Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- The Global Impact Factor (GIF)
- China National Knowledge Infrastructure (CNKI)
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2023) Volume 14, Issue 2
The Research on Compliance with ARV Treatment, Related Factors of Noncompliance with ARV in HIV Patients, and Assessment of Intervention Results by Communication at the Thot Not District In 2021
Duong Phuc Lam1* and Pham Tri Hung22Department of Medical Sciences, Thot Not District Health Center, Can Tho, Vietnam
Received: 12-Jan-2023, Manuscript No. PAA-23-19573; Editor assigned: 16-Jan-2023, Pre QC No. PAA-23-19573(PQ); Reviewed: 30-Jan-2023, QC No. PAA-23-19573; Revised: 06-Feb-2023, Manuscript No. PAA-23-19573(R); Published: 13-Feb-2023, DOI: 10.35248/2153-2435.23.14.724
Abstract
Background: Antiretroviral therapy adherence is a critical factor in antiretroviral therapy. Antiretroviral therapy is a lifelong treatment, so it is difficult to adhere to treatment. It is essential to identify factors that lead to non-adherence to treatment in order to communicate interventions to improve adherence.
Research objectives: Determine the percentage of HIV-infected patients who adhere to ART; comprehend the factors associated with HIV-infected patients not adhering to treatment; and participate in media interventions on HIV-infected people who do not adhere to treatment at Thot Not General Hospital in 2020-2021.
Subjects and methods: A cross-sectional descriptive study without a control group on 333 HIV-infected patients on ART at Thot Not District General Hospital.
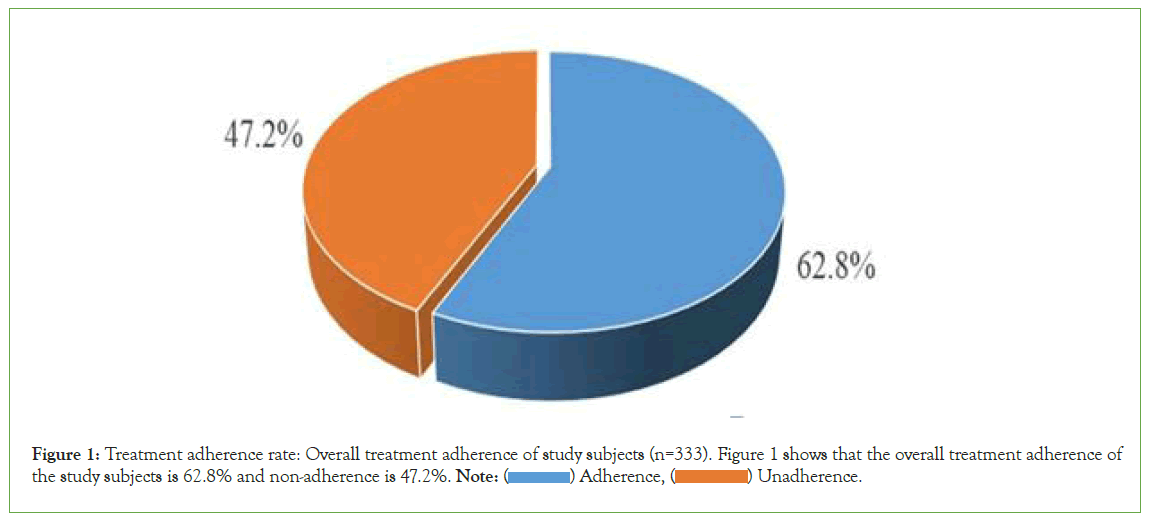
Results: 62.8% of HIV-infected patients adhered to antiretroviral therapy. Follow-up compliance on time was 79.3%; taking the full dose was 77.5%; on time, 74.5%; correctly, 77.5%; and correctly, 92.5%. There is a relationship between non-adherence to treatment and marital status, gender, and personal income. After the intervention, the adherence rate increased to 81.7%. In which 91% of patients had an on-time follow-up examination, 89.5% took the full dose, 87.4% were on time, 95.2% used the correct method, and 97.9% took the correct medication
Conclusion: The rate of HIV-infected patients who adhere to ARV treatment is 62.8%. There is a relationship between non-adherence to treatment and marital status, gender, personal income. The effectiveness of the intervention is 30% (p<0.001).
Keywords
ARV; Virus; Antiretroviral drugs; Infection; Treatment
Abbreviations
AIDS: Acquired Immunodeficiency Syndrome; ARV: Antiretroviral; CDC: Centers for Disease Control and Prevention; HAART: Highly Active Antiretroviral Therapy; HIV: Human Immunodeficiency Virus; MAC: Mycobacterium Avium Complex; NNRTI: Non-Nucleoside Reverse Transcriptase Inhibitors; NRTI: Nucleoside Reverse Transcriptase Inhibitors; PCP: Pneumocystis Pneumonia; PI: Protease Inhibitors; RT: Reverse Transcriptase; UNAIDS: The Joint United Nations Programme on HIV and AIDS; USAID: United States Agency for International Development; WHO: World Health Organization.
Introduction
Antiretroviral treatment not only reduces mortality and morbidity among people living with HIV but also reduces new HIV infections in the community. Patient compliance is very important, because adherence to treatment has many benefits for patients, such as preventing opportunistic infections, reducing virus levels in the blood, slowing the progression of the disease, and reducing the rate of infection death [1,2]. So we conducted a study on the topic. “Study on Adherence to ART, Related Factors, and Evaluation of Outcomes of Communication Interventions on HIV-Infected People” was conducted in the Thot Not district in 2020-2021 with the following goals:
1. Determine the rate of adherence to ART among HIV-infected people on treatment in the Thot Not district in 2020-2021.
2. Find out some factors related to non-adherence to treatment in HIV-infected people on treatment in the Thot Not district in 2020-2021.
3. Evaluation of the results of communication interventions on non-adherent HIV-infected people on ART in the Thot Not district in 2020-2021.
Materials and Methods
Research subjects
HIV patients receiving outpatient ART at Thot Not District General Hospital from March 2020 to March 2021
Research methods study design
Cross-sectional description and non-control intervention Sample size and selection criteria: The sample size for targets 1 and 2 was calculated using the formula for estimating a population proportion.
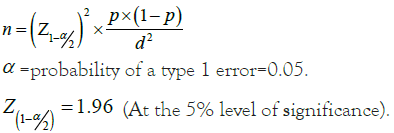
Based on Vo Thi Lot's research we chose p=0.725.
d=allowable error, set to 0.05 for n=304. Actually, there were 333 patients. The sample size for target 3 was all HIV-infected patients who did not adhere to ART.
Research content
In one year, adherence to ART is measured by taking the full dose on time, with the right drug, in the right way, having a re- examination, and receiving medication on time. Factors related to non-adherence to treatment include gender, marriage, and personal income, duration of treatment, treatment regimen, clinical stage, and distance. Evaluation of intervention outcomes through patient-guided communication to change ART adherence behavior [3].
Ethics
The study was approved by the medical ethics board of the Can Tho University of Medicine and Pharmacy and the Thot Noi District medical center. The study did not harm the health and psychology of the study participants; on the contrary, the participants also received health advice; provide knowledge and medical assistance as needed. The study does not affect the rights, reputation, or personality of the study participants. The subject has the right to refuse to participate in the research process, which is conducted only on people who are voluntary and willing to participate and keep the information confidential without information or activities contrary to the customs and ethics of the community or the individuals studied, and the results are used only for research purposes
Results
Intervention results
Compliance on re-examination and on-time medication receipt before the intervention was 79.3%; after the intervention, it increased to 91%, and the intervention efficiency was 14.7% with p<0.001. Through this content, we can see the effectiveness of counselling as well as the importance of guiding patients on how to adhere to treatment. Adherence to taking medication at the right dose before the intervention was 77.5%; after the intervention, it increased to 89.5%, and the effectiveness of the intervention reached 15% with p<0.001. Prior to the intervention, adherence to taking the correct medication was 92.5%; after the intervention, it increased by 97.9% and intervention efficiency reached 5.8% with a p-value<0.001. Medication adherence was 77.5% prior to intervention, 95.2% after intervention, and the intervention's effectiveness was 23% with a p<0.001.
As a result, during treatment and patient consultation, doctors, counsellors, and pharmacists must pay close attention to instruct patients to take the appropriate medication in conjunction with a reasonable diet and drug interactions. Prior to the intervention, 74.5% of subjects took their medications on time; after the intervention, this increased to 87.4%; the intervention's effectiveness reached 17% with a p-value<0.001.This rate increased the least in the intervention study because time compliance was the most difficult and was also affected by many factors, such as work the overall compliance rate of patients increased significantly: from 62.8% before the intervention to 81.7% after the intervention, with the intervention's effectiveness reaching 30% with a p value of 0.001. In general, non-adherence to ARV treatment in HIV-infected patients has been effectively overcome following communication intervention; however, good professional skills require medical staff to understand, sympathize, share, and have a heart in addition to knowledge and skills. We find it extremely important to regularly hold consultations, repeat them, and understand their impact on patient adherence, characteristics of ARV treatment in study subjects (Tables 1-5 and Figure 1).
| Characteristics | Frequency (n) | Ratio (%) | |
|---|---|---|---|
| Time participation ARV treatment | 6-12 months | 20 | 6,0 |
| >12 months-<2 years | 23 | 6,9 | |
| 2-3 years | 21 | 6,3 | |
| >3 years | 269 | 80,8 | |
| HIV transmission rout | Mother to son | 11 | 3,3 |
| heterosexual | 212 | 63,7 | |
| homosexual | 42 | 12,6 | |
| Blood tranfusion | 68 | 20,4 | |
| Regiem ARV teatment | Tier 1 protocol | 299 | 89,8 |
| Tier 2 protocol | 34 | 10,2 | |
Note: Table 1 shows that the majority of treatment time is over 3 years, accounting for 80.8%; the main cause of infection is homosexual contact, accounting for 76.3%; the main treatment regimen is first-line, accounting for 89.8%. |
|||
Table 1: Some characteristics of ART in study subjects (n=333).
| Adherence | Frequency (n) | Ratio (%) |
|---|---|---|
| Take enough medicine | 258 | 77,5 |
| Take medicine on time | 248 | 74,5 |
| Take the right medicine | 308 | 92,5 |
| Take medicine properly | 258 | 77,5 |
| Re-examination and receive medicine on time | 264 | 79,3 |
| Note: The majority of compliance behaviours are over 70%. | ||
Table 2: Adherence to treatment of study subjects (n=333).
| Reasons non-adherence | Frequency (n=124) | Ratio % |
|---|---|---|
| Side effect | 1 | 0,8 |
| Feel better | 3 | 2,4 |
| Taking a lot of medicine | 3 | 2,4 |
| Fear of other knowing | 39 | 31,5 |
| No means of reminding to drink | 36 | 29,0 |
| Out of medicine no time to go get it | 57 | 46,0 |
| Medical staff lack of advice | 65 | 52,4 |
| Anather reason | 67 | 54,0 |
| Note: The reasons why health workers lacked advice on compliance accounted for 52.4%; they ran out of medication and did not have time to get it, which accounted for 46%; and, in addition, other reasons also accounted for 54.0%. | ||
Table 3: Reasons for patient non-adherence (n=333).
| Characteristics | Adherence | p | OR | ||||
|---|---|---|---|---|---|---|---|
| No (n,%) | yes (n,%) | (CI 95%) | |||||
| Gender | Male | 94 | 42,3 | 128 | 57,7 | 0,006 | 1,98 (1,18-3,38) |
| Female | 30 | 27,0 | 81 | 73,0 | |||
| Marriage | Single | 71 | 42,5 | 96 | 57,5 | 0,046 | 1,57 (1,01-2,47) |
| Married | 53 | 31,9 | 113 | 68,1 | |||
| Income | low | 21 | 40,4 | 31 | 59,6 | 0,931 | 0,97(0,49-1,89) |
| Medium | 25 | 27,5 | 66 | 72,5 | 0,028 | 0,54(0,3-0,96) | |
| Rather | 78 | 41,1 | 112 | 58,9 | - | - | |
| Note: Table 4 shows that the male non-adherence rate is 1.98 times higher (CI 1.18-3.38) than the female rate (p<0.05). Single subjects have a 1.57-times higher non-adherence rate (CI 1.01-2.47) than married people (p<0.05). Higher-income people are not more likely than lower-income people to comply with treatment, but the difference is statistically significant (P 0.05). | |||||||
Table 4: Relationship between gender, marriage, income level, and non-compliance with treatment.
| Characteristics | Frequency(n) | Ratio (%) |
|---|---|---|
| Take enough medicine | 298 | 89,5 |
| Take medicine on time | 291 | 87,4 |
| Take the right medicine | 326 | 97,9 |
| Take medicine properly | 317 | 95,2 |
| Re-examination and receive medicine on time | 303 | 91,0 |
| General adherence | 272 | 81,7 |
| Note: Table 5 shows that after the intervention, most of the adherence behaviors were over 80%, of which the overall adherence increased from 62.8% to 81.7% (p<0.001). | ||
Table 5: Adherence to treatment after intervention.
Figure 1: Treatment adherence rate: Overall treatment adherence of study subjects (n=333). Figure 1 shows that the overall treatment adherence of
the study subjects is 62.8% and non-adherence is 47.2%. Note: ( ) Adherence, (
) Adherence, ( ) Unadherence.
) Unadherence.
Discussion
Adherence to ART
Adherence leads to success or failure in antiretroviral therapy [4]. Treatment adherence means taking the right medication at the right dose, at the right time, in the right way, and at the right time for follow-up visits. The use of antiretroviral drugs must last throughout life. With good cooperation and good adherence, HIV blood levels can be controlled, opportunistic infections prevented, and disease progression slowed. Mortality will decrease. Conversely, non-compliance will increase the chance that HIV will rapidly grow and produce drug-resistant strains of HIV, leading to treatment failure and an increased risk of death [5,6]. Therefore, quickly identify the causes of patient non-adherence to help them understand and practice adherence in the best way.
Compliance with the follow-up schedule and on-time medication receipt of 333 patients reached 79.3%, equivalent to the study of Duong Minh Tan at 72.57% [7]. Vo Thi Lot: 79.6% [5]. Failure to receive medication according to the schedule of follow-up visits will affect the effectiveness of treatment. Compliance with taking the right dose and taking it correctly accounted for 77.5%; taking the right medication accounted for 92.5%. In general, the medicine is dispensed according to the prescription and has an instruction sheet clearly stating the name of the drug and the dose, so the patient can review it in case she forgets the medicine or how to take it. In addition, eating right makes the drug concentration in the blood reach a high concentration, ensuring virus suppression, creating good immunity for the patient, limiting opportunistic infections and drug resistance, and avoiding the transmission of disease to others [1]. The rate of adherence to taking medication on time was 74.5%, equivalent to the study of Doan Thi Kim Phuong's 78.3% [6]. Taking medication on time is one of the most difficult principles to follow [7], requiring patients to be aware of the importance of taking medication on time and have specific solutions to avoid forgetting.
Compliance with the follow-up schedule and on-time medication receipt of 333 patients reached 79.3%, equivalent to the study of Duong Minh Tan at 72.57%, Vo Thi Lot: 79.6% [7]. Failure to receive medication according to the schedule of follow-up visits will affect the effectiveness of treatment. Compliance with taking the right dose and taking it correctly accounted for 77.5%; taking the right medication accounted for 92.5%. In general, the medicine is dispensed according to the prescription and has an instruction sheet clearly stating the name of the drug and the dose, so the patient can review it in case she forgets the medicine or how to take it. In addition, eating right makes the drug concentration in the blood reach a high concentration, ensuring virus suppression, creating good immunity for the patient, limiting opportunistic infections and drug resistance, and avoiding the transmission of disease to others. [1]. The rate of adherence to taking medication on time was 74.5%, equivalent to Doan Thi Kim Phuong's study's 78.3%. Taking medication on time is one of the most difficult principles to follow [8], requiring patients to be aware of the importance of taking medication on time and have specific solutions to avoid forgetting.
Factors associated with non-adherence to treatment
Male non-adherence to ART was 1.98 times higher than female (95% CI; 1.18-3.38) with p ≤ 0.05. Other studies have not been related to gender [5,6]. The reason for this is that men are often busy with work and travel a lot, so they often forget to take their medicine and do not follow up on time. Women may prioritize their health due to their natural motherhood and wifehood, or they may want to live a healthy life in order to care for their family and raise children. The rate of non-adherence to ART in the single group was 1.57 times higher (95% CI: 1.01-2.47) compared with the married group with p<0.05, similar to the study of Doan Thi Kim Phuong [6]. It is easy to understand that the group with spouses living together will support, share, and remind each other, resulting in better adherence to treatment than the single group [9]. Subjects with good income did not adhere to treatment 1.84 times (95% CI:1.07-3.17) compared with subjects with average income with p<0.05. Currently, people taking antiretroviral drugs who have a health insurance card will be paid insurance; they only pay when they exceed the insurance limit in one visit, so the problem of income has not been too big for them non-adherence to treatment [10].
Conclusion
The rate of adherence to ART among the 333 patients study subjects was 62.8%. The rate of adherence to taking the correct medication was the highest, at 92.5%. Factors related to treatment adherence include gender, marital status, and income level. Intervention results show a positive effect on all behaviours related to adherence to ART. Overall treatment adherence increased from 62.8% to 81.7%, and the intervention efficiency reached 30% with p<0.001.
Declaration
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the ethics committee of the Can Tho University of Medicine and Pharmacy and with the consent of the board of directors of the department of health of Can Tho City, the functional departments of the department, the board of directors of Thot Not general hospital, and all medical staff at Thot Not Medical Center. The procedures performed in this study adhered to the tenets of the declaration of Helsinki. (From pre-study protocol approval to implementation monitoring and post-study reporting). All study participants were selected when they agreed and checked the consent section of the research questionnaire and they have the right to terminate at any time during the study.
Consent for Publication
Please confirm that all authors (DPL and PTH) read and reviewed the entire content of the topic and agreed to submit the manuscript to the pharmaceutical chemistry journal for publication does not include identifying images or other personal or clinical details of participants; all information must be encrypted and kept confidential for participants.
Availability of Data and Materials
The data and documents checked by the Can Tho University of Medicine and Pharmacy meet new requirements for conducting research. The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Competing Interests
The authors declare that they haven’t any conflicts of interest.
Funding
There is no funding at all.
Author's Information
Author of the study: Duong Phuc Lam, MD, MPH, Ph.D, in public health, lecturer at Can Tho University of Medicine and Pharmacy.
Pham Tri Hung, MD, is a research associate. Deputy Director of the Thot Not District Health Center
Authors' contributions: DPL and PTH jointly produced the ideas and the study design. PTH developed the survey tools. Write a draft outline, collect data and put it into SPSS software. Write a draft of the entire research topic. DPL check and revise the research outline; process research data. Discussions and recommendations should be in writing. Both authors (DPL and PTH) read and reviewed the entire content of the topic and agreed to submit the manuscript to pharmaceutical chemistry Journal for publication.
Acknowledgement
We would like to express our gratitude and respect to patients and their families who agree to and voluntarily contribute to the research's success.
We would like to express our sincere thanks and deepest gratitude to: Ladies and gentlemen on the Board of Directors; The Ethics Committee of Can Tho University of Medicine and Pharmacy, especially Associate Professor Dr. Nguyen Trung Kien, Rector of the University, has enthusiastically helped and supported the Faculty of Public Health. Our special collaborator is Dr. Pham Tri Hung, who has provided support to complete the study.
I'd like to express my heartfelt appreciation to the board of directors of the department of Health of Can Tho City, the functional departments of the department, the board of directors of Thot Not General Hospital, and all medical staff at Thot Not Medical Center for helping me collect data to complete the research resource.
I would like to thank my colleagues, research institutions, friends, family, and relatives who encouraged and supported me throughout the research process. I sincerely appreciate everyone's good feelings and valuable help.
References
- Ministry of Health, Guidelines for HIV/AIDS diagnosis and treatment. Hanoi. 2009
- Ministry of Health, Guidelines for HIV/AIDS diagnosis and treatment. Hanoi. 2015
- Ministry of Health, Guidelines for HIV/AIDS diagnosis and treatment. Hanoi. 2017
- Nhung VT, Colby D, Khanh TH, Viet TT, Lu D, Thuy HT, et al. HIV drug resistance in children with treatment failure to first-line regimens in Ho Chi Minh City, Vietnam. J Int AIDS Soc. 2010;13(4):1.
- A specialized thesis level II in public health, conducted research on clinical, subclinical characteristics, and adherence to ARV drug treatment in HIV/AIDS-infected patients at outpatient clinics in Kien Giang province in 2018. Vo Thi Lot. 2018
- Master's Thesis in Public Health, Research on ART Adherence, Related Factors, and Evaluation of Outcomes of Communication Interventions after 1 Year in HIV-Infected People in Can Tho City in 2017-2018. Doan Thi Kim Phuong. 2018
- Specialized thesis level II health management, Research on compliance, some factors related to non-adherence to antiretroviral therapy in HIV-infected patients, and intervention results at Long Thanh District Medical Center, Dong Province, Year 2018–2019. 7. Duong Minh Tan. 2019
- Cauldbeck MB, O'Connor C, O'Connor MB, Saunders JA, Rao B, Mallesh VG, et al. Adherence to anti-retroviral therapy among HIV patients in Bangalore, India. AIDS Research and Therapy. 2009; 6:7.
[Crossref] [Google Scholar] [PubMed]
- O’Bryan GL. Factors associated with ART non-adherence and contributing influence of stock shortages at Nkongsamba Regional Hospital, Cameroon (Doctoral dissertation).
- Garcia R, Schooley RT, Badaró R. An adherence trilogy is essential for long-term HAART success. Braz J Infect Dis. 2003;7:307-314.
[Crossref] [Google Scholar] [Pubmed]
Citation: Lam DP, Hung PT (2023) The Research on Compliance with ARV Treatment, Related Factors of Noncompliance with ARV in HIV Patients, and Assessment of Intervention Results by Communication at the Thot Not District in 2021. Pharm Anal Acta.14:724.
Copyright: © 2023 Lam DP, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.