0.01252 |
| 10 | Neutrophils | 5500 1/μL | 0.01207 |
| 11 | Platelets | 320000 1/μL | 0.00893 |
| 12 | Na | 139 nmol/L | 0.00827 |
| 13 | Lymphocytes | 1700 1/μL | 0.0061 |
| 14 | Creatinine | 0.8 mg/dL | 0.00283 |
| 15 | Alkaline phosphatase | 90 U/L | 0.00255 |
| 16 | Total cholesterol | 160 mg/dL | 0.00137 |
| 17 | Ischemic heart disease | 1/0 | 0.00119 |
| 18 | Systolic blood pressure | 127 mmHg | 0.0008 |
| 19 | K | 4.3 nmol/L | 0.0008 |
| 20 | Heart rate | 77 BPM | 0.0008 |
| 21 | Blood glucose | 120 mg/dL | 0.00071 |
| 22 | Hyperlipidemia | 1/0 | 0.00071 |
| 23 | Folic acid | 8.5 ng/ml | 0.00054 |
Table 1: Values of Normalized Mutual Information (NMI) between particular diagnostic parameters and the presence of hip fracture under age 80 (the diagnosed parameter) vs., 80+.
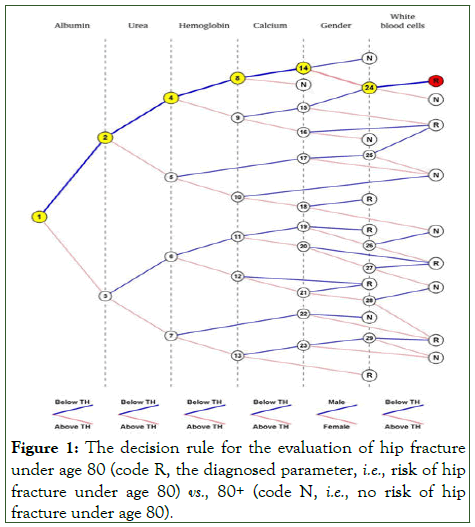
Figure 1: The decision rule for the evaluation of hip fracture under age 80 (code R, the diagnosed parameter, i.e., risk of hip fracture under age 80) vs., 80+ (code N, i.e., no risk of hip fracture under age 80).
Results and Discussion
We established the values of Normalized Mutual Information (NMI) for all the 23 diagnostic parameters vs., the age at hip fracture (below 80 y.o. vs., 80+ y.o.). Table 1 shows the values of Normalized Mutual Information (NMI or the amount of information about the presence of hip fracture) for all the parameters in descending order. For the construction of the decision rule, the following diagnostic parameters were selected: Albumin, urea, hemoglobin (Hb), calcium (Ca), gender, White Blood Cells (WBC).
These parameters were chosen insofar as these are the most informative parameters, as shown by their highest values of normalized mutual information between the parameters and the presence of hip fracture under 80 y.o.
Figure 1 shows the decision tree based on the selected diagnostic parameters. Notice the decision making proceeds from the most informative (discriminative) parameter to the less informative parameter. Namely, the decision making proceeds from the most informative indicator albumin (NMI=0.09587) to urea (NMI=0.06333) to hemoglobin (NMI=0.04806) to calcium (NMI=0.02723) to gender (NMI=0.01983) to the least informative in this group white blood cells (NMI=0.01832). This may roughly reflect the clinical decision making process, first discerning the most salient diagnostic features and then finetuning the decision by the more nuanced parameters. Any number of available diagnostic parameters could be included into the diagnostic rule (decision tree), but for practical purposes, the most discriminating features may be sufficient [9].
The findings of the most informative parameters are not surprising. Alterations in all these parameters were associated with frailty and aging states in earlier research. Specifically, the present work found the most informative parameter to be Albumin, the most abundant blood transport protein. In the past, albumin decrease has been associated with frailty and degenerative aging states in a variety of studies and with poor hip fracture outcomes in particular. Also the high informative value of urea could indicate the high importance of protein metabolism and protein homeostasis in aging. Furthermore, hemoglobin could give a special indication for the organisms’ oxygen supply state, calcium for the state of the muscular and skeletal systems and WBC for the immunological state. The interrelation of the various parameters of those systems created the decision rule. Also gender has been well recognized discriminating parameter for frailty status, other aging-related conditions and life expectancy. Altogether, these parameters provided a substantial basis to create the decision rule.
Consider an example of the use of the decision rule (Figure 1). Consider a woman aged 68 (red-coded), with the following blood test parameters: Albumin=2.91, urea=38.6, Hemoglobin (Hb)=9.7, Calcium (Ca)=8.09, White Blood Cells (WBC)=8100. Comparing these values with the values of boundaries for each parameter and coding accordingly as blue line below the boundary and red line equal and above the boundary, we obtain the following parameter value codes: Albumin (blue), urea (blue), hemoglobin (Hb) (blue), calcium (Ca) (blue), gender (red), White Blood Cells (WBC) (blue). With these parameter value codes we proceed along the nodes: 1-2-4-8-14-24 eventually arriving in the final node R (indicating hip fracture risk below the age of 80, the diagnosed parameter). Such an example is typical. In women the hip fractures are more frequent than in men and the relatively lower values of the majority of these parameters (below the threshold), especially for albumin, hemoglobin and calcium, have been associated with frail states. Yet it should be noted that also when the values for particular parameters are above the threshold (e.g. for albumin) it is possible to be categorized as having a risk of hip fracture in a younger age. This may illustrate the need to consider several diagnostic parameters at the same time, as any parameter considered only individually may be misleading [10].
The decision rule produced satisfactory diagnostic results. Within the entire cohort of 206 patients that were analyzed, 66 were younger than 80 years old and 140 were 80 years old and older. The decision rule (decision tree) was constructed based on 32 patients younger than 80 and 32 patients 80 years old and older. The accuracy of the decision tree was tested. Testing was done on 142 patients, including 34 patients younger than 80 years old and 108 patients 80 years old and older. Of the 142 tested patients, the age of 79 patients was determined correctly. The age of 20 patients younger than 80 years old was determined correctly and the age of 59 patients 80 years old and older was determined correctly.
• Thus, the accuracy of the prediction was (79/142)*100% 55.6%.
• The sensitivity was (20/34)*100% 58.8%.
• The specificity was (59/108)*100% 54.6%.
For the present purposes, the most important parameter is the sensitivity of the prediction, that is to say, the ability to correctly identify subjects below 80 years of age who are at risk of a hip fracture. The algorithm’s sensitivity was 58.8%. That is to say, when validating the algorithm, within the group of patients that the algorithm suggested had an increased risk of hip fracture under 80 y.o., almost 60% indeed had a hip fracture. Insofar as the sensitivity (the ability to correctly identify the risk group) is the most important outcome for this diagnostic problem, the obtained result can be considered as satisfactory, yet suggesting the need for further refinement of the diagnostic decision rule, with the use of more data. Notably, the diagnostic model in the form of a decision tree provides a visually convenient form to evaluate multiple diagnostic parameters. Such a form could be used by any physician, even without access to a computer and even by a patient himself.
This usability by the physicians, utilizing easily obtainable diagnostic parameters, is a major advantage of the proposed method. In our earlier works, we performed the comparative analysis of the information-theoretical method with the most popular statistical methods: ANOVA (parameter analysis) and logistic regression (diagnosis) methods. Both for the parameter analysis and diagnosis, the information-theoretical method proved to be preferable over the statistical methods. Here we compare the present method with the commonly used methods for fracture risk evaluation: QFracture, FRAX and Garvan fracture risk calculators. QFracture uses 26 parameters, including type 1 or type 2 diabetes, parental history of hip fracture/ osteoporosis, dementia, cancer, parkinson's disease, rheumatoid arthritis. FRAX uses 11 parameters, including parent fractured hip, rheumatoid arthritis, secondary osteoporosis, femoral neck Bone Mineral Density (BMD g/cm2). The Garvan fracture risk calculator uses 5 parameters, including actual BMD. The sensitivity and specificity of these methods are, respectively: For QFracture-61.4% and 90.9%, FRAX-43.6% and 90.9% and Garvan-28.7% and 90.8%. In terms of sensitivity and specificity, our method is significantly inferior to QFracture, but quite comparable with FRAX and Garvan. However, the QFracture calculator uses such parameters as type 1 or type 2 diabetes, dementia, cancer, parkinson's disease, rheumatoid arthritis, which may not yet be present at the age of 40-50 or may not yet be manifest. Also the “parental history of fracture/osteoporosis” may be obscure. Similar difficulties may arise for FRAX that uses the parameters parent fractured hip, rheumatoid arthritis, secondary osteoporosis. In addition, FRAX and Garvan, using the parameter bone mineral density (BMD g/cm2), require special dosimetry measurements. For QFracture, the literature also notes the problem of “inappropriate source data,” acknowledging the need to develop new methods for hip fracture risk assessment. In contrast, our method uses parameters of routine blood work. Unlike the FRAX and Garvan methods, the sensitivity and specificity of our method are balanced (58.8% and 54.6% respectively). Furthermore, the present method allows performing the practical risk evaluation after any routine blood test [11].
The practical application of this model for the identification of risk groups and prevention of hip fractures has already been piloted at the Shmuel Harofe geriatric medical center. Thus, using the decision rule, we examined 28 subjects younger than 80 years old for potential risk of hip fractures. Of the 28 examined subjects younger than 80 y.o., 19 were indicated with a fracture risk below 80 y.o. (within their age group) and 9 with a fracture risk above 80 y.o. The former group of younger subjects is the target risk group of interest, insofar as the main purpose of the present model is to indicate the risks for the younger subjects and suggest preventive recommendations. The examined subjects were patients that were hospitalized at the Shmuel Harofe geriatric medical center due to functional decline following brain damage or prolonged hospitalization in a general hospital, yet without hip fractures. As a part of the treatment, these patients are instructed for reconditioning and healthy life style. At the admission, such patients undergo physical examination by a multidisciplinary care team and undergo physiotherapy and occupational therapy at the rehabilitation department, while especially emphasizing exercise to increase muscle strength, body balance and walking in order to reduce the risk of falls and consequent hip fractures [12].
Conclusion
The proposed methodology can help the development of predictive diagnosis and preventive treatment or “precision medicine” for the emergence of hip fracture in specific groups of geriatric patients. Utilizing such information-theory-based algorithms, using the proposed methodology, with additional data, it may be possible to create further clinically applicable information-theory-based models and potentially computer programs, for the evaluation of risk of hip fracture, in different age groups, based on routinely measured diagnostic parameters. The finding of an enhanced risk of a hip fracture at a younger age may pinpoint a stronger need for preventive measures, including pharmacological means, nutritional supplementation, exercise, preconditioning, assistive technologies and other lifestyle modifications. Such algorithms, with the additional data on interventions, can be used not only for early diagnosis and prediction, but also for the evaluation of success of potential therapeutic interventions and for recommending specific early preventive interventions, for the groups at risk.
Conflicts of Interest
The authors have no conflict of interest.
Acknowledgments
This work was supported by the Shlomo Tyran foundation.
References
- Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB. Incidence and mortality of hip fractures in the United States. Jama. 2009;302(14):1573-1579.
[Crossref] [Google Scholar] [PubMed]
- Blokh D, Stambler I. The application of information theory for the research of aging and aging-related diseases. Prog Neurobiol. 2017;157:158-173.
[Crossref] [Google Scholar] [PubMed]
- Blokh D, Stambler I. Information theoretical analysis of aging as a risk factor for heart disease. Aging Dis. 2015;6(3):196.
[Crossref] [Google Scholar] [PubMed]
- Blokh D, Stambler I. The use of information theory for the evaluation of biomarkers of aging and physiological age. Mech Ageing Dev. 2017;163:23-29.
[Crossref] [Google Scholar] [PubMed]
- Zhang LX. A functional central limit theorem for asymptotically negatively dependent random fields. Acta Math Hung. 2000;86(3):237-259.
- Zvarova J, Studeny M. Information theoretical approach to constitution and reduction of medical data. Int J Med Inform. 1997;45(1-2):65-74.
[Crossref] [Google Scholar] [PubMed]
- Blokh D, Stambler I, Afrimzon E, Shafran Y, Korech E, Sandbank J, et al. The information-theory analysis of Michaelis-Menten constants for detection of breast cancer. Cancer Detect Prev. 2007;31(6):489-498.
[Crossref] [Google Scholar] [PubMed]
- Podgorelec V, Kokol P, Stiglic B, Rozman I. Decision trees: An overview and their use in medicine. J Med Syst. 2002;26:445-463.
[Crossref] [Google Scholar] [PubMed]
- Lin CH, Liao CC, Huang CH, Tung YT, Chang HC, Hsu MC, et al. Proteomics analysis to identify and characterize the biomarkers and physical activities of non-frail and frail older adults. Int J Med Sci. 2017;14(3):231.
[Crossref] [Google Scholar] [PubMed]
- Bylow K, Hemmerich J, Mohile SG, Stadler WM, Sajid S, Dale W. Obese frailty, physical performance deficits and falls in older men with biochemical recurrence of prostate cancer on androgen deprivation therapy: A case-control study. Urology. 2011;77(4):934-940.
- Pioli G, Barone A, Giusti A, Oliveri M, Pizzonia M, Razzano M, et al. Predictors of mortality after hip fracture: Results from 1-year follow-up. Aging Clin Exp Res. 2006;18:381-387.
[Crossref] [Google Scholar] [PubMed]
- Putin E, Mamoshina P, Aliper A, Korzinkin M, Moskalev A, Kolosov A, et al. Deep biomarkers of human aging: Application of deep neural networks to biomarker development. Aging. 2016;8(5):1021.
[Crossref] [Google Scholar] [PubMed]
Citation: Blokh D, Stambler I, Gitarts J, Mizrahi EH (2024) The Use of an Information-Theory based Diagnostic Rule for Hip Fracture Evaluation and Prediction. J Aging Sci. 12:377.
Copyright: © 2024 Blokh D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

