Indexed In
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
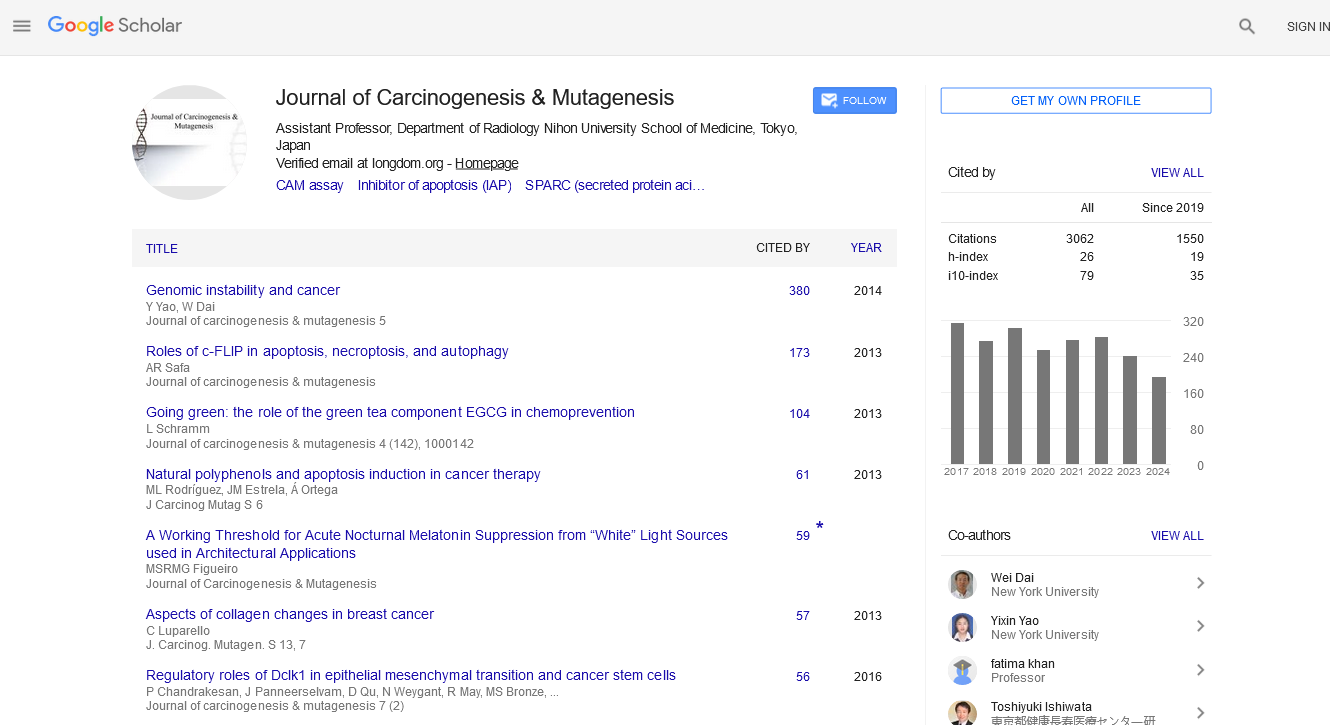
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Review Article - (2020) Volume 11, Issue 4
The Toxicity of Carcinogenic Metals to the Brain
Max Costa* and Angelica OrtizReceived: 17-Jul-2020 Published: 14-Aug-2020, DOI: 10.35248/2157-2518.20.11.354
Abstract
Metal toxicity is often associated with inflammatory diseases and carcinogenesis. Various metal compounds have the capacity to induce DNA damage and elicit epigenetic changes that contribute to cell transformation and cancer. Understanding the altered pathways elicited by these metals and metal compounds aid in the preventative care as well as establishment of therapy regimens. As the ambient environment becomes contaminated with these toxic metals, studies have also demonstrated a growing capacity of metals designated as carcinogens to also exhibit neurotoxicity. The brain is often thought as a protected organ within the confines of the skull and protected from foreign substances by the blood brain barrier. Unfortunately, carcinogenic metals exist as compounds conferring their ability to enter the brain and accumulate, and in many instances they do so by destroying the blood brain barrier. The presence and accumulation of these pernicious compounds activates pathways that alter neurochemistry that support cognitive and motor function.
Keywords
Cancer; Carcinogenic; Metals; Carcinogens
Introduction
Chromate, nickel, cadmium and arsenic compounds are well established human carcinogens [1]. Studies have shown that all of these carcinogens can induce lung cancer in humans. Arsenic, cadmium and chromate appear to have induced a broader spectrum of cancers compared to nickel compounds. However, this may be due to the more numerous studies with those compounds compared to studies focusing on nickel compounds. Chromium is a pervasive environmental contaminant that is of great importance because of its toxicity. There is metallic Cr, Cr(III) and Cr+6. Cr(III) is about 1000 times less toxic than Cr(VI) and Cr(III) is the major form found naturally, but Cr+6 in our environment is usually a result of human activity [2]. There have been many cases of humans being poisoned by environmental Cr+6 in drinking water and also occupationally in chrome platers, tanning of leather and its use as an antirust agent and wood preservative [2]. Hexavalent chromium is classified as a group 1 carcinogen with multiple complex mechanisms by which it triggers cancer development [2]. Increased levels of oxidative stress, chromosome breaks, and DNA-adduct formation are some of the major mechanisms by which Cr(VI) causes cellular damage [3]. Chromate resembles sulfate and phosphate and for that reason is transported into cells and distributes to all tissues in the body including the brain [2,4]. Once inside the cell it is converted rapidly to Cr(III) and oxidative stress results from this conversion as well as Cr(III) reaction with DNA and protein are responsible for it intracellular toxicity. Assessing human exposure to Cr+6 requires measuring the Cr concentration inside a blood cell such as red blood cells or white blood cells [5]. The reason for this is because Cr(III) will not enter cells but Cr+6 is actively transported into cells and any Cr inside the cell is assumed to have been Cr+6. Cr +6 is the only toxic agent that becomes safer after it is taken up by plants or animals since these can be consumed by humans. This is because all the Cr+6 has been converted to the non-toxic Cr(III) [2]. Chromate is known to cause lung, GI cancers such as small intestinal and liver cancers, pancreatic and stomach cancers [2,6,7]. Chromate is the only metal carcinogen that forms adducts with DNA and exhibits significant mutagenic activity directly [2].
Arsenic causes lung, bladder, liver, skin, and colon cancers [8,9]. Oxidative stress is the major mechanism for arsenic induced cancers, although inhibition of DNA repair via disruption of 3S and 4S Zn fingers, epigenetic effects including polyadenylation of canonical histones are also important mechanisms of As carcinogenesis [8,10-12]. The polyadenylation of canonical histone H3.1 results in more H3.1 protein which differs from H3.3 (a non-canonical histone) by 5 amino acids. H3.3 is found in active promoters enabling gene expression and is displaced when H3.1 is polyadenylated because arsenic causes stem loop binding protein to be degraded and canonical histones cannot be processed without a poly A tail. The polyadenylation increases the stability of the mRNA and causes more H3.1 protein to be produced, which in turn knocks out H3.3 from promoters and other sites in chromatin [8,12]. Arsenic is the only metal that is metabolized by methylation in the liver and other tissues [8]. The methylation of As increases the inherent toxicity of the arsenic (As) compound thus monomethyl and dimethyl arsenite are more toxic than inorganic arsenite [8]. The methylation of arsenite also increases its lipid solubility and will enhance its delivery to the brain but it also increases the excretion of arsenic from the body and thus humans who become resistant to arsenate and arsenite have greater liver methylation capacity [8].
Cadmium is well established as a lung carcinogen in humans. However there are other human cancers associated with cadmium (Cd) exposure including prostate, kidney, Breast, (Cd is estrogenic) urinary bladder [13]. Kidney, breast and pancreas human cancer data are stronger than that of prostate and bladder [13]. Over all, cadmium exposures of laboratory animals causes tumors of the hematopoietic system (leukemia and lymphoma), local sarcoma, and cancers of the adrenal gland, liver, lung, kidney, pancreas, pituitary, prostate, and testis [13]. Mechanism of Cd carcinogenesis also involve oxidative stress and it also has a very long half-life in vivo because it is tightly bound to metallothionein [13]. Cd also interferes with Zn fingers and in particular is very active at displacing Zn, since they both chemically very similar.
Water insoluble nickel sulfides and oxides are highly carcinogenic to humans causing nasal and lung cancers [14]. These water insoluble Ni compounds have induced lung cancers in the NTP study but water soluble Ni compounds were not carcinogenic [15,16]. These carcinogenic nickel compounds such as crystalline nickel subsulfide and sulfide are taken up into cells by phagocytosis while non-carcinogenic water insoluble compounds are not taken up into cells [17,18]. This is caused by the surface charge of the particles; those having negative surface charge are phagocytized while those with a positive charge are not [19-21]. In fact, if the surface charge of the particles is changed from positive to negative based on zeta potential, then the particle is taken up by phagocytosis and becomes carcinogenic [22]. The entry of a large nickel containing particle into the cell results in dissolution of Ni ions in lysosomes and vacuoles and intracellular Ni reaches very high levels. Although Ni ions can enter cells by the Fe/Mn transporter DMT1, this pathway does not cause large accumulation of intracellular Ni because soluble Ni compounds are rapidly cleared from tissues. The intracellular mechanisms of Ni ion carcinogenesis involves the inhibition of the Fe containing dioxygenase enzymes [23,24]. These enzymes all have Fe in their active site that is coordinated to 2 histidinesand a carboxylic facial triad. The Fe is pentacoordinated allowing one site for binding of molecular oxygen which is split in the reaction to yield hydroxylation of proline or arginine or demethylation of nitrogen. Ni is able to inhibit the oxygens sensor prolyl hydroxylase whose hydroxylation of HIF1 alpha at a proline residue in the oxygen dependent domain targets it for degradation. Thus, exposure to Ni or Co will displace the Fe in the active site of the prolyl hydroxylase causing accumulation of HIF-1 and a change in the genes expressed to create a hypoxic state under normal oxygen tension. Other enzymes that are dioxygenases are also inhibited by Ni and these include the Tet protein, histone demethylases, and FTO a DNA demethylase [16,25]. In addition to these effects of Ni, this metal can also induce silencing of genes that are located near heterochromatin [26]. The mechanism involves the ability of Ni to condense heterochromatin better than Mg ions resulting in the spreading of condensation and silencing of genes near heterochromatin [26].
Exposure to these carcinogens also induce neurotoxicity, likely through similar mechanisms. Neurotoxicity refers to damage to nervous tissue in the peripheral nervous system and/or central nervous system. Dysfunction of the peripheral nervous system can diminish motor function and autonomic neuropathy. Damage to the central nervous system (brain and spinal cord) alters cognitive function as well as sensation and movement. While various metals, including these carcinogenic metals, can be excreted from peripheral systems, the nervous system is more vulnerable to metal toxicity as it readily accumulates metals. The nervous system is vulnerable to foreign substances (i.e. xenobiotics) due to the complexity of the central nervous system due to the high metabolic rates of the neurons, myelination, and physical barriers, such as the blood-brain barrier and the choroid plexus. As such, carcinogenic metals may contribute to neurodegeneration by altering the blood-brain barrier or traversing it. The choroid plexus, which generates cerebrospinal fluid and acts as a filter to remove xenobiotics and waste, relies on calcium homeostasis that can be disrupted by foreign, nonessential metals. This review article will explore the carcinogenic metal compounds in neurotoxicity within the brain.
Chromium Toxicity To The Brain
Although there are many studies that examined the effect of chromate on the brain in developing embryos, this review focuses on the effect of chromate on adult animals or humans. Chromium oxide nanoparticles (Cr2O3 NPs) have a wide range of applications in industry. They are used as pigments, catalysts, wear-resistant or high-temperature-resistant coating material and are used in liquid crystal displays. Chromium compounds can enter the body via ingestion or pass through the intranasal cavity, which is rich in highly vascularized and possesses a highly permeable membrane [27]. When absorbed through the intranasal cavity allows for quick entry into the brain, olfactory nerves, and trigeminal nerves [28]. A study was conducted to evaluate biochemical changes and histopathological alterations in the kidneys and brain of rats, following exposure to Cr2O3 NPs. Male Wistar rats were divided into low-dose (50 microg/100 g body weight) and high-dose (200 microg/100 g bwt) groups. Each group type received oral Cr2O3 NPs for single dosing, once daily for 7 days and once daily for 14 days, respectively. In the kidneys and brain of Cr2O3 NPs-exposed animals, reactive oxygen species production caused a significant increase in malondialdehyde concentration along with a significant decrease in superoxide dismutase and glutathione levels, as compared to controls [29].
The toxic effects of Cr (VI) to zebrafish at environmental concentrations (2mg/L) was studied. The genotoxic potential of Cr (VI) in erythrocytes revealed an increase in frequency of micronucleated erythrocytes along with blebbed, lobed and notched nuclei [30]. Histological alterations in brain, elevated GSH and MDA content and increased catalase activity indicated oxidative stress-mediated brain damage. This was further confirmed through expressional alteration of Ucp2 and upregulation of Nrf2, Nqo1 and Ho1 indicating the involvement of Nrf2-ARE system in a oxidative stress response to Cr(VI) induced neurotoxicity [30]. The transcriptional induction of apoptotic genes such as Bax, Caspase 9 and Caspase 3 along with downregulation of Bcl2 indicated that the cytoprotective system failed to mitigate the induced stress. There was also upregulation of AChE gene which correlated with the upregulated apoptotic genes. The induction of nuclear anomalies in the erythrocytes can serve as extremely sensitive endpoints of toxicological stress indicators of aquatic contaminants like Cr(VI) [30].
There are many studies that show sublethal doses of chromate salts injected intraperitoneally in rats and rabbits results in the presence of a substantial amount of chromium to the brain [31]. A study investigated the contents of trace elements and entry of chromate into the brain and serum of male chickens and whether Se can suppress the entry and toxicity of chromate in the brain. 22.14 mg/kg K2Cr2O7 with 0.00, 0.31, 0.63, 1.25, 2.50, and 5.00 mg/kg Na2SeO3 mg/kg B.W was used in the drinking water daily. After 14, 28, and 42 days of exposure, the brain and serum of chickens from each group were collected and levels of metals were measured by ICP-MS. The contents of Cr increased both in the brain and serum in a time dependent manner. Cr contents in the brain and serum decreased with Se co-exposure [32]. In another study, the effect of selenium against oxidative stress induced by chromium in the cerebrum and cerebellum was studied in female Wistar rats. Animals were randomly divided into four groups with 6 rats per group. Group 1 served as control, group II received drinking water with K2Cr2O7 alone (700 ppm); group III received both K2Cr2O7and Se (0.5 mg Na2SeO3/kg of diet); and group IV received Se (0.5 mg/kg of diet) for 3 weeks [33]. The exposure of rats to K2Cr2O7 promoted oxidative stress in the cerebrum and cerebellum with an increase in malondialdehyde and a decrease of antioxidants such as glutathione, nonproteinthiol, and vitamin C [33]. An increase of catalase, glutathione peroxidase, and superoxide dismutase activities was also observed. Acetylcholinesterase activity was inhibited after treatment with K2Cr2O7. Co-administration of Se restored all the parameters mentioned above and histopathological findings were used to confirmed the biochemical results [33].
Potassium dichromate was given to female Swiss mice (25 mg/kg per day) orally in water for 1-3 days. Brain homogenates were used to evaluate antioxidant levels and the extent of lipid peroxidation. In addition, mitochondrial fractions were isolated from brain homogenates to determine the production of reactive oxygen species. The administration of potassium dichromate for 3 days caused increases of 72 and 74% in superoxide dismutase and catalase activities, respectively, in the brain homogenates. The treatment with this metal for 3 days increased brain homogenate chemiluminescence and thiobarbituric acid-reactive substances by 34 and 29%, respectively. The brain contents of the non-enzymatic antioxidants alpha-tocopherol and sulfhydryl groups decreased by 35 and 32%, respectively. Ascorbic acid levels were not modified by potassium dichromate. Finally, there was a significant increment in the mitochondrial production of oxidants in the brain of treated mice. These results suggest that chromium (VI) produces an increased formation of reactive oxygen species and brain lipid peroxidation. The increase in the antioxidant enzyme activities reflects an adaptive response against oxidative stress, while the reduction in the levels of nonenzymatic antioxidants might be due to their reaction with reactive oxygen species generated during the metabolism of chromium(VI) [34].
Beside its hazardous effects on the lungs, brain injury could be induced by the absorption of substances through the nasal membrane which provides a direct delivery to the brain [35]. The distribution and the effects of Cr in both brain and lung following the intranasal instillation of potassium dichromate in rats has been investigated. Simultaneously, the intraperitoneal rat model of acute Cr-toxicity was used for comparison with the intranasal exposure [35]. Thirty male Wistar rats were randomly placed into five groups (n=6); each received a single dose of saline, ip chromate (15 mg/kg), or chromate intranasally at three dose levels: 0.5, 1, or 2 mg/kg [35]. Locomotor activity was assessed before and 24 h after chromate administration. The lungs and brain were collected for biochemical, histopathological, and immunohistochemical investigations. Treatment of rats with ip chromate resulted in a 36% and 31% of the injected dose of Cr delivered to in the brain and lung, respectively. With intranasal chromate-treated rats, brain, Cr levels increased in a dose-dependent manner to reach 46% of the instilled highest dose. Moreover, only this high dose of intranasal chromate resulted in a delivery of a significant concentration of Cr (42%) to the lungs. The uppermost alteration in the rats locomotor activity as well as in the brain and lung histopathological features and contents of oxidative stress biomarkers, interleukin-1beta (IL-1beta), phosphorylated protein kinase B (PKB), and cyclooxygenase 2 (COX-2) were observed in the rats treated intranasally with chromate (2 mg/ kg). The findings revealed that these toxic manifestations were directly proportional to the delivered concentration of Cr to the tissue. In conclusion, the study showed that a comparably higher concentrations of Cr and more elevated levels of oxidative stress and inflammatory markers were observed in brain and lung tissues of rats subjected to intranasal at a dose that is 13% that given IP. Therefore, the study suggests a high risk of braintargeting injury among individuals environmentally or occupationally exposed to Cr dust intranasally, even at low doses, and also an additional risk of lung injury with higher Cr concentrations [35]. Chrome platers for example develop chrome holes in their nasal septum suggesting that a significant portion may enter the body by the intranasal route [2].
In addition to hexavalent chromate trivalent chromate has also been shown to enter the brain and produce toxicity at this site. An experiment was conducted to investigate oxidative stress in chickens exposed to various concentrations of chromium trichloride (CrCl3) in drinking water. Seventy-two Hylan Brown male chickens were randomly divided into four groups: three experimental groups and one control group [36]. The experimental groups were exposed to three different doses in their drinking water (50% LD50, 25% LD50, and 12.5% LD50) of CrCl3 mg/kg body weight for 42 days, while the control group was given the equivalent water. The activities of superoxide dismutase, catalase, and glutathione peroxidase and non-enzymatic antioxidants (glutathione, total antioxidant capacity, malondialdehyde, and hydrogen peroxide) were measured after obtaining brain samples. Results suggested that 50% LD50 chromium(III) significantly increased (p<0.05) the contents of malondialdehyde and hydrogen peroxide [36]. The antioxidant enzyme activities, total glutathione concentration, and total antioxidant capacity decreased significantly (p<0.05) compared with those of the controls and were consistent with the increase in dosage and time. Additionally, extensive histological alterations were observed in the chicken brain, such as the vacuolization and nuclear condensation of the neurons. These results indicated that exposure to high-dose CrCl3 for a certain time could induce the occurrence of oxidative stress and histological alterations in the brain of chickens [36].
Another study investigated the effects of supplemental chromium picolinate (CrPic) and chromium histidinate (CrHis) on nuclear factor-kappa B (NF-kappaB p65) and nuclear factor (erythroid-derived 2)-like 2 (Nrf2) signaling pathway in diabetic rat brain. Nondiabetic (n=45) and diabetic (n=45) male Wistar rats were either not supplemented or supplemented with CrPic or CrHisvia drinking water to consume 8 mug elemental chromium (Cr) per day for 12 weeks. Diabetes was induced by streptozotocin injection (40 mg/kg i.p., for 2 weeks) and maintained by high-fat feeding (40%) [37]. Diabetes was associated with increases in cerebral NF-kappaB and 4- hydroxynonenal (4-HNE) protein adducts and decreased in cerebral nuclear factor of kappa light polypeptide gene enhancer in B cells inhibitor, alpha (IkappaBalpha) and Nrf2 levels. Both Cr chelates were effective to decrease levels of NF-kappaB and 4- HNE protein adducts and to increase levels of IkappaBalpha and Nrf2 in the brain of diabetic rats [37]. However, responses of these increases and decreases were more notable when Cr was supplemented as CrHis than as CrPic. In conclusion, Cr may play a protective role in cerebral antioxidant defense system in diabetic subjects via the Nrf2 pathway by reducing inflammation through NF-kappaB p65 inhibition. Histidinate form of Cr was superior to picolinate form of Cr in reducing NF-kappaB expression and increasing Nrf2 expression in the brain of diabetic rats [37].
Another study was designed to investigate the susceptibility of liver and brain tissues, as insulin-dependent tissues, of normal adult male rats to the oxidative challenge of subchronic supplementation with chromium picolinate (CrPic) at low (human equivalent) and high doses (2.90 and 13.20 mug Cr kg(-1) day(-1), respectively) [38]. Also, the modulative effect of CrPic administration on the enhanced oxidative stress in the liver and brain tissues of alloxan-diabetic rats was investigated. Fasting serum glucose level was not modified in normal rats but significantly reduced in diabetic rats that had received CrPic supplement. A mild oxidative stress was observed in the liver and brain of CrPic-supplemented normal rats by a dosedependent reduction in the levels of hepatic and cerebral free fatty acids, superoxide dismutase and glutathione peroxidase activities, and increased tissue malondialdehyde concentration. On the other hand, hepatic and cerebral catalase activity was reduced in the high dose group only. CrPic supplementation did not act as a peroxisome proliferator confirmed by the significant reductions in liver and brain peroxisomalpalmitoyl CoA oxidase activity [38]. The non significant alterations in liver protein/DNA and RNA/DNA ratios indicate that CrPic did not affect protein synthesis per cell, and that mild elevations in hepatic total protein and RNA concentrations might be due to block or decrease in the export rate of synthesized proteins from the liver to the plasma. In diabetic rats, elevated levels of hepatic and cerebral free fatty acids and malondialdehyde, and in contrast the overwhelmed antioxidant enzymes, were significantly modulated in the low dose group and nearnormalized in the high dose group [38]. The significant increases observed in liver total protein and RNA concentrations, as well as protein/DNA and RNA/DNA ratios in diabetic rats supplemented with the high dose of Cr, compared to untreated diabetics, may be related to the improvement in the glycemic status of the diabetic animals rather than the direct effect of CrPic on protein anabolism [38].
Although, Cr(III) is no longer on the list of minerals necessary for the proper functioning of the human body, and its pharmacological effect is still unclear, a proposed purposes of Cr(III) administration is to use it in patients with mood disorders and this effect is strictly related to its pharmacological, not dietary effect [39]. This is because high doses are necessary to obtain such results and additionally, no deficiencies in human population have been noted [39]. In a study, the affinity of chromium(III) to selected receptors and transporters in the rat brain was evaluated, and the effect of the 14 days administration of this metal was assessed on the density of selected receptors. All analyses were performed in vitro using radioligand binding assays, and the results indicated lack of affinity to beta1 and alpha1 receptors and serotonin transporter (SERT), furthermore very weak affinity to the 5-HT1A receptor (30% inhibition at 10(-4) and 10(-5) M). [39]. Analysis of the alpha1 and beta1 adrenergic receptor density indicated lack of any adaptive effects after 14 days of Cr(III) administration through intraperitoneal injections (doses 6 and 12 mg/kg). The antidepressant activity of chromium(III) suggested in clinical trials involved patients with atypical, seasonal, or dystonic symptoms. This effect does not depend on direct affinity to serotonin receptors and transporter nor is the result of adaptive changes in the adrenoreceptor system [39].
Cadmium And The Brain
There is no question that Cd exposure during development and in early life enters the brain and produces a strong oxidative stress response damaging brain tissue. However, this review has focused on the effect of Cd in adult animals or humans.
Cadmium can enter the body through various mechanisms to induce neurotoxicity. When inhaled, Cd can affect the olfactory neurons and accumulate in the olfactory bulb before entering the brain, or accumulate in the lungs and enter circulation to damage the blood brain barrier. Although many investigators believe that Cd cannot cross the blood brain barrier in adults male albino rats of 21 days age were exposed to 10 p.p.m. cadmium (CdCl2 salt) in drinking water, ad libitum, for 90 days [40]. Brain cadmium levels increased by 76% (p<0.05) and 165% (p<0.001) respectively at 30 and 90 days of exposure compared to controls. Cadmium increased blood-brain barrier permeability of fluoroscein dye (24%, p<0.02) and the levels of brain microvessel malondialdehyde (31%, p<0.01) at 90 days of exposure. However, these parameters did not alter significantly at 30 days of exposure. Increased activities of microvessel superoxide dismutase (18%, p<0.02), glutathione peroxidase (20%, p<0.01) and catalase (28%, p<0.01) were observed at 30 days of exposure. The continuation of the Cd treatment for 90 days decreased the levels of superoxide dismutase (30%, p<0.001), glutathione peroxidase (23%, p<0.005), catalase (25%, p<0.005), glutathione reductase (18%, p<0.02), vitamin E (20%, p<0.01), glutathione (26%, p<0.01), ascorbic acid (18%, p<0.05) and ceruloplasmin (13%, p<0.05) in the microvessal preparation compared to controls (40). It appears that Cd-induced bloodbrain barrier dysfunction may be related to the depletion of microvessel antioxidant substances along with increase in lipid peroxidation at 90 days of exposure [40].Cadmium (Cd) is a highly toxic environmental pollutant released from the smelting and refining of metals and cigarette smoking. Oral exposure to cadmium may result in adverse effects on a number of tissues, including the central nervous system (CNS) [41]. In fact, its toxicity has been related to neurological disorders, as well as neurodegenerative diseases such as Alzheimer's and Parkinson's diseases. Under normal conditions, Cd barely reaches the brain in adults because of the presence of the blood-brain barrier (BBB); however, it has been demonstrated that Cd-dependent BBB alteration contributes to pathogenesis of neurodegeneration [41]. However, the mechanism underlying Cd-dependent BBB alteration remain obscure. The signaling pathway of Cd-induced tight junction (TJ), F-actin, and vimentin protein disassembly in a rat brain endothelial cell line (RBE4). RBE4 cells treated with 10 muM cadmium chloride (CdCl2) showed a dose and time-dependent significant increase in reactive oxygen species (ROS) production. This phenomenon was coincident with the alteration of the TJ zonula occludens-1 (ZO-1), F-actin, and vimentin proteins. The Cd-dependent ROS increase elicited the upregulation of GRP78 expression levels, a chaperone involved in endoplasmic reticulum (ER) stress that induces caspase-3 activation (41). Further signal profiling by the pannexin-1 (PANX1) specific inhibitor (10) Panx revealed a PANX1-independent increase in ATP spillage in Cd-treated endothelial cells. The results point out that a ROS-dependent ER stress-mediated signaling pathway involving caspase-3 activation and ATP release is behind the BBB morphological alterations induced by Cd [41].
Cadmium accumulation and metallothionein (MT) expression were studied in brains of adult mice as well as at different stages of development [42]. MT expression was also studied in the eye of adult mice as well as at different stages of development [42]. Using northern blot analysis with total RNA, MT mRNAs were not detected in day 16 through day 18 embryos or in postnatal animals up to day 14. Detectable expression of MT-I,-II, and-III mRNAs was obtained in brains of 30 and 60 days old mice [42]. The expression of MT-III mRNA appeared to be much stronger in adults (12 weeks old or more) than in 30 and 60 days old animals. In contrast, there was similar expression of MT-I and-II in 30 and 60 days old mice. Cd distribution to brain was found to decrease with age; the brains of 7 days old mice contained about 4-times more Cd than that of adult mice. Thus, an inverse correlation was observed between MT expression and Cd accumulation in brain [42]. Although Cd is known to be bound to MT and one would have expected more Cd with increasing MT it is likely that the ability of Cd to penetrate the brain during development may override the ability of higher levels of MT to sequester more metal in the brain [42].
Male albino rats of 21 days age were exposed to 10 p.p.m. cadmium (CdCl2 salt) in drinking water, ad libitum, for 90 days. Brain cadmium levels increased by 76% (p<0.05) and 165% (p<0.001) respectively at 30 and 90 days of exposure compared to controls [40]. Cadmium increased blood-brain barrier permeability of fluoroscein dye (24%, p<0.02) and the levels of brain microvessel malondialdehyde (31%, p<0.01) at 90 days of exposure. However, these parameters were not alter significantly at 30 days of exposure. Increased activities of microvessel superoxide dismutase (18%, p<0.02), glutathione peroxidase (20%, p<0.01) and catalase (28%, p<0.01) were observed at 30 days of exposure. The continuation of the Cd treatment for 90 days decreased the levels of superoxide dismutase (30%, p<0.001), glutathione peroxidase (23%, p<0.005), catalase (25%, p<0.005), glutathione reductase (18%, p<0.02), vitamin E (20%, p<0.01), glutathione (26%, p<0.01), ascorbic acid (18%, p<0.05) and ceruloplasmin (13%, p<0.05) in the microvessal preparation compared to controls. It appears that Cd-induced blood-brain barrier dysfunction may be related to the depletion of microvessel antioxidant substances along with increase in lipid peroxidation at 90 days of exposure [40].
Cadmium chloride-induced DNA damage was investigated in individual brain, kidney and liver cells isolated from rats gavaged 14 mg/kg/day cadmium chloride [43]. Animals were sacrificed on days 2, 4, 8, 16, and 33, and DNA damage was determined using an alkaline microgel electrophoresis technique. Data for DNA migration from 50 randomly selected cells clearly show significant increases in DNA damage in cells from three different organs of cadmium chloride gavaged animals compared to saline treated control animals (33 day control, brain 64.7+/-5.3, kidney 75.5+/-9.4, liver 67.9+/-5.7 microm; 33 days experimental, brain 284.3+/-16.9, kidney 397.9+/-11.3, liver 315+/-22.5 microm; these values represent length of exposure in days and length of DNA migration in micron. There was an increase in DNA damage for all three cell types, with increasing duration of treatment. Cadmium induced levels of DNA single strand breaks were more pronounced in kidney cells than in cells from the other two organs. Body and organ weights decreased of treated animals were decreased as compared to control. Results of this study indicate a potential of cadmium to be a genotoxic compound [43].
Many plant foods are rich sources of rutin, a flavonoid with many biological activities and health benefits. Exposure to cadmium has been implicated in neurotoxicity and cognitive dysfunction in animal models [44]. However, there is a little information available on the effect of rutin on the cadmium bioavailability in the brain. Animals were divided into six groups (n=6): group 1 served as control, groups 2 and 3 are normal rats received 25 and 50 mg/kg of rutin respectively, group 4 received cadmium (5 mg/kg), while groups 5 and 6 are cadmium-exposed rats treated with 25 and 50 mg/kg rutin respectively via oral administration for 21 days. Rutin was administered 30 min after cadmium administration each day. The spatial working memory of the exposed and treated rats was assessed using Morris water maze and Y-Maze tasks. Furthermore, the residual level of cadmium ion in the brain of the rats was estimated. The cholinesterase (AChE and BChE) activities and nitric oxide level were determined and level of oxidative stress markers (ROS and MDA) was assessed. Results revealed that rutin significantly reduced cadmium bioavailability in the brain [44]. Cadmium increased cholinesterase (AChE and BChE) activities and level of oxidative stress markers in the brain, with a concomitant decrease in nitric oxide level. However, treatment with rutin decreased cholinesterase activities and the level of oxidative stress markers in cadmium-exposed rats. Also, rutin improved spatial working memory and learning processes as revealed by Morris water maze and Y-Maze tasks. Conclusively, rutin could be considered to possess cognitive-enhancing properties possibly through alterations of cadmium bioavailability in the brain of cadmium-exposed rats [44].
Whereas cadmium is a toxicant that has been shown to cause cardiovascular toxicity and mortality in mammals, few mechanistic studies address its acute circulatory actions. The present study assessed the hypothesis that cadmium effects dosedependent acute circulatory fates via differential participation of the cardiovascular regulatory mechanisms in brain [45]. In Sprague-Dawley rats maintained under propofol anesthesia, cadmium acetate (8 mg/kg, iv) induced significantly high mortality rate within 10 min, concomitant with progressive decline toward zero level of mean arterial pressure (MAP), heart rate (HR), baroreflex-mediated sympathetic vasomotor tone, and carotid blood flow (CBF). There were concurrent tissue anoxia, cessation of microvascular perfusion, reduction of mitochondrial membrane potential and ATP production, and necrotic cell death in the rostral ventrolateral medulla (RVLM), the brain stem site that maintains blood pressure and sympathetic vasomotor tone (45). On the other hand, a lowerdose of cadmium (4 mg/kg, iv) resulted in only a transient decrease in MAP that was mirrored by an increase in CBF and baroreflex-mediated sympathetic vasomotor tone, minor changes in HR, along with transient hypoxia, and apoptotic cell death in RVLM. Cadmium elicits dose-dependent acute cardiovascular effects with differential underlying biochemical and neural mechanisms. At a higher-dose, cadmium induces high mortality by effecting acute cardiovascular collapse via anoxia, diminished tissue perfusion, mitochondrial dysfunction and bioenergetics failure that echo failure of cerebral autoregulation, leading to necrosis, and loss of functionality in RVLM [45]. On the other hand, a lower-dose of cadmium elicits low mortality, transientdecrease in arterial pressure, and hypoxia and apoptosis in RVLM that reflect sustained cerebral autoregulation.
To investigate the underlying mechanism of neurotoxicity of cadmium, the effects of intraperitoneal injection of cadmium on messenger RNA (mRNA) expression of Bcl-2 (B-cell lymphoma 2) and Bax (Bcl-2-associated x) genes and caspase-3/7 activation in rat hippocampus and frontal cortex [46]. Twenty-eight male Wistar rats weighing 200-250 g were randomly divided into four groups. Control group received saline and three other groups received cadmium at doses of 1, 2 and 4 mg/kg (body weight) for 15 successive days. One day after the last injection, the hippocampus and frontal cortex were dissected and removed and then the expression of Bcl-2 and Bax genes was evaluated using real-time polymerase chain reaction and apoptotic studies was done using caspase-3/7 activation assay (46). Cadmium reduced the mRNA level of Bcl-2 in the control group at doses of 1 (p<0.01), 2 and 4 mg/kg ( p<0.001) in rat hippocampus and cortex cells [46]. The mRNA level of Bax increased significantly compared to the control group at the doses of 1 (p<0.05), 2 and 4 mg/kg (p<0.001) in rat hippocampus. The mRNA level of Bax was increased significantly compared to the control group at the doses of 2 and 4 mg/kg (p<0.001) in rat cortex cells. Cadmium increased caspase-3/7 activity at doses of 1, 2 and 4 mg/kg in rat hippocampus. Caspase-3/7 activity was increased significantly at dose of 4 mg/kg in rat cortex. This decreased Bcl-2/Bax mRNA ratio induces cell apoptosis. Apoptotic effect of cadmium may be through the mitochondrial pathway by the activation of caspase-3/7 [46].
Cadmium (Cd) exposure can induce acute lethal health-related threats in humans since it has an exceptional ability to accumulate in living organism tissues and cause toxicological effects. Curcumin (Cur) on the other hand has a wide variety of biological activities and several studies have suggested its potential therapeutic or protective effects against several ailments and infections. To study the effect of Cur on the toxicity of Cd, Swiss-Webster strain male and female mice (sixty each) were divided into 6 groups of ten each at random. Group-1 served as the naive control and received no treatment. Group-2, 3 and 4 were the experimental controls and were administered once a day with a single oral dose of 50% dimethyl sulfoxide (DMSO), Cur (300 mg/kg) or Cd (100 mg/kg) respectively, for 2 weeks. Group-5 and 6 received Cur and Cd in combination once a day orally for 2 weeks except that Cur in a dose of 150 and 300 mg/kg to group 5 and 6 respectively, was administered one hour before Cd administration to both groups [47]. After treatment period, the male animals were subjected to social standard opponent test and females were subjected to the tube restraint tests and thereafter, their blood was collected to measure the blood composition indices and level of reproductive hormones. The animals were sacrificed to collect their brain for the estimation of acetylcholinesterase (AChE). Results indicated that Cd significantly increased nonsocial activities in males and latency to first bite in females, whereas the social activities in males and the number of bites in females were significantly decreased. All measured indices of blood composition and levels of progesterone (female) and testosterone (male) in blood and AChE in their brain tissues were significantly decreased due to Cd treatment. However, administration of Cur along with Cd had an ameliorating effect on all the behavioral and biochemical parameters studied herein and reduced the toxicity of Cd significantly and dose-dependently. Thus, Cur may be beneficial for general health and for protection from Cd intoxication [47].
Arsenic And The Brain
Arsenic is identified as a known carcinogen and ubiquitously exists in nature. It appears that accumulation of inorganic arsenic (iAs) and its methylated metabolites in various tissues is closely correlated with the long-term toxicity and carcinogenicity of this metalloid. Although there are many studies showing that arsenic effects the brain in developing embryos, this review has focused on studies showing the effect of arsenic in adult animals or humans. Arsenic exposure is associated with encephalopathy and neuropathy. Analysis of various arsenic species in murine tissues, especially in the cerebral cortex, cerebellum, and hippocampus, were determined after long-term exposure to 25, 50, 100, and 200 mg/L sodium arsenite in drinking water for 1 and 12 months [48]. Data showed that the amount of total arsenic (TAs) increased in an obvious dose-dependent manner in various tissues, and total As levels were in the order of urinary bladder>brain>lung>liver>kidney>spleen. Furthermore, iAs(III) and DMA could be observed in all tissues and brain regions with DMA being the predominant metabolite. The bladder, brain, and lung contained the higher levels of DMA, while the liver, kidney, and spleen accumulated a higher proportion of iAs(III). MMA was preferentially accumulated in the lung and bladder of mice regardless of arsenic exposure doses or duration. Higher levels of MMA were observed in the hippocampus, which was distinguished from the cerebral cortex and cerebellum. Together with these results, this study clearly demonstrates that the accumulation of iAs and its methylated metabolites is tissue-specific and even not homogeneous among different brain regions in mice by long-term exposure to arsenite. The study thus provides crucial information for recognizing arsenical neurotoxicity, and reducing the uncertainty in the risk assessment for this toxic metalloid [48]. Although most of the methylated arsenic is thought to come from the liver other tissues including the brain have the Asmethylating enzyme arsenic methyl transferase.
Another study examined the associations between arsenic exposure and adult cognitive impairment using the Mini-Mental State Examination (MMSE) and the serum levels of brainderived neurotrophic factor (BDNF), a potential biomarker of cognitive health status [49]. A cross-sectional study recruited 693 adult (18-60 years old) subjects from the areas of low and high arsenic exposure in rural Bangladesh. The subjects' arsenic exposure levels (drinking water, hair, and nail arsenic concentrations) were measured by inductively coupled plasmamass spectroscopy. The Bangla version of the MMSE was used as a cognitive assessment tool. Serum BDNF (sBDNF) levels were assessed by immunoassay. The average MMSE score and sBDNF level of the subjects in arsenic-endemic areas were significantly (p<0.001 for both) lower than those of the subjects in nonendemic area. Analyses revealed that both MMSE scores and sBDNF levels were decreased with the increasing concentrations of arsenic in drinking water, hair, and nails in a dose-dependent fashion. In regression analyses, significant associations of arsenic exposure metrics with MMSE scores and sBDNF levels were observed even after adjustment for several variables. MMSE scores showed a significantly positive correlation with sBDNF levels. The findings demonstrate that chronic exposure to arsenic dose-dependently decreases cognitive function in adults, with a concomitant reduction of sBDNF levels. A decreased BDNF level may be part of the biochemical basis of chronic arsenic exposure-related cognitive impairment [49].
A study was conducted to evaluate the neurotoxic effect of arsenic in Swiss albino mice and its amelioration by Vitamin E, Coenzyme Q10 and their combination. Swiss albino mice were treated with arsenic of 136 ppm for 15 days. The daily dose is 1/3 of LD 50 [50]. Thereafter, the animals were maintained either on drinking water or treated with Vitamin E (50 mg/kg bwt), Coenzyme Q10 (10 mg/kg bwt), and their combination by i.p.daily for 15 days. After the treatment, animals were sacrificed. The weight of the brain was marginally lower (ns), in arsenic-treated group as compared to control and antioxidantprotected groups. Lipid peroxidation level was higher in arsenictreated group, A significant reduction was found in GSH level in the brain of arsenic-treated mice whereas GSH level was considerably higher in antioxidant groups. Further, total thiol and total protein level were lower in arsenic-treated group. However, total thiol was significantly higher in antioxidantprotected groups. Catalase activity was significantly lower while SOD activity was marginally lowered in arsenic-treated group, and it was slightly higher in antioxidant-protected groups [50]. Further, reduction in acetylcholinesterase, autyrylcholinesterase and motor coordination activity were also observed in arsenictreated groups. Whereas, a higher AChE, BChE, and motor coordination activity was observed in antioxidant-protected group. These data indicate a positive role of selected antioxidant against the toxicity of arsenic in the brain of mice.
Another study was carried out to investigate the molecular mechanism of arsenic-induced mitochondrial oxidative damage and its relation to biogenesis in rat brain. Chronic sodium arsenite (25 ppm, orally) administration for 12 weeks decreased mitochondrial complexes activities and mRNA expression of selective complexes subunits [51]. The expression of mitochondrial biogenesis regulator PGC-1alpha, and its downstream targets NRF-1, NRF-2 and Tfam were decreased significantly both at mRNA and protein levels suggesting impaired biogenesis following chronic arsenic-exposure [51]. In addition to this, protein expression analysis also revealed activation of Bax and caspase-3, leading to translocation of cytochrome c from mitochondria to cytosol suggesting induction of apoptotic pathway under oxidative stress. This was further confirmed by electron microscopy, which depicted morphological changes in mitochondria including altered nuclear and mitochondrial shape and chromatin condensation in arsenic-treated rats [51]. The immunohistochemical studies showed both nuclear and cytosolic localization of NRF-1 and NRF-2 in arsenic-exposed rat brain further suggesting regulatory role of these transcription factors in arsenic neurotoxicity. Arsenic-induced mitochondrial oxidative damage was associated with decreased mitochondrial biogenesis in rat brain that may bean be an important target in the mechanism for arsenicinduced neurotoxicity [51].
Using rodent models, it is possible to demonstrate As accumulation in the brain that leads to defects in operant learning, behavioral changes, and effect on pituitary gonadotrophins. iAsbiomethylation in the CNS is a significant process, yielding products that are more reactive and toxic than the parent compound. Mice received 2.5, 5, and 10 mg/kg/day sodium arsenite orally for 9 days [52]. The distribution of iAs and its metabolites as well as the mRNA and protein expression of arsenic (III) methyltransferase (AS3MT), which encodes the key enzyme in iAs metabolism, was present in the cerebral cortex, hippocampus, striatum, mesencephalon, thalamus, cerebellum, hypothalamus, pons, medulla oblongata, and pituitary of mouse brain [52]. Findings show that methylated As metabolites are present in all brain regions studied suggesting that AS3MT is ubiquitously expressed in the brain and it is not inducible by arsenite. There is also a dose-related accumulation of As species in all brain regions, with the highest accumulation observed in the pituitary. The higher distribution of arsenicals in pituitary can help to explain the neuroendocrine effects associated with iAs exposure [52]. Although arsenic methyltransferase protein and mRNA is present in different brain regions the liver is clearly the major organ that methylates arsenic.
Arsenic exposure induces overproduction of reactive nitrogen species (RNS) in brain tissue and results in nucleic acid damage to the nerve cells. The 8-nitroguanine is one of the major products formed by the reaction of guanine, and ONOO-, and has been used as a popular biomarker of nucleic acid damage due to RNS attacking. In the present study examined whether the administration of taurine can protect against nucleic acid damage of brain neurons by arsenic-induced RNS [53]. Sixty mice (30 male and 30 female) weighing 19.5+/-1.5 g were divided into 3 groups: (1) control group, experimental group that received arsenic (As2O3), and antagonistic group that received taurine with arsenic. Arsenic was administered for 60 days. 8-Nitroguanine expressions in brain neurons of mice were examined by the immunohistochemical method in cerebrum and cerebellum of mice. In the control group, no abnormal histopathological changes were observed in brain tissue. In brains of mice exposed to arsenic, histopathological results showed swells, evident vacuolar degeneration in cytoplasm, karyorrhexis and karyolysis. Relatively light pathological changes were observed in brain of the mice co-administered arsenic and taurine. Little or no expression of 8-nitroguanine in brain tissue was observed in controls. However, intensive expression of 8- nitroguanine was found in brain tissue of mice exposed to arsenic and it was mainly distributed in nucleus neighboring the nuclear membrane, but also in cytoplasm. A weak expression of 8-nitroguanine was observed in brain cells of mice coadministered arsenic and taurine [53]. The brain neurons may be the major target cells of arsenic neurotoxicity. Coadministration of arsenic and taurine can alleviate DNA damage of brain neurons caused by arsenic through the RNS signal pathway.
The understanding of the biomethylation process of arsenic is essential to uncover the mechanisms of arsenic toxicity [54]. A study analyzed the time course of arsenic species in the brain and liver of adult mice, after a single oral administration of three arsenate doses [2.5, 5.0 and 10 mg As(V)/kg]. Quantification of arsenic species was performed by means of liquid chromatography coupled to atomic fluorescence 2, 5, 8, 12 and 24 h after administration. The results show that 2 h after arsenate administration inorganic arsenic arrives to the liver and its concentration diminishes gradually until becoming nondetectable at 12 h [54]. Arsenic takes longer to appear in the brain and it is present only as dimethyl arsenic acid. Since arsenic concentration decreases in liver while it increases in the brain, this suggests that the arsenic metabolite reaches the brain after formation in the liver. Importantly, the fact that dimethyl arsenic acid is no longer present after 24 h suggests the existence of a mechanism to clear this metabolite from brain tissue.
Nickel And The Brain
Nickel (Ni) is an environmental pollutant towards which human exposure can be both occupational (mainly through inhalation) and dietary (through water and food chain-induced bioaccumulation). The overexposure to nickel due to the extensive use of it in modern technology remains a major public health concern. The mechanisms of pathological effects of this metal remain elusive. The nervous system is highly susceptible to Ni toxicity as it may enter the brain through the blood-brain barrier and the olfactory bulb to then accumulate in the cerebral cortex and the brain as a whole. In evaluation the neurotoxic effects of Ni we focused on studies using adult animals or humans since developing animals or pup have poorly developed blood brain barriers and many toxic metals may reach the brain that could be excluded in adults. This is the case with lead for example. A study was devoted to evaluate the effect of nickel on the oxidative state of the brain cells of mice and to assess whether zinc as redox state modulator could efficiently protect cells against nickel's neurotoxicity [55]. As oxidative stress biomarkers in the present study, the concentrations of reduced glutathione, metallothioneins, and malondialdehyde and the activity of the enzyme delta-aminolevulinatedehydratase were utilized. For single metal exposure, mice were i.p. injected once with solutions of NiCl2 and/or ZnSO4; repeated exposure was performed i.p. injecting metal salt solutions for 14 days [55]. The control mice received i.p. injections of saline. Results of our study demonstrate that single and 14 days of Ni2+ exposure decreased reduced glutathione and increased malondialdehyde contents in the brain of mice. Repeated Ni2+ administration significantly inhibited delta-aminolevulinatedehydratase while increasing brain metallothionein concentration at both exposure periods. Zinc exhibited a protective effect against nickel-induced glutathione and lipid peroxidation in brain cells of mice at both intervals of time, while repeated exposure to this metal significantly raised the brain metallothionein content. Repeated Zn2+ pretreatment protected deltaaminolevulinatedehydratase from Ni2+-induced inhibition and significantly increased metallothionein concentration at both investigated time intervals [55]. It is not clear from this study why Zn administration did not increase metallothionein but it may be that because Zn is an essential nutrient and Ni is not the body limits the amount of Zn that may be retained and enter the brain.
A study investigated the effects of short-term Ni-administration (as NiCl2, 13 mg/kg) on the adult rat whole brain total antioxidant status (TAS) and the activities of acetylcholinesterase (AChE), Na+,K+-ATPase, and Mg2+-ATPase; in addition, the potential effect of the co-administration of the antioxidant Lcysteine (Cys, 7 mg/kg) on the above parameters was studied [56]. Twenty-eight male Wistar rats were divided into four groups: A (saline-treated control), B (Ni), C (Cys), and D (Ni and Cys). All rats were treated once daily with intraperitoneal injections of the tested compounds, for 1-week. Rats were sacrificed by decapitation and the above-mentioned parameters were measured spectrophotometrically [56]. Rats treated with Ni exhibited a significant reduction in brain TAS (-47%, p<0.001, Bvs. A) that was efficiently limited by the co-administration of Cys (-4%, p>0.05, Dvs. A; +83%, p<0.001, Dvs. B), while Cys (group C) had no effect on TAS. The rat brain AChE activity was found significantly increased by both Ni (+30%, p<0.001, Bvs. A) andCys (+62%, p<0.001, Cvs. A), while it tended to adjust to control levels by the co-administration of Ni and Cys (+13%, p<0.001, Dvs. A;-13%, p<0.001, Dvs. B). The activity of rat brain Na(+),K(+)-ATPase was significantly decreased by Niadministration (-49%, p<0.001, Bvs. A), while Cys supplementation could not reverse this decrease (-44%, p<0.001, Dvs. A). The activity of Mg2+-ATPase was not affected by Niadministration (-3%, p>0.05, Bvs. A), but was significantly reduced when combined with Cys administration (-17%, p<0.001, Dvs. A). The above findings suggest that Ni short-term invivo administration causes a statistically significant decrease in the rat brain TAS and an increase in AChE activity. Both effects can be, partially or totally, reversed to control by Cys coadministration; Cyscould thus be considered as a potential neuroprotective agent against chronic exposure to Ni. The activity of Na(+),K(+)-ATPase that was inhibited by Ni, could not be reversed by Cys co-administration [56,57]. Although Ni ions bind to both cysteine and histidine, the affinity of Ni for histidine is greater than cysteine, but these effects may not only depend on chelation but also the antioxidant potential of Cys and His.
Conclusion
The effect of L-ascorbic acid and alpha-tocopherol supplementation on plasma and whole brain nitric oxide level and antioxidant status in nickel sulfate or lead acetate treated male albino rats. Nitric oxide and lipid peroxide levels in whole brain tissue and plasma increased following nickel and lead treatment but significantly returned to near-normal values upon L-ascorbic acid or alpha-tocopherol supplementation. In brain tissue, antioxidant enzymes superoxide dismutase, glutathione peroxidase, glutathione peroxidase, and catalase along with the glutathione level decreased significantly after both treatments but significantly improved upon simultaneous supplementation with L-ascorbic acid or alpha-tocopherol. Lead-treated animals showed a greater improvement with alpha-tocopherol, whereas nickel-treated rats showed a greater improvement with L-ascorbic acid. In both groups, combined supplementation with Lascorbic acid and alpha-tocopherol did not change the percentage improvement in comparison with supplementation with a single vitamin alone.
Acknowledgements
This work was supported by NIH grants: ES000260, ES022935, ES023174, ES026138
REFERENCES
- Chervona Y, Arita A, Costa M. Carcinogenic metals and the epigenome: Understanding the effect of nickel, arsenic, and chromium. Metallomics. 2012;4(7): 619-627.
- Costa M, Klein CB. Toxicity and carcinogenicity of chromium compounds in humans. Crit Rev Toxicol. 2006;36(2):155-163.
- DesMarais TL, Costa M. Mechanisms of chromium-induced toxicity. CurrOpinToxicol. 2019;14(4):1-7.
- Mahmoud AM, Abd El-Twab SM. Caffeic acid phenethyl ester protects the brain against hexavalent chromium toxicity by enhancing endogenous antioxidants and modulating the JAK/STAT signaling pathway. Biomed Pharmacother. 2017;91(7):303-311.
- Zhitkovich A, Voitkun V, Kluz T, Costa M. Utilization of DNA-protein cross-links as a biomarker of chromium exposure. Environ Health Perspect. 1998;106(4):969-974.
- Sheffet A, Thind I, Miller AM, Louria DB. Cancer mortality in a pigment plant utilizing lead and zinc chromates. Arch Environ Health. 1982;37(7): 44-52.
- Cohen MD, Kargacin B, Klein CB, Costa M. Mechanisms of chromium carcinogenicity and toxicity. Crit Rev Toxicol. 1993;23(3):255-281.
- Costa M. Review of arsenic toxicity, speciation and polyadenylation of canonical histones. ToxicolApplPharmacol. 2019;375(7):1-4.
- Huang C, Ke Q, Costa M, Shi X. Molecular mechanisms of arsenic carcinogenesis. Mol Cell Biochem. 2004;255(1):57-66.
- Brocato J, Chen D, Liu J, Fang L, Jin C, Costa M. A potential new mechanism of arsenic carcinogenesis: depletion of stem-loop binding protein and increase in polyadenylated canonical histone h3.1 mrna.Biol Trace Elem Res. 2015;166(4):72-81.
- Brocato J, Costa M. 10th NTES Conference: Nickel and Arsenic Compounds Alter the Epigenome of Peripheral Blood Mononuclear Cells. J Trace Elem Med Biol. 2015;31(7):209-213.
- Brocato J, Fang L, Chervona Y, Chen D, Kiok K, Sun H, et al. Arsenic induces polyadenylation of canonical histone mRNA by down-regulating stem-loop-binding protein gene expression. J Biol Chem. 2014;289(9):31751-31764.
- Huff J, Lunn RM, Waalkes MP, Tomatis L, Infante PF. Cadmium-induced cancers in animals and in humans. Int J Occup Environ Health. 2007;13(2):202-212.
- Costa M, Mollenhauer HH. Phagocytosis of nickel subsulfide particles during the early stages of neoplastic transformation in tissue culture. Cancer Res. 1980;40(8):2688-2694.
- Oller AR, Costa M, Oberdorster G. Carcinogenicity assessment of selected nickel compounds. ToxicolApplPharmacol. 1997;143(11):152-166.
- Costa M, Davidson TL, Chen H, Ke Q, Zhang P, Yan Y, et al. Nickel carcinogenesis: Epigenetics and hypoxia signaling. Mutat Res. 2005;592(2):79-88.
- Costa M, Mollenhauer HH. Carcinogenic activity of particulate nickel compounds is proportional to their cellular uptake. Science. 1980;209(4455):515-517.
- Costa M., Simmons-Hansen J, Bedrossian CW, Bonura J, Caprioli RM. Phagocytosis, cellular distribution, and carcinogenic activity of particulate nickel compounds in tissue culture. Cancer Res. 1981;41(7):2868-2876.
- Evans RM, Davies PJ, Costa M. Video time-lapse microscopy of phagocytosis and intracellular fate of crystalline nickel sulfide particles in cultured mammalian cells. Cancer Res. 1982;42(7):2729-2735.
- Costa M, Heck JD. Perspectives on the mechanism of nickel carcinogenesis. AdvInorgBiochem. 1984;6(53):285-309.
- Costa M, Abbracchio MP, Simmons-Hansen J. Factors influencing the phagocytosis, neoplastic transformation, and cytotoxicity of particulate nickel compounds in tissue culture systems. Toxicol Appl Pharmacol. 1981;60(2):313-323.
- Costa M. Sequential events in the induction of transformation in cell culture by specific nickel compounds. Biol Trace Elem Res. 1983;5(8):285-295.
- Davidson T, Chen H, Garrick MD, D'Angelo G, Costa M. Soluble nickel interferes with cellular iron homeostasis. Mol Cell Biochem. 2005; 279(3):157-162.
- Chen H, Costa M. Iron and 2-oxoglutarate-dependent dioxygenases: An emerging group of molecular targets for nickel toxicity and carcinogenicity. Biometals. 2009;22(5):191-196.
- Chen H, Ke Q, Kluz T, Yan Y, Costa M. Nickel ions increase histone H3 lysine 9 dimethylation and induce transgene silencing. Mol Cell Biol. 2006;26():3728-3737.
- Ellen TP, Kluz T, Harder ME, Xiong J, Costa M. Heterochromatinization as a potential mechanism of nickel-induced carcinogenesis. Biochemistry. 2009;48(21):4626-4632.
- Kaur P, Garg T, Rath G, Goyal AK. In situ nasal gel drug delivery: A novel approach for brain targeting through the mucosal membrane. Artif Cells NanomedBiotechnol. 2016;44(4):1167-1176.
- Mustafa G, Alrohaimi AH, Bhatnagar A, Baboota S, Ali J, Ahuja A. Brain targeting by intranasal drug delivery (INDD): A combined effect of trans-neural and para-neuronal pathway. Drug Deliv. 2016;23(3):933-939.
- Fatima R, Akhtar K, Hossain MM, Ahmad R. Chromium oxide nanoparticle-induced biochemical and histopathological alterations in the kidneys and brain of Wistar rats. ToxicolInd Health. 2017;33(12) 911-921.
- Shaw P, Mondal P, Bandyopadhyay A, Chattopadhyay A. Environmentally relevant concentration of chromium induces nuclear deformities in erythrocytes and alters the expression of stress-responsive and apoptotic genes in brain of adult zebrafish. Sci Total Environ. 2020;703(2):135622.
- Duckett S. Abnormal deposits of chromium in the pathological human brain. J NeurolNeurosurg Psychiatry. 1986;49(3):296-301.
- Hao P, Zhu Y, Wang S, Wan H, Chen P, Wang Y, et al. Selenium administration alleviates toxicity of chromium(vi) in the chicken brain. Biol Trace Elem Res. 2017;178(8):127-135.
- Soudani N, Troudi A, Amara IB, Bouaziz H, Boudawara T, Zeghal N. Ameliorating effect of selenium on chromium (VI)-induced oxidative damage in the brain of adult rats. J PhysiolBiochem. 2012;68(1):397-409.
- Travacio M, Polo JM, Llesuy S. Chromium (VI) induces oxidative stress in the mouse brain. Toxicology. 2001;162(2):139-148.
- Salama A, Hegazy R, Hassan A. Intranasal Chromium Induces Acute Brain and Lung Injuries in Rats: Assessment of Different Potential Hazardous Effects of Environmental and Occupational Exposure to Chromium and Introduction of a Novel Pharmacological and Toxicological Animal Model.PLoS One. 2016;11(8): 0168688.
- Cheng J, Fan W, Zhao X, Liu Y, Cheng Z, Liu Y. Oxidative stress and histological alterations of chicken brain induced by oral administration of chromium(iii).Biol Trace Elem Res. 2016;173(1):185-193.
- Sahin K, Tuzcu M, Orhan C, Gencoglu H, Ulas M, Atalay M, et al. The effects of chromium picolinate and chromium histidinate administration on NF-kappaB and Nrf2/HO-1 pathway in the brain of diabetic rats. Biol Trace Elem Res. 2012;150(3):291-296.
- Refaie FM, Esmat AY, Mohamed AF, AboulNour WH. Effect of chromium supplementation on the diabetes induced-oxidative stress in liver and brain of adult rats. Biometals. 2009;22(4):1075-1087.
- Piotrowska A, Siwek A, Wolak M, Nowak G. Analysis of Density Changes of Selected Brain Receptors After a 14-Days Supply of Chromium(III) and Evaluation of Chromium(III) Affinity to Selected Receptors and Transporters.Biol Trace Elem Res. 2020;196(10):359-364.
- Shukla A, Shukla GS, Srimal RC. Cadmium-induced alterations in blood-brain barrier permeability and its possible correlation with decreased microvessel antioxidant potential in rat. Hum ExpToxicol. 1996;15(3):400-405.
- Mimouna SB, Chemek M, Boughammoura S, Banni M, Messaoudi I. Early-Life Exposure to Cadmium Triggers Distinct Zn-Dependent Protein Expression Patterns and Impairs Brain Development.Biol Trace Elem Res. 2018;184(6):409-421.
- Choudhuri S, Liu WL, Berman NE, Klaassen CD. Cadmium accumulation and metallothionein expression in brain of mice at different stages of development. ToxicolLett. 1996;84(3):127-133.
- Latinwo LM, Ikediobi CO, Singh NP, Sponholtz G, Fasanya C, Riley L. Comparative studies of in vivo genotoxic effects of cadmium chloride in rat brain, kidney and liver cells. Cell MolBiol (Noisy-le-grand). 1997;43(2):203-210.
- Oboh G, Adebayo AA, Ademosun AO, Olowokere OG. Rutin restores neurobehavioral deficits via alterations in cadmium bioavailability in the brain of rats exposed to cadmium. Neurotoxicology. 2020;77(3):12-19.
- Chen SM, Phuagkhaopong S, Fang C, Wu JCC, Huang YH, Vivithanaporn P, et al. Dose-Dependent Acute Circulatory Fates Elicited by Cadmium Are Mediated by Differential Engagements of Cardiovascular Regulatory Mechanisms in Brain. Front Physiol. 2019;10(4):772.
- Mahdavi S, Khodarahmi P, Roodbari NH. Effects of cadmium on Bcl-2/Bax expression ratio in rat cortex brain and hippocampus. Hum ExpToxicol. 2018;37(3):321-328.
- Abu-Taweel GM. Effects of curcumin on the social behavior, blood composition, reproductive hormones in plasma and brain acetylcholinesterase in cadmium intoxicated mice. Saudi J Biol Sci. 2016; 23(2):219-228.
- Li J, Guo Y, Duan X, Li B. Tissue and region-specific accumulation of arsenic species, especially in the brain of mice, after long-term arsenite exposure in drinking water.Biol Trace Elem Res. 2020;96(1):39.
- Karim Y, Siddique AE, Hossen F, Rahman M, Mondal V, Banna HU, et al. Dose-dependent relationships between chronic arsenic exposure and cognitive impairment and serum brain-derived neurotrophic factor. Environ Int. 2019;131(10):105029.
- Sharma A, Kshetrimayum C, Sadhu HG, Kumar S. Arsenic-induced oxidative stress, cholinesterase activity in the brain of Swiss albino mice, and its amelioration by antioxidants Vitamin E and Coenzyme Q10. Environ SciPollut Res Int. 2018;25(4):23946-23953.
- Prakash C, Kumar V. Arsenic-induced mitochondrial oxidative damage is mediated by decreased PGC-1alpha expression and its downstream targets in rat brain. ChemBiol Interact 2016;256(8): 228-235.
- Sanchez-Pena LC, Petrosyan P, Morales M, Gonzalez NB, Gutierrez-Ospina G, Del Razo LM, et al. Arsenic species, AS3MT amount, and AS3MT gene expression in different brain regions of mouse exposed to arsenite. Environ Res. 2010;110(5):428-434.
- Ma N, Sasoh M, Kawanishi S, Sugiura H, Piao F. Protection effect of taurine on nitrosative stress in the mice brain with chronic exposure to arsenic. J Biomed Sci. 2010;17 (1):7.
- Juarez-Reyes A, Jimenez-Capdeville ME, Delgado JM, Ortiz-Perez D. Time course of arsenic species in the brain and liver of mice after oral administration of arsenate. Arch Toxicol. 2009;83(2): 557-563.
- Sulinskiene J, Bernotiene R, Baranauskiene D, Naginiene R, Staneviciene I, Kasauskas A, et al. Effect of zinc on the oxidative stress biomarkers in the brain of nickel-treated mice.Oxid Med Cell Longev. 2019;2019(4): 8549727.
- Liapi C, Zarros A, Theocharis S, Voumvourakis K, Anifantaki F, Gkrouzman E, et al. Short-term exposure to nickel alters the adult rat brain antioxidant status and the activities of crucial membrane-bound enzymes: Neuroprotection by L-cysteine. Biol Trace Elem Res. 2011;143(3):1673-1681.
- Das KK, Saha S. L-ascorbic acid and alpha tocopherol supplementation and antioxidant status in nickel-or lead-exposed rat brain tissue. J Basic Clin Physiol Pharmacol. 2010;21(2):325-346.
Citation: Costa M, Ortiz A (2020) The Toxicity of Carcinogenic Metals to the Brain. J Carcinog Mutagen. 11:354. DOI: 10.35248/2157-2518.20.11.354
Copyright: © 2020 Costa M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Sources of funding : This work was supported by NIH grants: ES000260, ES022935, ES023174, ES026138