Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- Directory of Abstract Indexing for Journals
- OCLC- WorldCat
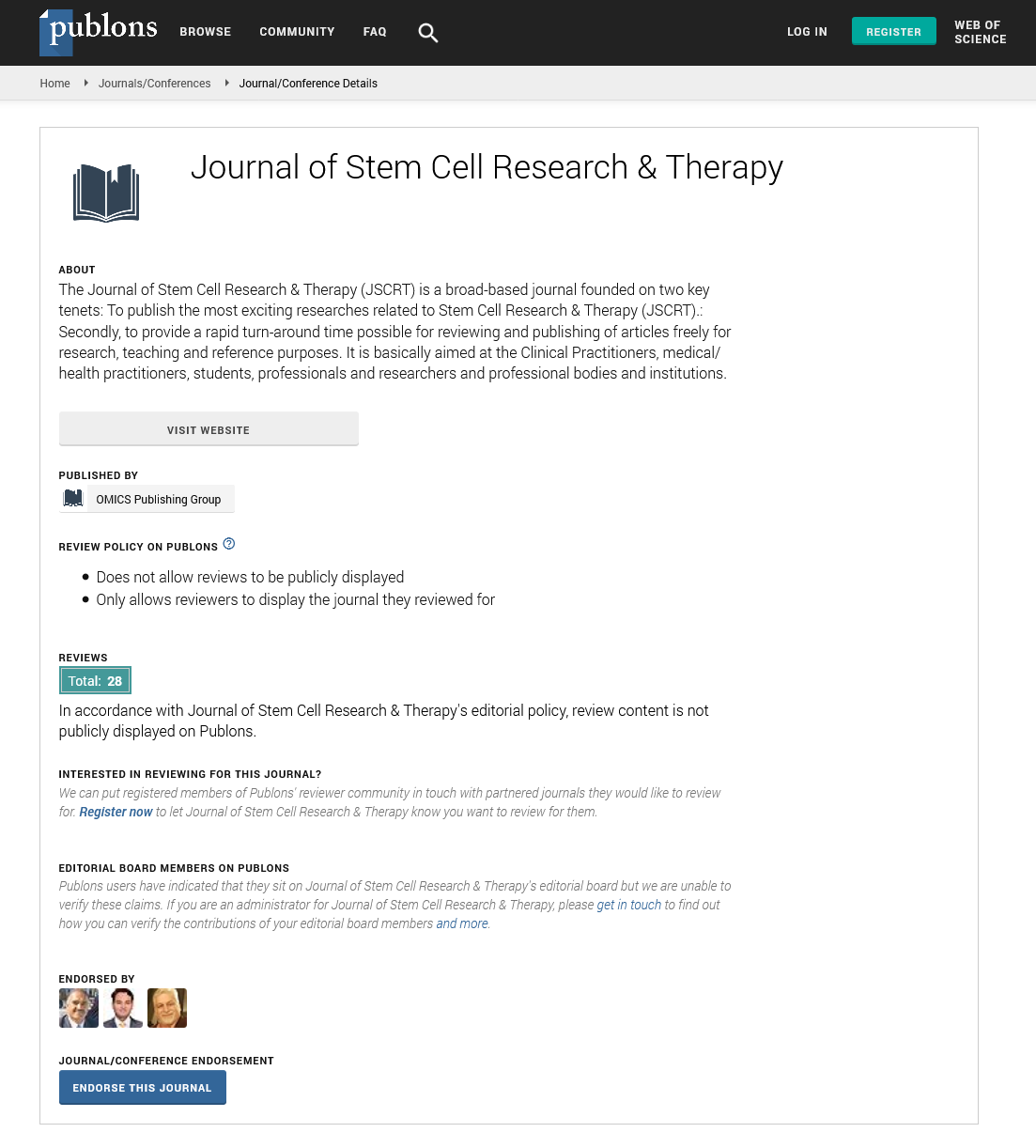
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Opinion Article - (2024) Volume 14, Issue 1
The Potential of Stem Cell-Derived Extracellular Vesicles/Exosomes for Cardiac Repair: Current Strategies and Optimization
Francesco C Martino*Received: 24-Feb-2024, Manuscript No. JSCRT-24-25325; Editor assigned: 27-Feb-2024, Pre QC No. JSCRT-24-25325 (PQ); Reviewed: 12-Mar-2024, QC No. JSCRT-24-25325; Revised: 19-Mar-2024, Manuscript No. JSCRT-24-25325 (R); Published: 26-Mar-2024, DOI: 10.35248/2157-7633.24.14.634
Description
Cardiovascular diseases remain a leading cause of mortality worldwide, urging the exploration of innovative therapeutic strategies. Stem cell therapy has emerged as a potential approach for cardiac repair due to its regenerative potential. Recently, researchers have shifted their focus towards control the therapeutic properties of Extracellular Vesicles (EVs) or exosomes derived from stem cells. These nano-sized vesicles carry a cargo of bioactive molecules, making them potential candidates for targeted cardiac repair. This article delve into the current optimized strategies for utilizing stem cell-derived EVs/ exosomes in cardiac repair.
Stem cell-derived EVs/exosomes
Exosomes and other extracellular vesicles are membrane-bound nanovesicles secreted by various cell types, including stem cells. Stem cell-derived EVs/exosomes encapsulate a diverse array of proteins, lipids, nucleic acids, and signaling molecules, functioning as mediators of intercellular communication and modulators of tissue repair processes. Their cargo includes growth factors, cytokines, microRNAs, and other regulatory molecules implicated in cardiac regeneration and repair mechanisms.
Optimized strategies for cardiac repair
Isolation and characterization:
• Precise isolation methods are important to obtain pure populations of stem cell-derived EVs/exosomes. Techniques such as ultracentrifugation, size exclusion chromatography, and immunoaffinity capture are commonly employed.
• Advanced characterization methods including nanoparticle tracking analysis, electron microscopy, and proteomic profiling enable the comprehensive analysis of EVs/exosomes, ensuring their quality and functionality.
Engineering for enhanced therapeutic efficacy:
• Researchers are exploring various strategies to enhance the therapeutic potential of stem cell-derived EVs/exosomes. These include genetic modification, surface engineering, and cargo loading techniques.
• Genetic engineering allows the overexpression or knockdown of specific cargo molecules within EVs/exosomes, optimizing their regenerative properties.
• Surface modification techniques, such as peptide or antibody conjugation, facilitate targeted delivery to injured cardiac tissues, enhancing therapeutic efficacy.
• Cargo loading approaches involve loading EVs/exosomes with specific bioactive molecules or drugs to augment their reparative capabilities.
Optimization of administration routes:
• The route of administration significantly impacts the biodistribution and therapeutic efficacy of stem cell-derived EVs/exosomes in cardiac repair.
• Intravenous injection is a commonly employed systemic delivery route, allowing widespread distribution of EVs/ exosomes throughout the myocardium.
• Intramyocardial injection offers a more localized delivery approach, directly targeting injured cardiac tissues, albeit with limited distribution.
• Inhalation and topical application routes are also being explored for non-invasive and targeted delivery to the heart.
Combination therapies:
• Combining stem cell-derived EVs/exosomes with other therapeutic modalities holds promise for synergistic effects and enhanced cardiac repair.
• Co-administration with biomaterials, such as hydrogels or scaffolds, provides a supportive microenvironment for EV/ exosome retention and sustained release, promoting tissue regeneration.
• Integration with gene therapy approaches enables the simultaneous delivery of therapeutic genes and EVs/ exosomes, offering a multifaceted strategy for cardiac repair.
Preclinical optimization and translation:
• Preclinical studies in relevant animal models are essential for evaluating the safety and efficacy of stem cell-derived EVs/ exosomes in cardiac repair.
• Optimization of dose, frequency, and timing of administration is important to maximize therapeutic outcomes while minimizing adverse effects.
• Translation of optimized strategies from preclinical models to clinical settings involves rigorous preclinical-to-clinical translational research, including pharmacokinetic studies, dose escalation trials, and safety assessments.
Stem cell-derived extracellular vesicles/exosomes represent a potential therapeutic approach for cardiac repair, offering several advantages over conventional stem cell therapies. Optimized strategies surround precise isolation and characterization, engineering for enhanced efficacy, optimization of administration routes, combination therapies, and rigorous preclinical optimization are prepare for their clinical translation. Continued research efforts aimed at refining these strategies will undoubtedly contribute to the development of effective regenerative therapies for cardiovascular diseases, ultimately improving patient outcomes and quality of life.
Citation: Martino FC (2024) The Potential of Stem Cell-Derived Extracellular Vesicles/Exosomes for Cardiac Repair: Current Strategies and Optimization. J Stem Cell Res Ther. 14:634.
Copyright: © 2024 Martino FC. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.