Indexed In
- Open J Gate
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
- Google Scholar
- SHERPA ROMEO
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2021) Volume 0, Issue 0
The Risk Factors and Associated Socio-Demographic Profile of Deep Vein Thrombosis (Dvt) Among Patients Referred For Doppler Ultrasound Imaging At Dr George Mukhari Academic Hospital
Hilary Kamombe-Zingwari*, Margaret Kisansa and Alireza Dehghan-DehnaviReceived: 19-Jan-2021 Published: 09-Feb-2021, DOI: 10.35248/2329-6925.21.s4.001
Abstract
Background: Venous Thromboembolism (VTE) is one of the leading causes of cardiovascular related deaths and is a significant economic burden on the healthcare system. Early identification and correct management of patients at risk of developing DVT improves their health.
Objectives: The study sought to determine the risk factors and socio-demographic profiles of Deep Vein Thrombosis (DVT) of patients referred for Doppler ultrasound imaging at Dr George Mukhari Academic Hospital (DGMAH).
Methods: A cross sectional descriptive study was used to determine the risk factors and associated demographic profiles of DVT among patients referred for Doppler ultrasound imaging at DGMAH. The study used quantitative methods. A total of 135 patients participated. Patients completed a structured questionnaire to assess risk factors of DVT. They were then assessed for DVT using an ultrasound scan and results were documented. The information from the questionnaires and results was coded and entered into a computer using Statistical Package for Social Science (SPSS) Version 25. Data analysis was then conducted.
Results: Of the 135 patients who were referred to the radiology department for ultrasound scanning of lower limbs between January and June 2019, 42 patients (31%) were diagnosed with DVT. Prolonged bed rest (p=0.037) and history of having recently completed TB treatment (p=0.042) were associated with development of DVT.
Conclusion: Prolonged immobility and recent completion of TB treatment were associated with increased risk of developing DVT. There is need to screen these patients for DVT early and institute DVT protocols.
Keywords
DVT; Risk factors; Dr George Mukhari Academic hospital; Thrombosis; Prophylaxis
Introduction
Venous Thromboembolism is the third leading cause of cardiovascular related deaths and is a significant economic burden on the healthcare system [1] Venous thromboembolism although preventable, still causes significant morbidity and mortality among hospitalized patients [2]. Early identification and correct management of patients at risk of developing deep vein thrombosis improves their health.
The study sought to determine the risk factors and sociodemographic profiles of patients diagnosed with lower limb DVT at Dr George Mukhari Academic Hospital (DGMAH). The results of the study would be used to identify patients at risk of developing DVT and initiate prophylaxis before they develop the condition. The study would add to the body of knowledge on the risk factors for developing DVT in the South African context.
VTE comprises DVT and Pulmonary Embolism (PE). Deep vein thrombosis refers to the formation of thrombi within the venous system of the lower limbs, whereas PE occurs when a thrombus dislodges and partially or completely blocks a pulmonary artery or one of its branches. PE is a life threatening complication of DVT [3].
The prevalence of VTE varies between countries. In the USA, Europe and Asia, the prevalence of VTE was found to range from 0.2 to 0.66%, with lower rates in Asia compared to Western countries [4]. This changed in 2011 when the prevalence of DVT suddenly increased to 2.20% in Japan Tsunami flooded shelters [5]. This was attributed to dehydration and restricted mobility in crowded shelters.
Although there is limited information on DVT prevalence in Africa, a systemic review by Danwang et al. [6] showed a higher prevalence of DVT among post-operative patients, varying from 2.4% to 9.6%. A study done in a teaching hospital in Lusaka, Zambia showed a very high prevalence of lower limb DVT of 11% among HIV positive patients [7]. In South Africa, an estimated 2,00,000 people develop DVT annually and thromboembolic disease is responsible for 20,000 deaths per annum [8]. Dr George Mukhari Academic Hospital has protocols on the use of prophylaxis for DVT to reduce incidence of the disease among hospitalised patients. The use of prophylaxis in hospitalised patients reduces the incidence of DVT [9].
Virchow’s triad describes three factors that contribute to thrombosis, and these are; venous stasis, endothelial injury and hypercoagulability [10]. These should be targeted when considering the prevention of deep vein thrombosis.
In hypercoagulability, the changes in blood coagulation pathways increases the risk of coagulation [11]. Hypercoagulable instances can be due to hereditary factors such as Factor V Leiden, Protein C and S deficiency and acquired factors such as cancer, oral contraceptives, hormone replacement therapy, inflammatory bowel disease, HIV, nephrotic syndrome and pregnancy [12].
Normal endothelium is antithrombotic while endothelium injury triggers clot formation [11]. The risk of post-operative DVT is higher than preoperative, both in the injured and uninjured limbs in patients with hip fractures [13]. This is secondary to blood loss and vessel injury during surgery.
Venous stasis can occur due to immobility, congestive cardiac failure and polycythaemia [10]. Prolonged immobility was a risk factor for DVT in HIV positive patients attending out patients department at Mulago hospital in Uganda [14]. The major complications of deep vein thrombosis include pulmonary embolism, post thrombotic syndrome, recurrent DVT and treatment related complications.
Materials and Methods
We carried out a cross sectional descriptive study. The study used quantitative methods to assess the association between named risk factors and DVT among patients referred for Doppler ultrasound imaging.
The study assessed patients referred for Doppler ultrasound imaging at DGMAH for a period of 6 months.
Inclusion criteria
All patients aged ≥ 18 years and those below 18 years with consent, referred for Doppler ultrasound imaging were included in the study.
Exclusion criteria
Patients currently diagnosed with DVT and below 18 years, without consent, were excluded from the study.
Sample size was calculated using a Pearson Chi square test based on the information that an average of 20 patients is referred for ultrasound every month. Prediction based on medium effect size of 0.3 [15] and power of 0.8 [16] with degrees of freedom of 3, an adequate sample size was 122.
All patients referred for Doppler ultrasound imaging during the study period were given a detailed explanation on the purpose of the study. They were given a consent form to sign. Ethical clearance to perform the study was obtained from Sefako Makgatho University Research Ethics Committee (SMUREC). A structured questionnaire to assess risk factors of DVT, which included demographic data and DVT risk factors, was then administered.
The patient was then examined for DVT using the protocol below.
Ultrasound protocol
• A Philips Ultrasound machine EPIQ5G was used for the study. Linear probe: 5-10 MHz and Curvilinear probe: 3-5MHz was also used.
• Gray scale, colour Doppler and phasic flow were demonstrated.
• All patients were examined in supine position.
Procedure: Starting at the common femoral vein, direct visualisation of the vein for hyperechoic material and graded compression was done. Graded compression was done by applying pressure perpendicular to vessel. In the absence of a thrombus the vessel was compressed to a white thin line. Colour Doppler was used to demonstrate flow and spectral Doppler changes.
A convex probe was used to interrogate the pelvis. Colour Doppler and phasic flow were used to evaluate external iliac veins and Inferior Vena Cava (IVC).
Information from the questionnaires was entered into a computer using Statistical Package for Social Science Version 25. All the inferential statistics were conducted at 95% confidence interval with a p< 0.05.
Results
Biographic profile of the respondents
Gender: Most participants were females, who constituted 76% (n=103) and 24% (n=32) were males as shown in Figure 1.
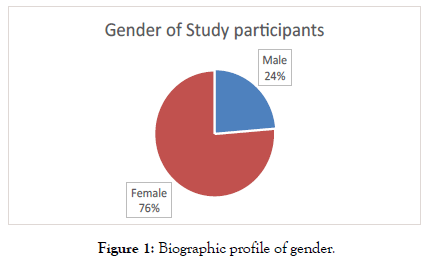
Figure 1: Biographic profile of gender.
Age: The ages of the study participants are as shown below. More than 50% of the participants were below 50 years (Figure 2).
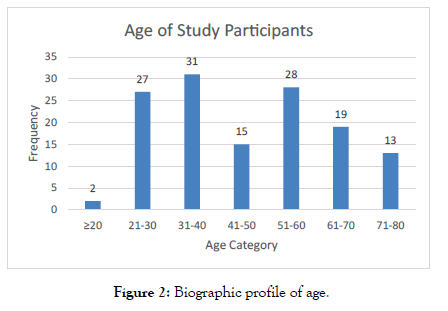
Figure 2: Biographic profile of age.
Descriptive statistics of current medical history
Twenty-four (18.3%) patients were bedridden for more than three days. Nine patients (6.9%) had undergone surgery within four weeks prior to the study. Majority of patients did not have recent paralysis or plaster immobilisation of the lower extremities.
There were 40 HIV positive patients (30.5%), while 91 patients (69.5%) were HIV negative.
Seven (5.3%) patients were diagnosed with TB at the time of the study and six patients (4.7%) had just completed TB treatment. Most of the patients (87%) had no history of cancer as shown in Figure 3.
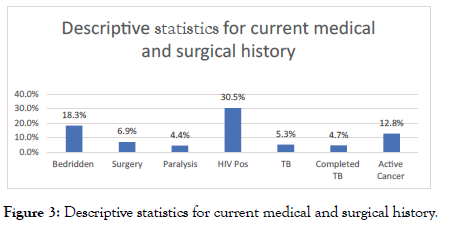
Figure 3: Descriptive statistics for current medical and surgical history.
Assessment of the current obstetric, drug and social history showed that few patients were smokers n=10 (7.5%), on oral contraceptives n=5 (5%) and on hormone replacement therapy (n=5) 3.8%. Obesity was defined as a waist circumference of more than 102 cm in males and more than 88 cm in females. Only n=39 (30.5%) of the patients were obese. Few patients n=16 (16.5%) were pregnant. A total of 6.3% (n=6) patients had delivered within the previous 6 weeks as shown in Figures 4 and 5.
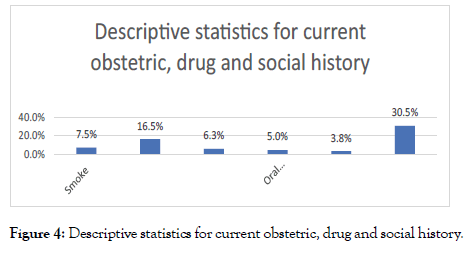
Figure 4: Descriptive statistics for current obstetric, drug and social history.
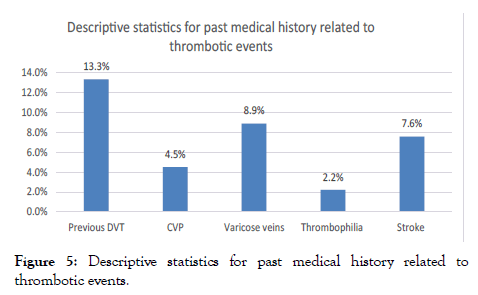
Figure 5: Descriptive statistics for past medical history related to thrombotic events.
Descriptive statistics for past medical history
A total of 18 (13.3%) patients had a previous history of DVT and 6 (4,5%) of the 133 patients had a history of having a central venous line inserted in the limb where DVT was being investigated.
Few patients n=12 (8.9%) had a history of varicose veins. Only three patients (2.2%) had a history of clotting disorders (thrombophilia) and n=10 (7.6%) had history of heart attack or stroke.
The association between current history and DVT diagnosis
Statistical analysis of the results indicated that being bedridden for more than 3 days was associated with the development of DVT (χ2=4.341, df=1, p=0.037). There was significant association between patients who had completed TB treatment within the previous three months with development of DVT (χ2=4.155, df=1, p=0.042). There was no significant association between pregnancy and development of DVT (p=0.157) and patients on oral contraceptives with DVT diagnosis (p=0.474) (Table 1).
| Factor | Developed DVT (n)% |
No DVT (n)% | P-value |
|---|---|---|---|
| Bedridden more than 3 days | 12(50%) | 12(50%) | 0.037 |
| Recent surgery within 4 weeks | 1(11%) | 8(88%) | 0.176 |
| Paralysis/recent plaster of lower extremity) | 2(33%) | 4(66%) | 0.925 |
| HIV positive | 17(43%) | 23(57%) | 0.053 |
| Patients currently diagnosed with TB | 4(57%) | 3(43%) | 0.12 |
| Recently completed TB treatment within 3 months | 4(67%) | 2(33%) | 0.042 |
| Active cancer | 5(29%) | 12(71%) | 0.857 |
| Pregnancy | 2(12.5%) | 14(87.5%) | 0.157 |
| Postpartum | 2(34%) | 4(66%) | 0.737 |
| Oral contraceptives | 2(40%) | 3(60%) | 0.474 |
Table 1: Association between current history and DVT diagnosis.
Past medical history
There was no statistically significant association between previous episodes of deep vein thrombosis and DVT (χ2=1.595, p=0.207). There was no association with history of CVP in affected limb and DVT (χ2=3.457, p=0.63).
Table 2 shows no statistical significant association between history of varicose veins and DVT (χ2=1.358, p=0.244). There was no significant association between history of clotting disorders (thrombophilia) and DVT (χ2=1.417, p=0.234). There was no significant statistical relationship between patients with history of heart disease and DVT (χ2=0.26, p=0.871).
| Factor | Total number (n) | Current DVT in the study | P-value | |
|---|---|---|---|---|
| Diagnosed with DVT(n)% | Not diagnosed with DVT(n)% | |||
| 1.Previous episodes of DVT | 18 | 8(44%) | 10(56%) | 1.595 |
| 2.History of CVP in affected limb | 6 | 4(67%) | 2(34%) | 0.063 |
| 3.History of varicose veins | 12 | 2(17%) | 10(83%) | 1.358 |
| 4.History of clotting disorders | 3 | 0 | 3(100%) | 0.234 |
| 5.History of heart disease/heart attack/stroke | 10 | 3(30%) | 7(70%) | 0.871 |
Table 2: Association between past medical history and diagnosis.
Eighteen (18) variables were evaluated and two showed a significant relationship with DVT. These were immobilisation for more than 3 days and recently completed TB treatment within 3 months. Their statistical power ranged from 0.0325 to 0.0414.
Discussion
A total of 135 patients referred to radiology department for Doppler ultrasound imaging of the lower limbs between January and June 2019 participated in the study. Of these, 42 (31%) were diagnosed with DVT. The results showed that there was a significant association between: prolonged bedrest (patients bedridden for more than 3 days), recently completed TB treatment and development of DVT.
Immobility
This study demonstrated a strong association between patients bedridden for more than 3 days and development of DVT (p value=0.037). Similar results were observed in the study by Vululi et al. [14] at Mulago hospital in Uganda, which demonstrated that prolonged immobility was a risk factor for DVT among HIV positive patients attending out-patients department. Similar results were observed in a study at a teaching hospital in Zambia where DVT was associated with prolonged hospital stay of more than 7 days [7].
Tuberculosis (TB)
This study also demonstrated a statistically significant relationship between patients who had recently completed TB treatment with DVT (p value=0.042). Four of the six patients who completed TB treatment developed DVT within 3 months of completing their treatment. A study done at a teaching hospital in Lusaka, Zambia by Mwandama et al. [7] showed a similar association between TB and DVT among admitted medical patients. Similar results were also observed in a Johannesburg hospital where TB and HIV were associated with DVT [17].
According to Gupta et al. [18] the mechanism responsible for development of DVT in TB patients is unclear. However hypercoagulability, venous stasis, and endothelial dysfunction may play a role in pathogenesis of the disease. In patients with TB, hypercoagulability could be due to increased plasma fibrinogen and factor VIII, leading to reactive thrombocytosis [18].
HIV infection
In our study, 17 out of 40 (43%) HIV positive patients developed DVT compared to 23 out of 90 (25.6%) HIV negative patients who developed DVT. There was no statistical significance (p value of 0.053) between HIV and DVT in this study. This contrasts with other studies in South Africa, Zambia and Uganda which showed association between HIV and DVT [7,14,17]. The study by Goldstein and Wu [17] in South Africa represents a cohort of patients seen in 2013, while the one by Mwandama et al. [7] in Zambia was conducted in 2016. The current study at DGMAH was conducted in 2019 at a time when South Africa had significantly improved roll out of anti-retroviral therapy (ART) programme among HIV positive patients.
South Africa had an estimated 7.7 million people living with HIV [19]. It had the largest ART programme in the world, with an estimated 4.8 million people accessing anti-retroviral therapy [19]. ART reduces opportunistic infections [20]. HIV patients with low CD4 cell count are at high risk of developing opportunistic infections and hospitalisation [14].
Although the proportion of HIV positive patients developing DVT was higher in the study compared to HIV negative patients, ART roll out could be contributing to the reduced risk of HIV positive patients developing DVT. A study by Arildsen et al. [21] demonstrated that anti-retroviral treatment (ART) improves markers of endothelial injury and coagulation.
Pregnancy
In our study, there was no statistical significance between pregnancy and DVT (p value of 0.157). This could be due to fewer pregnant patients diagnosed with DVT in our study. A metaanalysis done by Meng et al. [22] showed increased incidence of venous thromboembolism among pregnant patients and during puerperium.
Recent surgery
Patients undergoing surgical procedures are bedridden postsurgery, increasing the risk of DVT. A study by Zhang et al. [13] showed an increase in postoperative DVT in patients with bilateral hip fractures. Interestingly, only 1 of the 9 patients referred for ultrasound imaging in this study had developed DVT within 4 weeks of surgery. This could point towards improved management of patients post-surgery, with early ambulation, physiotherapy and prophylaxis to prevent DVT. A study by Wang and Ryan [2] demonstrated that the use of pharmacological and mechanical prophylaxis prevented venous thromboembolism in postoperative patients.
Oral contraceptives
In our study, there was no statistical significance between patients taking oral contraceptives and DVT (p=0.474). This could be due to few patients being on oral contraceptives in our study.
Limitation of the Study
In our study there were 135 participants. As a result of the small size of participants, our results could not be extrapolated to the population of the hospital. This could have been an inaccurate reflection of thrombosis at a tertiary hospital.
This study focused on risk factors in patients with lower limb DVT and excluded patients with upper limb DVT. Patients in Intensive Care Unit (ICU), from whom consent could not be obtained were also excluded from the study.
Ultrasound imaging has its limitations as it is not the gold standard for diagnosis of DVT. In a few obese patients it was difficult to visualise veins, and in such patients contrast venography was used to diagnose DVT. These patients were also excluded from the study.
Conclusion
Prolonged immobility and recent completion of TB treatment were associated with increased risk of DVT. There is need to screen these patients for DVT early and actively institute DVT protocols in such patients to reduce their risk of developing DVT.
Recommendations
a) ICU patients were excluded from the study due to difficulties in getting consent. We recommend empirical prophylaxis if there are no contraindications.
b) In our study, few patients were referred for DVT post-surgery. A study to assess management practices to prevent DVT in postsurgical patients is recommended.
c) TB patients should be monitored for DVT as they are at risk of developing it.
REFERENCES
- Lin J, Lingohr-Smith M, Kwong WJ. Incremental health care resource utilization and economic burden of Venous thromboembolism recurrence from a U.S. payer perspective. J Manag Care Pharm. 2020:20(2):174-186.
- Wang T-F, Wong CA, Milligan PE, Thoelke MS, Woeltje KF. Risk factors for inpatient venous thromboembolism despite thromboprophylaxis. Thromb Res. 2018;133(1):25-29.
- Stone J, Hangge P, Albadawi H, Wallace A, Shamoun F, Knuttien MG, et al. Deep vein thrombosis: Pathogenesis, diagnosis, and medical management. Cardiovasc Diagn Ther. 2017;7:S276-S284.
- Liu X, Phatak H, Dillon R, Mitchell SA. Epidemiology and mortality of venous thromboembolism across patient populations: A systematic literature review. Value Heal. 2013;16(3):A272.
- Ueda S, Hanzawa K, Shibata M, Suzuki S. High prevalence of DVT in tsunami-flooded shelters high prevalence of deep vein thrombosis in tsunami-flooded shelters established after the Great East-Japan earthquake. Tohoku J Exp Med. 2012;227(3):199-202.
- Danwang C, Temgoua MN, Agbor VN, Tankeu AT, Noubiap JJ. Epidemiology of venous thromboembolism in Africa: a systematic review. J Thromb Haemost. 2017;15(9):1770-1781.
- Mwandama CK, Andrews B, Lakhi S. Prevalence of deep vein thrombosis and associated factors in adult medical patients admitted to the University Teaching Hospital, Lusaka, Zambia. Med J Zambia. 2016;43(4):224-230.
- Awolesi D, Naidoo M, Cassimijee MH. The profile and frequency of known risk factors or comorbidities for deep vein thrombosis in an urban district hospital in KwaZulu-Natal. South Afr J HIV Med. 2016;17(1):425.
- Halim TA, Chhabra HS, Arora M, Kumar S. Pharmacological prophylaxis for deep vein thrombosis in acute spinal cord injury: an Indian perspective. Spinal Cord. 2014;52:547-550.
- Bauer K, Lip G. Overview of the causes of venous thrombosis. Uptodate. 2013:1-44.
- Wong E, Chaudhry S. Venous thromboembolism (VTE). McMaster Pathophysiology Review. 2011.
- Rybstein MD, Desancho MT. Hypercoagulable states and thrombophilias: Risks relating to recurrent venous thromboembolism. Semin Intervent Radiol. 2018;35(2):99-104.
- Zhang B-F, Wei X, Huang H, Wang P-F, Liu P, Qu S-W, et al. Deep vein thrombosis in bilateral lower extremities after hip fracture: A retrospective study of 463 patients. Clin Interv Aging. 2018;13:681-689.
- Tsongo Vululi S, Bugeza S, Zeridah M, Ddungu H, Openy AB, Frank M, et al. Prevalence of lower limb deep venous thrombosis among adult HIV positive patients attending an outpatient clinic at Mulago Hospital. AIDS Res Ther. 2018;15:3.
- Sullivan G, Feinn R. Using effect size-or why the p value is not enough. J Grad Med Educ. 2012;4(3):279-282.
- Becker LA. Effect Size (ES). 2000.
- Goldstein LN, Wu M-T. A one year audit of patients with venous thromboembolism presenting to a tertiary hospital in Johannesburg, South Africa. African J Emerg Med. 2018;8:12-15.
- Gupta A, Mrigpuri P, Faye A, Bandyopadhyay D, Singla R. Pulmonary tuberculosis-An emerging risk factor for venous thromboembolism: A case series and review of literature. Lung India. 2017;34(1):65-69.
- UNAIDS. South Africa. 2018.
- Lundgren JD, Borges AH, Neaton JD. Serious non-AIDS conditions in HIV: Benefit of Early ART. Curr HIV/AIDS Rep. 2018;15(2):162-171.
- Arildsen H, Sørensen KE, Ingerslev JM, Østergaard LJ, Laursen AL. Endothelial dysfunction, increased inflammation, and activated coagulation in HIV-infected patients improve after initiation of highly active antiretroviral therapy. HIV Med. 2013;14(1):1-9.
- Meng K, Hu X, Peng X, Zhang Z. Incidence of venous thromboembolism during pregnancy and the puerperium: A systematic review and meta-analysis. J Matern Neonatal Med. 2015;28(3):245-53.
Citation: Kamombe-Zingwari H, Kisansa M, Dehghan-Dehnavi A (2021) The Risk Factors and Associated Socio-Demographic Profile of Deep Vein Thrombosis (Dvt) Among Patients Referred For Doppler Ultrasound Imaging At Dr George Mukhari Academic Hospital. J Vasc Med Surg. S4: 001.
Copyright: © 2021 Kamombe-Zingwari H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

