Indexed In
- The Global Impact Factor (GIF)
- CiteFactor
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- Virtual Library of Biology (vifabio)
- International committee of medical journals editors (ICMJE)
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Review Article - (2024) Volume 23, Issue 3
The significance of denture hygiene related to denture stomatitis-A review.
Ray Galvan1*, Michael Mc Bride1, Tom V. Korioth1 and Franklin Garcia-Godoy22Department of Bioscience Research, University of Tennessee, Memphis, USA
Received: 24-Jun-2020, Manuscript No. OHDM-24-5111; Editor assigned: 29-Jun-2020, Pre QC No. OHDM-24-5111 (PQ); Reviewed: 13-Jul-2020, QC No. OHDM-24-5111; Revised: 02-Sep-2024, Manuscript No. OHDM-24-5111 (R); Published: 30-Sep-2024
Abstract
The wear of dentures carries with it the possibility of an inflammatory response by the denture-bearing tissues. Lack of hygiene or improper hygiene has been shown to contribute to denture stomatitis. Denture hygiene is essential and yet it is often overlooked by the patient or performed improperly. It is imperative for dentists as professional care-givers to instruct and assure patients understand the relevance and importance. Critical review of the literature on protocols and procedures to indicate the importance of denture hygiene and clinically showing the effects of lack of denture care. A literature search through Google, PubMed and Google Scholar focusing on publications in English dealing with denture hygiene and denture disinfection process and on the protocols used.
Protocols for denture disinfections were read of relevant articles. The results of different denture disinfection techniques were discussed including manual techniques, chemical techniques, microwaving techniques and a combination of different techniques were assessed. It is imperative for dentists as professional care-givers to take the time to instruct the patient on proper denture disinfection procedures and the importance of cleaning the dentures at least once daily well.
Keywords
Dentures, Denture stomatitis, Denture hygiene, Mechanical denture hygiene, Chemical denture hygiene, Microwave denture hygiene
Introduction
Denture hygiene and denture removal prior to sleeping is beneficial to the patient by preventing DS and allowing the tissue to a state of homeostasis. Between 2000 and 2010, the population 65 and older grew 15.1 percent, while the total U.S. population grew 9.7 percent. The opposite happened between 1990 and 2000 when the growth of the older population was slower than the growth of the total population, with growth rates of 12.0 percent and 13.2 percent, respectively. According to the American College of Prosthodontics website, “About 15 percent of the edentulous population has dentures made each year.” More than 36 million Americans do not have any teeth and 120 million people in the U.S. are missing at least one tooth [1]. These numbers are expected to grow in the next two decades. According to the Center for Disease Control and prevention (CDC) website, “Nearly 1 in 5 of adults aged 65 or older have lost all of their teeth. Complete tooth loss is twice as prevalent among adults aged 75 and older (26%) compared with adults aged 65-74 (13%).” There are many edentulous people in need of dentures.
Literature Review
The wear of dentures carries with it the possibility of an inflammatory response by the denture-bearing tissues. Denture Stomatitis (DS) is a chronic inflammation localized to the denture-bearing mucosa (the basal seat) [2]. DS may also be generalized in nature clinically, the tissue covered by the appliance, especially one made of acrylic, is erythematous and smooth or granular. It can have petechial hemorrhage. The exact cause of denture stomatitis is controversial and may even be multi-factorial. The predominant belief is that Candida albicans is strongly associated. “Although C. albicans is often associated with this condition, biopsy specimen of denture stomatitis seldom show Candida hyphae actually penetrating the keratin layer of the host epithelium [3]. It is rarely asymptomic, often accompanied by a burning sensation, is associated with pain, and is often seen in the maxilla. This could result from an illfitting mandibular denture that will not lend itself to patient use (Figures 1-6).
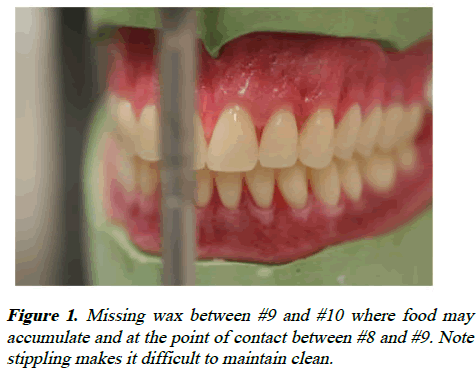
Figure 1: Missing wax between #9 and #10 where food may accumulate and at the point of contact between #8 and #9. Note stippling makes it difficult to maintain clean.
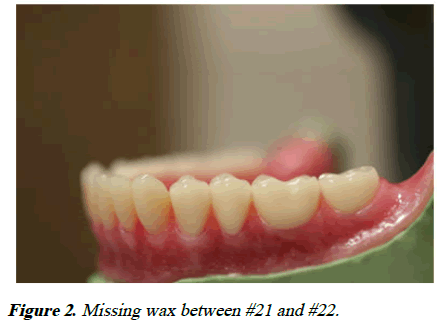
Figure 2: Missing wax between #21 and #22.
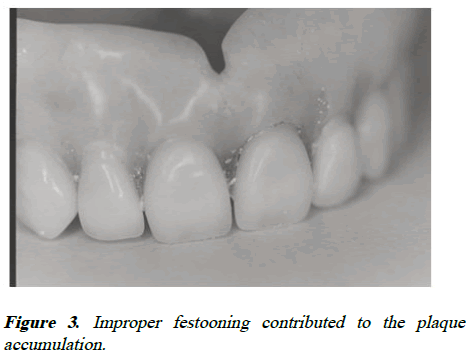
Figure 3: Improper festooning contributed to the plaque accumulation.
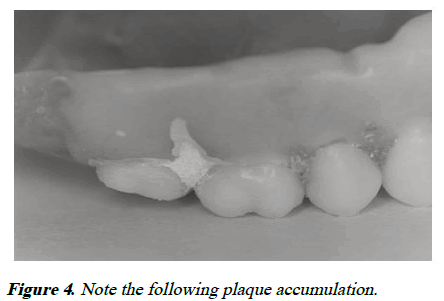
Figure 4: Note the following plaque accumulation.
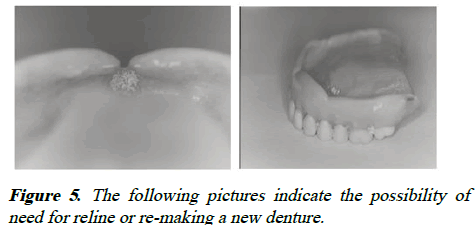
Figure 5: The following pictures indicate the possibility of need for reline or re-making a new denture.
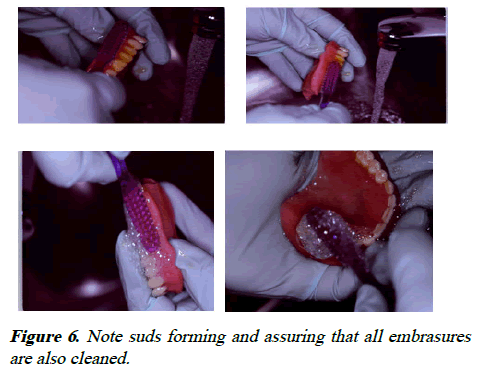
Figure 6: Note suds forming and assuring that all embrasures are also cleaned.
Discussion
Patient treatment is determined by the cause of the problem. Treatment include evaluation of systemic health (i.e., diabetes mellitus), assure proper fit of the prosthetic appliance (considerations such as reline, rebase, fabrication of new dentures and prosthetic design), improving hygiene of the appliance, control of the fungal infection (such as amphotericin, nystatin or miconazole), artificial saliva and cessation of smoking [4]. There may be cases that do not respond to these methods of treatments and a biopsy is indicated along with topical steroid therapy to rule out mucositis (an allergic reaction to denture material).
Candida-associated DS has been associated with a lack of denture hygiene. There are different methods to assist the patient with hygiene. Over-the-counter disinfection tablets in water basin has shown to decrease the bacteria count on a denture, but does not affect the Candida albicans flora. A study by Robin and Raj reported that patients aged 60-80 primarily cleaned their dentures with a toothbrush and water. Felton, et al. determined that “Careful daily removal of the bacterial biofilm present in the oral cavity and on the dentures is of paramount importance to minimize denture stomatitis and help contribute to good oral and general health [5].” Sodium hypochlorite has been shown to be effective against different microorganisms The 0.5% sodium hypochlorite solution was the most effective and might be used to control denture biofilm. Dentures should not be soaked in sodium hypochlorite for more than 10 minutes. Repeated soaking in sodium hypochlorite may cause discoloration of the denture. da Silva determined that 1% sodium hypochlorite, 2% glutaraldehyde and 2% chlorhexidine gluconate were most effective against microorganisms followed by 100% vinegar. de Souza et al., concluded that their review “Found weak evidence in support of soaking of dentures in effervescent tablets or enzymatic solutions and that brushing with paste can remove plaque and kill microbes better than inactive treatments. It is, however, unclear which is the most effective [6].” Chlorhexidine digluconate (CHX), Cetylpyridinium Chloride (CPC) or triclosan solutions inhibit bacteria. Machado showed that chlorhexidine decreases the colonization of candida albicans. CPC, CHX and Sanguinarine (SNG) mouthwashes have been shown to be effective against Candida albicans. The results suggest that mouthrinses containing antimicrobial agents might represent an appropriate alternative to conventional antifungal drugs in the management of oral candidiasis. CHX, CPC and their combination (CHX-CPC) have inhibitory effects on Candida albicans and that rinsing with mouthwashes containing these active ingredients will prove beneficial to patients. Shay mentioned that a “more effective mechanical approach to denture cleaning is through the use of a table-top ultrasonic cleaner.” Lack of professional instruction and common knowledge by a lay person limit the ability to use ultrasonic cleaner according to Shay; however, it is recommended to clean the patients denture with an ultrasonic cleaner in an institution or an office setting [7]. Shay indicated the use of a denture brush specifically designed for denture cleaning. Felton et al. indicated that daily cleaning of dentures is effective with a non-abrasive denture cleanser. Hard bristle toothbrushes and abrasive toothpastes and cleansers have been shown in studies to abrade the acrylic allowing easier growth of bacteria and C. albicans. In the United States, the dominant manner of denture maintenance is with the utilization of an effervescent commercial denture cleansing product dissolved in water. The use of a microwave after placing the denture in an ultrasonic scaling or brushing was also recommended [8]. Although microwave disinfection is being tested, there are conflicting reports with its’ effectiveness, the power to be used and the time needed for disinfection while also preventing acrylic resin deformation. Color changes have been noted with microwave disinfection. Papadiochou concluded that effervescent tablets combined with mechanical cleaning was more effective for denture sanitation compared to mechanical cleaning alone; however, the effects on Candida albicans are conflicting. Brushing with dentifrice attained greater removal of biofilm area percentage compared with brushing with neutral pH gel soap. He also determined that alkaline peroxide, 0.5% sodium hypochlorite and CHX were also effective. Color change has also been noted [9]. “Contrary to recommendations from dental and allied professionals, many individuals wearing dentures (either partial or complete) do not remove the appliances at night and as a result, denture-bearing tissues, do not get a chance to rest or receive the benefits associated with the properties of the antibacterial agents naturally present in saliva.
As clinicians, we have a responsibility to the patient regardless of the patient’s insurance for a well-fitting, relative selfcleansing denture. Ill-fitting dentures traumatize the oral mucosa creating an irritation. It is imperative that we maximize the peripheral seal by assuring that proper preliminary and secondary impression-making techniques are followed. We have to assure that the proper Vertical Dimension of Occlusion (VDO) is determined. In addition, during the festooning, assure that the wax is convex and smooth not concave and rough. This will also prevent less problems for the patient and less headaches for the clinician [10]. Also, if a patient has manual dexterity issues, an electric toothbrush be recommended to disinfect the dentures with dentifrice.
The authors recommend reiterating multiple times during the course of treatment the instructions with the patient and assuring that they have an understanding of their responsibilities. Patients should place a towel in the sink to prevent fracturing the teeth and the acrylic base. After eating, they should brush their denture with a soft bristle toothbrush and a non-abrasive liquid soap assuring that the entire denture is cleaned. This will minimize food debris accumulation and staining [11]. Dentures should be placed in soaking tablets nightly following the manufacturer’s recommendation. After instructions are followed, they should be left to soak in a water basin overnight with clean water which is replaced daily. After removing the denture from the denture basin, it should be rinsed well to remove any chemical debris left behind. Patients should be informed that denture cleansers should only be used to clean dentures outside of the mouth [12]. Dentures should never be placed in hot water and should be stored in water when not in use due to distortion factors upon drying out.
Conclusion
It must be reinforced to patients to not wear the dentures at night to allow the tissue oxygenation and prevent the moist, hot environment Candida albicans prevail.
This will also allow the tissue to rest by avoiding unnecessary compression. It is advisable to see the patient and examine intraorally and examine the denture to help prevent a future problem.
References
- Dye B, Thornton-Evans G, Li X, Iafolla T. Dental caries and tooth loss in adults in the United States, 2011-2012. NCHS Data Brief. 2015;(197):197.
[Google Scholar] [PubMed]
- Patil S, Rao RS, Majumdar B, Anil S. Clinical appearance of oral Candida infection and therapeutic strategies. Front Microbiol. 2015;6:1391.
[Crossref] [Google Scholar] [PubMed]
- Webb BC, Thomas CJ, Whittle T. A 2‐year study of Candida‐associated denture stomatitis treatment in aged care subjects. Gerodontology. 2005;22(3):168-176.
[Crossref] [Google Scholar] [PubMed]
- Duyck J, Vandamme K, Krausch-Hofmann S, Boon L, de Keersmaecker K, Jalon E, et al. Impact of denture cleaning method and overnight storage condition on denture biofilm mass and composition: A cross-over randomized clinical trial. PloS One. 2016;11(1):0145837.
[Crossref] [Google Scholar] [PubMed]
- Roshene R, Robin P, Raj JD. A survey of denture hygiene in older patients. J Pharm Sci Res. 2015;7(10):897.
- Felton D, Cooper L, Duqum I, Minsley G, Guckes A, Haug S, et al. Evidence-based guidelines for the care and maintenance of complete dentures: A publication of the American College of Prosthodontists. J Prosthodont. 2011;20(Suppl 1):S1-S12.
[Crossref] [Google Scholar] [PubMed]
- Salles MM, Badaro MM, Arruda CN, Leite VM, Silva CH, Watanabe E, et al. Antimicrobial activity of complete denture cleanser solutions based on sodium hypochlorite and Ricinus communis-a randomized clinical study. J Appl Oral Sci. 2015;23(6):637-642.
[Crossref] [Google Scholar] [PubMed]
- Moore TC, Smith DE, Kenny GE. Sanitization of dentures by several denture hygiene methods. J Prosthet Dent. 1984;52(2):158-163.
- da Silva FC, Kimpara ET, Mancini MN, Balducci I, Jorge AO, Koga‐Ito CY. Effectiveness of six different disinfectants on removing five microbial species and effects on the topographic characteristics of acrylic resin. J Prosthodont. 2008;17(8):627-633.
[Crossref] [Google Scholar] [PubMed]
- de Souza RF, Paranhos HD, da Silva CH, Abu-Naba'a L, Fedorowicz Z, Gurgan CA. Interventions for cleaning dentures in adults. Cochrane Database Syst Rev. 2009(4):CD007395.
[Crossref] [Google Scholar] [PubMed]
- Sreenivasan PK, Mattai J, Nabi N, Xu T, Gaffar A. A simple approach to examine early oral microbial biofilm formation and the effects of treatments. Oral Microbiol Immunol. 2004;19(5):297-302.
[Crossref] [Google Scholar] [PubMed]
- Giuliana G, Pizzo G, Milici ME, Musotto GC, Giangreco R. In vitro antifungal properties of mouthrinses containing antimicrobial agents. J Periodontol. 1997;68(8):729-733.
[Crossref][Google Scholar] [PubMed]
Citation: Galvan R, et al. The significance of denture hygiene related to denture stomatitis-A review. Oral Health Dent Manage. 2024;23(3):1115.
