Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- CiteFactor
- Ulrich's Periodicals Directory
- Access to Global Online Research in Agriculture (AGORA)
- Electronic Journals Library
- Centre for Agriculture and Biosciences International (CABI)
- RefSeek
- Directory of Research Journal Indexing (DRJI)
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Scholarsteer
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Review Article - (2021) Volume 12, Issue 4
The Pharmacology and Therapeutic Value of Conventional Antihypertensive Drugs in the Management of Hypertension: An Ethno-Botanical Review of Commonly Used Antihypertensive Medicinal Plants in Arsi Zone, South-East Ethiopia
Leta Melaku*Received: 10-Apr-2021 Published: 28-Apr-2021, DOI: 10.35248/2157-7471.21.12.549
Abstract
Plants have been used to treat a wide range of diseases throughout the history of human beings and this practice continues to date. In traditional methods, plant materials are tested for pharmaceutical purposes. Natural products from plants remain vital in drug discovery where they can be used directly as drugs or serve as leads to new drugs by providing chemical entities. Hypertension (HTN) is a progressive cardiovascular disease characterized by persistently elevated systemic blood pressure. If left uncontrolled, HTN will become the major cause of human suffering as well as imposing severe economic and service burdens on health systems. Today on the market there are large armamentaria of conventional antihypertensive drugs, however, the major concerns that often delay treatment allude to higher costs, unavailability and inaccessibility, undesired side effects of antihypertensive drugs and reduced patient compliance to consume more than a pill per day. The search for natural, cheaper, and nontoxic compounds is becoming necessary. In the past, the drug discovery of the biological compounds from plant materials and the process of identifying the structures of active compounds from the extracts were problematic. In Ethiopia, the long history of using traditional medicinal plants for combating various ailments can be confirmed by referring to the medico-religious manuscripts in the country. Herbal medicines have been also commonly used and remain. Symptoms of HTN can be also resolved by herbals.
Keywords
Antihypertensive drugs; Hypertension; Medicinal plants
Introduction
Traditional medicine refers to any ancient, culturally based healthcare practice different from scientific medicine [1]. Plants have been used to treat a wide range of diseases throughout the history of human beings and this practice continues to date. This is mainly because most of these herbals are accessible, affordable and the extracted chemicals have little or no side effects compared to drugs synthesized in the laboratory [2]. Natural products from plants remain vital in drug discovery where they can be used directly as drugs or serve as leads to new drugs by providing chemical entities [3]. The approach to new drugs through natural products has proved to be the single most successful strategy for the discovery of new drugs [4]. Currently, a large number of medicinal plants have found their way as raw materials of modern biopharmaceutical industry. Besides their use in fighting various ailments at local level, different medicinal plants are used as export commodities, which generate considerable income [5].
In traditional methods, plant materials are tested for pharmaceutical purposes. If any evidence of activity is observed, the extract is fractioned, and the active compound is isolated and identified. Each step of decomposition and isolation is usually guided by biological tests, which are referred to as bioassay-guided fractionation (Figure 1) [6]. Sometimes, a direct product isolation method, regardless of bioactivity, is also used, which leads to the isolation of a number of natural compounds suitable for measuring any biological activity. However, this process can be slow and inefficient, and also does not guarantee isolation of lead compounds from screening would be in chemically successful or even recordable [7].
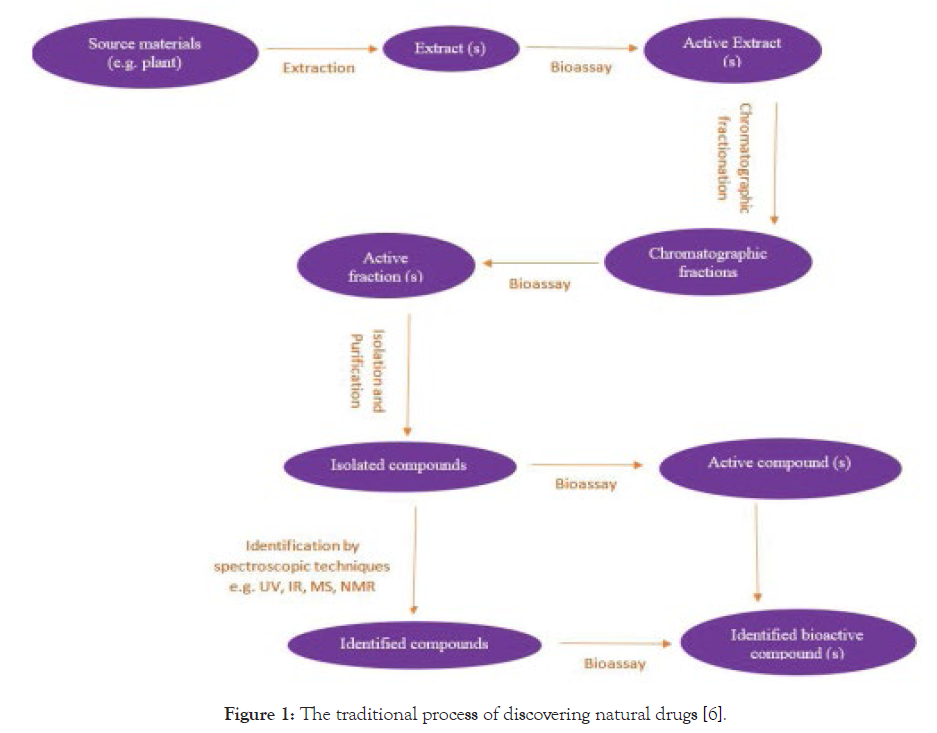
Figure 1: The traditional process of discovering natural drugs [6].
The beginning of the development of herbal medicines was concurrent with the development of chemistry and isolation, purification, and determination of plant compounds [8]. Naturally occurring compounds may be divided into two broad categories. The first class of compounds is known as primary metabolites which include nucleic acids, common amino acids, sugars, and high molecular weight polymeric materials such as cellulose, lignin and proteins which form the cellular structures. Most primary metabolites exert their biological effects within the cell or organism that is responsible for their production. The second class of compounds is secondary metabolites. Such compounds are characteristic of a limited range of species and occur in plants with high structural diversity. The major classes of secondary metabolites including tannins, glycosides, flavonoids, alkaloids, terpenoids, steroids, quinones, and saponins are among others and play a significant role in drug discovery. Secondary metabolites have often attracted the interest of researchers because of their biological effects on other organisms [9,10].
In the past, the drug discovery of the biological compounds from plant materials and the process of identifying the structures of active compounds from the extracts were problematic depending on the complexity of the compounds and might take weeks, months or even years. Nowadays, the rate of bioassay-guided fractionation has been significantly enhanced by the development of precision instruments such as high-performance liquid chromatography (HPLC/MS), liquid chromatography mass spectrometry (LC/ MS), magnetic field and nuclear magnetic resonance (NMR) is a recent major breakthrough for the categorization of compounds that are extremely limited in quantity in their organisms of origin [11]. Despite the success of research to produce medicinal plants over the past few decades, future efforts face many challenges. Standardization of raw materials is an important issue for the plant industry [12]. Herbaceous plants can be easily infected during growth, processing and collection. Contamination and pollution with heavy metals are two main problems with herbal drugs [13]. The other challenge facing medicinal plants is also the loss of medicinal plant species due to the non-principled use of these resources [6]. According to the International Union for Conservation of Nature, there are between 50,000 and 80,000 flowering plant species that are used for pharmaceutical purposes around the world. Among these numbers, about 15,000 species are exposed to a risk of extinction due to high harvesting and destruction of habitats [14] and 20% of their wildlife resources are decreasing due to growing human populations and excessive consumption of plants [15].
Literature Review
The pharmacology and therapeutic value of conventional antihypertensive drugs in the management of hypertension
Hypertension (HTN) is a progressive cardiovascular disease characterized by persistently elevated systemic blood pressure of at least SBP > 140 mmHg and/or DBP > 90 mmHg [16,17]. From a pathophysiological perspective, it is obvious that HTN is not purely an increase of blood pressure (BP) values, but a rather a sophisticated web of neurohormonal and haemodynamic interactions [18]. Depending on the underlying causes of the condition, HTN is categorized into 2 types: primary (essential) and secondary HTN. The majority (90%) of patients with HTN have ‘primary’ or ‘essential’ HTN where no identifiable underlying causes are exactly found but likely to be a consequence of a combination of both genetic and environmental factors [19,20]. The remaining minority (up to 10%) have ‘secondary’ HTN which has identifiable organic causes such as endocrine, neurologic, renal, and vascular diseases, medical conditions (i.e., obstructive sleep apnea), pregnancy, and drug-induced [21,22].
HTN is one of the most important public health problems in the world. HTN remains the leading cause of death globally, accounting for 10.4 million deaths per year [23]. By 2030, the annual death toll is estimated to reach 23.5 million people [24]. Complications of HTN also account for 9.4 million deaths worldwide. It is responsible for at least 45% of deaths due to CHF [25], 49% of deaths due to ischemic heart disease [26], and 54% of deaths due to stroke [27]. HTN is the leading preventable risk factor for premature death and disability worldwide [28]. HTN is responsible for 143 million disabilities worldwide [29,30]. HTN is also a major player in the onset of diseases such as atherosclerosis, stroke, peripheral artery disease, heart failure, and coronary artery disease, as well as it can also lead to kidney damage, dementia, or blindness [31,32]. It has been considered as the first and the most common risk factor for CKD and ESRD [33]. The association with comorbidities such as dyslipidemia, prothrombotic state, and autonomic dysfunction contributes to an increase in morbidity and mortality [34]. The risk of cataract and hypertensive retinopathy was also found to be increased in populations with HTN independent of glycaemic risk, obesity, or lipids [35]. It also increases the risk and progression of diabetic retinopathy [36]. There is evidence that raised BP inversely correlates with cognitive function and that hypertension is associated with an increased incidence of dementia [37].
According to the World Economic Forum, NCDs are not only an important public health problem in both economically developed and developing nations [38]; rather, it will also have a big economic impact as a significant proportion of the productive population becomes chronically ill and stays at home, leaves their jobs, or die, leaving their families in poverty [39,40]. The global direct medical costs of HTN are estimated at $370 billion per year, with health care savings from effective management of blood pressure projected at roughly $100 billion per year [41]. High blood pressure costs the USA about $131 billion each year, averaged over 12 years from 2003 to 2014 [42]. This total includes the cost of health care services, medications to treat HTN, and missed days of work [43]. Over the period 2011 – 2025, the cumulative lost output in LMICs associated with NCDs is projected to be US$ 7.28 trillion [44]. HTN accounts for nearly half of the cost [45]. If left uncontrolled, HTN will become a major cause of human suffering as well as imposing severe economic and service burdens on health systems.
HTN is common and readily detectable; the key factor for the prevention and control of the epidemic of HTN is the identification and treatment of its major risk factors. Today on market there are many standard antihypertensive drugs ranging from diuretics (Indapamide, Furosemide, Amiloride), sympathoplegic agents (clonidine, reserpine), renin inhibitor (Aliskiren), ACEI (Enalapril, Captopril, Quinapril), ARBs (Losartan, Irbesartan, Olmesartan), Ca2+ channel blockers (Nifedipine, Verapamil, Diltiazem), α-adrenergic blockers (Prazosin, Doxazosin), β-adrenergic blockers (Nebivolol, Atenolol) to vasodilators (Minoxidil, sodium nitroprusside), which are used to manage blood pressure levels in hypertensive patients [46-48]. The objective of antihypertensive treatment is to achieve optimal blood pressure levels during therapy to reduce HTN-related complications. However, the frequent side effects that come with the use of these synthetic antihypertensive drugs, including dry mouth, dizziness, visual disorders, headache, cough, emotional distress, gastrointestinal disturbance, peripheral circulatory symptoms like cold hands and feet, swollen ankles, are by far their biggest disadvantages [49,50]. These distressing side effects can lead to noncompliance and adversely affect healthrelated quality of life. These antihypertensive drugs also increase the risk of developing new diseases which worsen the situation and result in suboptimal control of high blood pressure [51]. Clinically, various antihypertensive drugs have been used to manage HTN and to alleviate symptoms. However, the efficacy of these drugs is only 40-60% and usually two or more antihypertensive drugs from different categories are needed to be combined to achieve the optimal results and thus, this ultimately increases the cost of treatment and side effects [52,53]. In ALLHAT, 60% of those BP was controlled to < 140/90 mmHg received two or more agents, and only 30% overall were controlled with one drug [54]. Furthermore, HTN prevalence is still increasing as a result of the awareness, control, and treatment of the disease are very weak [55]. Despite the fact that the detection of raised BP is very simple and cheap, only 34% of HTN is managed [56]. The major concerns that often delay treatment allude to higher costs [48], unavailability and inaccessibility [57], undesired side effects of antihypertensive drugs [48,56] and reduced patient compliance to consume more than a pill per day [31]. Therefore, newer antihypertensive agents are needed to expand therapeutic options, increase treatment efficacy, decrease side effects, and enhance patient adherence [57]. In addition, the search for natural, cheaper, and nontoxic compounds is becoming necessary [58-60].
Phytotherapeutic roles of commonly used medicinal plants for the management of hypertension in Arsi zone of Ethiopia
It is estimated that 70 - 80% of people worldwide rely chiefly on traditional, largely herbal medicines to meet their primary healthcare needs [61,62]. Traditional medicine plays an important role in primary health care in Ethiopia, where an estimated 80% of human illnesses and 90% of livestock diseases are being treated with plant materials, minerals, and animal products [63]. In Ethiopia, the long history of using traditional medicinal plants for combating various ailments can be confirmed by referring to the medico-religious manuscripts in the country [64]. Modern studies on traditional medicinal plants in Ethiopia started in 1973 [65]. Ever since this time, during the last four decades, considerable researchers have been doing investigations on MPs, especially on local knowledge of traditional MPs [66-71].
Although many people nowadays use herbal medicines as a constituent of primary health care, there are still many concerns about the safety and efficacy of using plants. While herbal medicines can potentially contribute to the advancement of healthcare, many major challenges need to be addressed before effective adherence of herbal medicines to traditional medicine. The lack of accurate translation and interpretation of the texts and research findings on plants by scientists around the world is one of the main challenges in this field. In fact, to realize the effective integration of plants into a medical system, researchers and practitioners should be trained in both modern and traditional medicine in the use of plant compounds. In addition, to build credibility for the use of plants in conventional medicine, the empirical arguments should be converted into evidence-based arguments. Finally, several questions about safety, accurate dose, duration of treatment, side effects, acute and chronic toxicities as well as the standardization of herbal medicines and natural products should be answered. If these issues are resolved, medicinal plants can be used as a safe, effective, and affordable form of health care [6]. Medicinal herbs have a hopeful future since there are about half a million plants around the world, most of them have not yet been studied in medical practice, and current and future studies on medical activities can be effective in treating diseases [73]. The use of medicinal plants has a long history; however, the use of the whole plant or raw materials for treatment or experimentation has many drawbacks, including changes in the plant’s compounds in different climates, simultaneous development of synergistic compounds that lead to adverse effects of antagonists, or other unexpected changes in bioactivity, and changes or loss of bioactivity due to the variability and accumulation, storage and preparation of raw materials; therefore, advancing towards the isolation of compounds and the use of pure substances with bioactivity, instead of the plant benefits, has certain benefits including convenient examination of therapeutic effects and determination of toxic doses to control the quality of the therapeutic formulation [72].
Herbal medicines have been commonly used and remain so instead of synthetic drugs because of their possible fewer side effects like weakness, tiredness, drowsiness, impotence, cold hands and feet, depression, insomnia, abnormal heartbeats, skin rash, dry mouth, dry cough, stuffy nose, headache, dizziness, swelling around eyes, constipation or diarrhea, fever or anaemia alone and associated with pressure medicines [74,75]. Symptoms of HTN like headaches, palpitations, fatigue, flushed face, blurry vision, nosebleeds, strong need to urinate, often ringing in ears, and dizziness can be resolved by herbals [76]. Herbals do not also interfere with medications including diuretics, blood thinners, β-blockers, and calcium channel blockers [77]. Many scientific studies also suggest different life style changes such as stress reduction, proper diet, regular exercise, limited salt intake, smoking cessation, limited alcohol intake, and the use of appropriate herbal medicines in the management of HTN [78,79].
The Rumex species
The Polygonaceae, commonly known as the knotwood or smartweed family, are a family of flowering plants and comprise about 1200 species containing 50 genera. Among which largest ones are Eriogonum (2410 species), Rumex (200 species), Cocoloba (120 species) and Persicaria (100 species), etc. This family is wildly distributed in North Temperature Zones although it can be found worldwide [80]. Plants belonging to the Polygonaceae are known to produce a large number of biologically important secondary metabolites, such as anthraquinones, naphthalenes, stilbenoids, steroids, flavonoid glycosides, leucoanthocyanidins and phenolic acids [81-85]. The name Rumex originated from the Latin word for dart, alluding to the shape of the leaves [86]. Roots, seeds, leaves, fresh plant juice, aerial parts, etc. are the parts generally used. Different species of Rumex genus contain various types of pharmacological activities, e.g. anti-inflammatory, antioxidant, cytotoxic, antifertility, purgative, antidiarrhoeal, antifungal, antipyretic, antiviral activities [87-92]. Traditionally, one species of Rumex genus named Rumex abyssinicus, has been also used for hypertension and pain relief. This plant also possesses antibacterial and diuretic properties [89]. Important chemical constituents of Rumex include anthraquinones, naphthalenes, tannins, flavonoids, phenolic acids, stilbenoids, triterpenes, carotenoids, etc. Rumex hymenosepalus contains Leucodelphinidin and Leucopelargonidin which are antitumorous substituents. Neopodin, a substance found in Rumex japonicas, has an inhibitory effect on osteoclasts [93]. Rumex nepalensis Spreng is another species that is widely used for various actions like antifungal, antibacterial, purgative. This species has moderate cytotoxicity and high phytotoxic activity [94]. The methanolic extract of Rumex hastatus D. Don species has many biological effects including antioxidant, antinociceptive, anti-diarrhoeal, and cytotoxic potential [95,96]. Rumex dentatus, Rumex acetosa, Rumex crispus, Rumex patientia, and Rumex obtusifolius are also some of the plants highly used for various pharmacological actions [97]. The juice of Rumex nervosus is used in Ethiopia for seizure bleeding roves to be the single most successful strategy for the discovery of new drugs [4].
Cymbopogon citratus
Cymbopogon citratus is an aromatic perennial plant of the Poacae family, with long slender green leaves. It is widely distributed and extensively used worldwide [98-101]. Several studies evaluating the phytochemical composition of C. citratus have shown the presence of saponins, tannins, anthraquinones, flavonoids, phenols, and alkaloids, in addition to terpenes, aldehydes, alcohols, and esters [102-105]. Furthermore, trace amounts of other components have been detected, including myrcene, geranial, geraniol, limonene, burneol, citronellol, nerol, α-terpineol, elemicin, catechol, luteolin, 6-C and 7-C-glycosides, caffeic acid, apigenin, luteolin, kaempferol, quercetin, chlorogenic acid, and geranyl acetate [102-105]. Fumesol, furfurol, isopulegol, isovaleranic aldehyde, L-linalool, methylheptenone, n-decyclic aldehyde, nerol, terpineone, p-coumaric acid, and valeric esters have also been isolated in some studies [102-105]. Cheel et al. [106] have reported the presence of isoscoparin, swertia japonin, and orientin in C. citratus, along with numerous other phytochemicals reported recently by Bharti et al. [107]. C. citratus also contains electrolytes and minerals (including sodium, potassium, calcium, copper, magnesium, manganese, selenium, phosphorus, iron, and zinc), vitamins (including folate, niacin, pyridoxine, riboflavin, and vitamins A, C, and E), and macronutrients (carbohydrates, proteins), and a small amount of fat [108]. Growing evidence suggests that these phytochemical components are responsible for the wide range of biological and therapeutic actions of C. citratus. The consumption of infusions and decoctions made from C. citratus has been a common practice in various countries since the discovery of the medicinal value of the plant throughout recorded history [98-100]. It is most frequently consumed for recreational and medical/therapeutic purposes [99], much like green, black, and red (rooibos) teas, herbal tea blends, and coffee. Many consumers prefer C. citratus tea to other beverages, because of its physicochemical characteristics, including taste; distinctive lemony smell, color, strength, and intensity [98], while many others consume C. citratus tea or decoction for physiological reasons [99,100]. It is used in herbal medicine for a wide range of applications based on its antibacterial [109], antifungal [110], antiprotozoal [111], anti-carcinogenic [112], anti-inflammatory [113], antioxidant [114], cardio-protective [115], antitussive, antiseptic, and anti-rheumatic activities. It has also been used to inhibit platelet aggregation [116], treat diabetes [117], dyslipidemia, gastrointestinal disturbances [118], anxiety [119], malaria [120], flu, fever, and pneumonia [102], as well as in aromatherapy. In addition to its therapeutic uses, C. citratus is also consumed as a tea, added to nonalcoholic beverages and baked food, and used as a flavoring and preservative in confections and cuisines. In cosmetics, essential oils are used as fragrances in the manufacture of perfumes, soaps, detergents, and creams [121, 122].
Cymbopogon citratus Stapf
Cymbopogon citratus Stapf. (Lemon grass) is an important medicinal and aromatic perennial tall grass having rhizomes and densely tufted fibrous roots. It belongs to the Poaceae family which is renowned as an oil rich family. Green slightly leathery leaves appear in dense clusters on short underground stems [123]. The plant is a native herb of India and is cultivated in other tropical and subtropical countries [124]. Lemongrass can tolerate a wide range of soils and climatic conditions. However, vigorous growth is obtained on well-drained sandy loam soil with high fertility and exposed to sunlight [125]. It is reported to possess antibacterial [109], antifungal [123], antiprotozoal, anti-carcinogenic, anti-inflammatory, antioxidant, cardio-protective, antitussive, anti-septic, and antirheumatic activities [102]. It has also been used to inhibit platelet aggregation [116], treat diabetes [117], dyslipidemia, gastrointestinal disturbances [123], anxiety [119], malaria [120], flu, fever, and pneumonia [102], as well as in aromatherapy. In addition to its therapeutic uses, C. citratus is also consumed as a tea, added to nonalcoholic beverages and baked food, and used as a flavoring and preservative in confections and cuisines. In cosmetics, essential oils are used as fragrances in the manufacture of perfumes, soaps, detergents, and creams [126].
Calpurnia Aurea
Calpurnia aurea is a genus of flowering plants within the family of Fabaceae. The genus comprises shrubs or small trees in or along the margin of forests in many parts of Ethiopia and widely distributed in Africa from Cape Province to Eritrea and which also occurs in Southern India [127]. Literature survey brings to light that all parts of the plant species have been used for different human and animal diseases [128]. Calpurnia aurea from Ethiopia is known locally as "digitta" (Amharic), "Hitsawits" (Tigrigna). The plant is used in traditional medicine of Ethiopia to treat diverse medical conditions. In native countries like Ethiopia, traditionally, the leaves and powdered roots of Calpurnia aurea are used for the treatment of syphilis, malaria, rabies, diabetes, lung TB, hypertension, diarrhoea, leishmaniasis, elephantiasis, fungal diseases, different swellings, stomach-ache, abscesses, bowel, bladder disorders, to induce uterine contractions [129], used as an insecticide to kill lice [130], and tapeworm, trachoma, ringworm, as well as vomiting, headache and eye diseases [131-134], to destroy maggots, to destroy bedbugs, to relieve itches, used as a fish-poison or as a cure for dysentery, exhibit activity against amoebiasis and giardiasis, cough and snake bite [128,135].
The Thymus Species
The genus ThymusL. belongs to the Lamiaceae family and consists of over 400 species of herbaceous annuals and perennial plants that are extensively used for medicinal and nonmedicinal purposes. These plants are widely distributed throughout the Old World [136,137] and have been used for many centuries in traditional medicine due to their antiseptic, carminative, antiviral, and antioxidant properties [138]. Thymusspecies are also interesting as a source of pentacyclic triterpenoids with several properties, such as anti-inflammatory, hepatoprotective, antimicrobial, anti-HIV-1 activity, antiulcer, gastroprotective, hypoglycemic, anti-hyperlipidemic activity, and specific cytotoxicity against a variety of tumor cell lines [139-141]. Furthermore, interests focusing mainly on selected chemotypes for the cosmetic and food industries, among others, lead to the loss of other species in nature, such as Thymus cariensis Hub.-Mor. & Jalas, Thymus cilicicus Boiss. & Balansa, Thymus sipyleusBoiss., Thymus pulvinatusČelak., and Thymus cherlerioides Vis [142]. These species should be preserved to make available access to a wide range of genetic diversity. On the other hand, as the plant has a low propagation rate in nature, a suitable method to obtain a high number of plants is needed [143].
Diuretics are substances that promote the production of urine and elimination of ions such as sodium from the body. Numerous studies now exist affirming the diuretic effects of traditional medicines [144]. The leaf of T. schimperi is traditionally used for urinary retention and hypertension and is reported to show diuretic activity with increased ionic content of urine in rats [145]. Moreover, there is also scientific evidence that aqueous leaf extract of T. serrulatus possesses in vitro vasodilatory activity on the thoracic aorta of Guinea pigs [146].
The Genus Ajuga
The plants in the genus Ajugaare evergreen, clump-forming, rhizomatous, annual or perennial herbaceous flowering species in the mint family, Lamiaceae. There are at least 301 species of the genus Ajugawith many variations: Ajugais one of the 266 genera of the family Lamiaceae. Ajuga integrifolia, mostly known under the name Ajuga bracteosa, is a herb often lying on the ground and rooting at the nodes, covered with soft hairs, stems growing up to 40 cm high. Its leaves are oblanceolate and coarsely toothed. Its flowers are small, pale blue, white, or pale violet found in small clusters in the leaf axils [147,148]. It is found at an altitude of 1500 to 3200 m above sea level [147-149]. In Ethiopia it grows in different regions including Bale, Gojam, Gondar, Harerge, Kefa, Shoa, Sidamo, Tigray and Wollo [149,150]. Andarge et al. [151], also reported that Ajuga integrifolia has been found abundantly (plenty) in Dawuro Zone, SNNPR, Ethiopia. Ajuga integrifolia Buch.-Ham. (Syn: Ajuga remota; Ajuga bracteosa) is known by common names: ‘Armagussa’, ‘Etse Libawit’, ‘Medhanit’ (in Amharic). Ajuga integrifolia is widely used in traditional medicine for treating; It can also be used for veterinary purposes [134,152]. A decoction of the leaves of the herb is used in traditional medicine for a number of diseases including diarrhea, stomach disorders, evil eye, retained placenta, ascariasis, malaria, swollen legs, hypertension, jaundice and wounds, diabetes, fever, and malaria [153,154].
Hagenia abyssinica
Rosaceae, in the order Rosals, is a large family containing more than 100 genera and 2,000 species of herbs, shrubs, and trees of economic value, both for food (e.g., fruit trees including plums, apples, pears, loquats, blackberries and strawberries) and as ornamentals (e.g., flowers of the genus Rosa) . This family is represented on all continents except Antarctica [155,156]. Hagenia abyssinica (Bruce) J. F. Gmel is commonly known as Kosso in Ethiopia belongs to a monotypic genus in the family Rosaceae. It is a deciduous tree with distinct male and female trees, both of which are endowed with colourful flowers. The tree attains heights of up to 20 m, with a short trunks and thick branches. The flowers are greenish or white, turning reddish to maturity in female flowers. In Ethiopia, H. abyssinicawas once abundant in the semi-humid mountain woodlands with the altitudinal range of between 2,450 and 3,250 m. The traditional healer claims that kosso are also useful in the treatment of fever/cough, intestinal worms (tape worm), stomachache, diarrhea, healing of wounds, typhoid, bronchitis, epilepsy, livestock disease (thin/skinny body), evil eyes, hepatitis, sexually transmitted diseases (STDs), throat disease, problems related to bile cancer (mixed with other plants), dermatology, and malaria [157-160]. The female flowers of Kosso have long been used to expel tapeworms, a widespread infestation among Ethiopians due to the age-long practice of eating raw beef by a large sector of the population [161]. It is used in the treatment of syphilis together with powdered bark of Albizzia anthelminticaand against scrophulous tumours and cough. Women also use the bark ofH. abyssinicaduring childbirth to prevent blood clotting and use to treat skin diseases. The seeds and the resin are toxic and are used as a fish poison. Decoction of the roots is used as a laxative. Oil of the seed is used against ear inflammations. The soup of leaves for headaches; inhaling smoke from burning leaves or drinking the leaf sap is said to relieve the pains of a woman in labour; chewing the root, bark or wood relieves toothache. The juice of flowers and leaves is used for hypertension and diabetes mellitus [157,158]. Besides being a source of medicine, Hagenia abyssinica has been utilized for various other purposes such as construction, furniture, fuel wood, and soil fertility management. As a result of its enormous significance, H. abyssinica is one of the endangered tree species in the country due to over exploitation [162].
Conclusion
Traditional medicine is commonly regarded as an indigenous, unorthodox, alternative or folk and largely orally transmitted practice used by communities with different cultures. If any evidence of activity is observed, the extract is fractioned, and the active compound is isolated and identified. Besides their use in fighting various ailments, medicinal plants are used as export commodities, which generate considerable income. From a pathophysiological perspective, it is obvious that HTN is not purely an increase of blood pressure values, but rather a sophisticated web of neurohormonal and haemodynamic interactions. Depending on the underlying causes of the condition, HTN is categorized as primary (essential) and secondary. HTN is the most important public health problem in the world as well as imposes severe economic burdens. HTN is common and readily detectable; many standard antihypertensive drugs are used to manage blood pressure levels in hypertensive patients. However, the frequent side effects that comes with the use of these synthetic antihypertensive drugs. These antihypertensive drugs also increase the risk of developing new diseases. Clinically, various antihypertensive drugs have been also used to manage HTN and to alleviate symptoms. Therefore, newer antihypertensive agents are needed to expand therapeutic options, increase treatment efficacy, decrease side effects, and enhance patient adherence. It is estimated that 70 – 80% of people worldwide rely chiefly on traditional, largely herbal medicines to meet their primary healthcare needs. Modern studies on traditional medicinal plants in Ethiopia started in 1973. Nowadays, the rate of bioassay-guided fractionation has been significantly enhanced by the development of precision instruments. Despite the success of research to produce medicinal plants over the past few decades, future efforts face many challenges. Many scientific studies suggest different life style changes such as stress reduction, proper diet, regular exercise, limited salt intake, smoking cessation, limited alcohol intake, and the use of appropriate herbal medicines in the management of HTN. The Rumex species, cymbopogon citratus, cymbopogon citratus stapf, calpurnia aurea, thymus species, genus ajuga, hagenia abyssinica are common medicinal plants used for the management of hypertension in Arsi zone of Ethiopia.
Availability of Data and Materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Ethical Approval
Ethical approval was obtained from Arsi University Ethical Review Committee (No.CoHS/CS/005/2018/2019).
Competing Interests
The author declares that there is no conflict of interests regarding the publication of this paper.
Authors Contribution
LM had participated in the design of the study, data analyses, and manuscript preparation; and the authors could have read and approved the final manuscript.
Acknowledgement
The author is grateful to College of Health Sciences Research and Community Office of Arsi University as well as supervisors for their support and contribution.
Rights and Permissions
This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise, in a credit line to the material. If the material is not included in the article's Creative Commons licence and your intended use is not permitted by the statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
REFERENCES
- Cotton C, Wilkie P. Ethnobotany: Principles and applications. In: Chichester, New York: John Wiley and Sons Ltd., USA. 1996.
- Nigussie G. Isolation and Characterization of the Roots of Rumex nervosus. J Trop Pharm Chem. 2020;5(1):39-50.
- Li W, Lin Z, Yang C, Wang Y, Qiao Y. Study on the chemical constituents of Momordica charantia L. leaves and method for their quantitative determination. Biomed Res J. 2015;26:415–419.
- Rout SP, Choudary KA, Kar DM, Das LO, Jain A. Plants in traditional medicinal system-future source of new drugs. Int J Pharm Pharm Sci. 2009;1(1):1-23.
- Rai LK, Prasad P, Sharma E. Conservation threats to some important medicinal plants of the Sikkim Himalaya. Biological conservation. 2000;93(1):27-33.
- Jamshidi-Kia F, Lorigooini Z, Amini-Khoei H. Medicinal plants: past history and future perspective. J Herbmed Pharmacol. 2018;7:1–7.
- Sarker SD, Nahar L. Chemistry for pharmacy students. John Willey & Sons Ltd. USA. 2007:322-324.
- Shakya AK, Sharma N, Saxena M, Shrivastava S, Shukla S. Evaluation of the antioxidant and hepatoprotective effect of Majoon-e-Dabeed-ul-ward against carbon tetrachloride induced liver injury. Exp Toxicol Pathol. 2012;64(7-8):767-773.
- Devi MR, Krishnakumari S. Quantitative estimation of primary and secondary metabolites in hot aqueous extract of Pleurotus sajor caju. J Pharmacogn Phytochem. 2015;4(3):198.
- Zohra SF, Meriem B, Samira S, Muneer MA. Phytochemical screening and identification of some compounds from mallow. J Nat Prod Plant Resour. 2012;2(4):512-516.
- Schroeder FC, Gronquist M. Extending the scope of NMR spectroscopy with microcoil probes. Angew Chem Int Ed Engl. 2006;45:7122–7131.
- Yadav M, Chatterji S, Gupta SK, Watal G. Preliminary phytochemical screening of six medicinal plants used in traditional medicine. Int J Pharm Pharm Sci. 2014;6(5):539-42.
- Clark AM. Natural products as a resource for new drugs. Pharm Res. 1996;13(8):1133-41.
- Bentley R. Medicinal Plants. Domville-Fife Press, London, UK. 2010.23–46.
- Simmonds MS. Medicinal plants of the world: Volume 3 Chemical constituents, traditional and modern medicinal uses, Ivan A. Ross, Humana Press Inc., New Jersey, USA. 2005;623.
- Kotwani P, Kwarisiima D, Clark TD, Kabami J, Geng EH, Jain V, et al. Epidemiology and awareness of hypertension in a rural Ugandan community: a cross-sectional study. BMC Public Health. 2013;13(1):1151.
- Chow CK, Teo KK, Rangarajan S, Islam S, Gupta R, Avezum A, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA. 2013;310(9):959-968.
- Ionov MV, Zvartau NE, Konradi AO. Status of hypertension in Russia and Eastern Europe. E-Journal of Cardiology Practice. 2019;17:1–5.
- Ng K, Stanley A, Williams B. Hypertension. Medicine. 2010;38:403–408.
- Ethiopian Review. Blood pressure treatments: Disadvantages of anti-hypertensive drugs. Ethiopian News & Opinion Journal; 2008.
- Rout SK, Dutta S, Sengupta M, Das S, Rout B. Antihypertensive therapy: The concepts of management with herbal and synthetic agents for pulmonary hypertension. Int. J Pharm Sci Rev Res. 2010;3(2):72–79.
- Garovic VD, Textor SC. Renovascular hypertension and ischemic nephropathy. Circulation. 2005;112(9):1362-1374.
- Global Burden of Disease Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1923–1994.
- WHO. Cardiovascular Diseases (CVDs). Geneva, Switzerland: World Health Organization; 2013. Report No.: No 317.
- Palano F, Paneni F, Sciarretta S, Tocci G, Volpe M. The progression from hypertension to congestive heart failure. Recenti Prog Med. 2011;102:461–467.
- World Health Report. Reducing Risks, Promoting Healthy Life [Internet]. World Health Report 2013: Research for Universal Health Coverage. 2013.
- Lawes CM, Vander Hoorn S, Rodgers A. Global burden of blood-pressure-related disease, 2001. The Lancet. 2008;371(9623):1513-1518.
- GBD 2013 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risk factors or clusters of risks in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:2287–2323.
- Forouzanfar MH, Liu P, Roth GA, Ng M, Biryukov S, et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990-2015. JAMA. 2017;317(2):165–182.
- Egan BM, Kjeldsen SE, Grassi G, Esler M, Mancia G. The global burden of hypertension exceeds 1.4 billion people: should a systolic blood pressure target below 130 become the universal standard?. J Hyperten. 2019;37(6):1148-1153.
- August P. Overview: Mechanisms of hypertension: Cells, hormones, and the kidney. J Am Soc Nephrol. 2004;15(8):1971–1973.
- Freedman B, Cohen A. Hypertension-attributed nephropathy: What’s in a name? Nat Rev Nephrol. 2016;12(1):27–36.
- Hendriks ME, Wit FW, Roos MT, Brewster LM, Akande TM, De Beer IH, et al. Hypertension in sub-Saharan Africa: cross-sectional surveys in four rural and urban communities. PloS one. 2012;7(3):32638.
- López-Jaramillo P, Sánchez R, Diaz M, Cobos L, Bryce A, Parra Carrillo J, et al. Latin American consensus on hypertension in patients with diabetes type 2 and metabolic syndrome. J Hypertens. 2013;31:223–238.
- Yu X, Lyu D, Dong X, He J, Yao K. Hypertension and risk of cataract: A meta-analysis. PloS one. 2014;9(12):114012.
- Parati G, Bilo G, Ochoa JE. Benefits of tight blood pressure control in diabetic patients with hypertension: importance of early and sustained implementation of effective treatment strategies. Diabetes Care. 2011;34(Supplement 2):297-303.
- Skoog I, Nilsson L, Persson G, Lernfelt B, Landahl S, Palmertz B, et al. 15-year longitudinal study of blood pressure and dementia. The Lancet. 1996;347(9009):1141-1145.
- Kearney PM, Whelton M, Reynolds K, Whelton PK, He J. Worldwide prevalence of hypertension: A systematic review. J Hypertens. 2004;22(1):11-9.
- Elliott WJ. The economic impact of hypertension. J Clin Hypertens. 2008;5(3):3–13.
- Yach D, Hawkes C, Gould CL, Hofman KJ. The global burden of chronic diseases: overcoming impediments to prevention and control. JAMA. 2004;291(21):2616-2622.
- Gaziano T, Bitton A, Anand S, Weinstein M. International Society of Hypertension. The global cost of nonoptimal blood pressure. J Hypertens. 2009;27:1472–1477.
- Kirkland EB, Heincelman M, Bishu KG, Schumann SO, Schreiner A, Axon RN, et al. Trends in healthcare expenditures among US adults with hypertension: national estimates, 2003-2014. J Am Heart Assoc. 2018;7(11):008731.
- Kochanek K, Xu J, Murphy S, Miniño A, Kung H. Deaths: Final data for 2009. National vital statistics reports; 2011;59(4):1.
- From Burden to “Best Buys”: Reducing the Economic Impact of Non-Communicable Diseases in Low- and Middle-Income Countries. In Geneva, Switzerland: World Health Organization and World Economic Forum; 2011:12.
- WEF. The Global Economic Burden of Non-communicable Diseases. World Economic Forum and the Harvard School of Public Health. 2011.
- Lindholm LH. The problem of uncontrolled hypertension. J Hum Hypertens. 2002;16:S3–8.
- Archer J. Evaluation and treatment of hypertension. Prim Care Update Ob Gyns. 2000;7:1–6.
- Susalit E, Agus N, Effendi I, Tjandrawinata R, Nofiarny D, PerrinjaquetMoccetti T, et al. Olive (Olea europaea) leaf extract effective in patients with stage-1 hypertension: comparison with Captopril. Phytomedicine. 2011;18(4):251–258.
- Yeh C, Huang W, Yen G. Antihypertensive effects of Hsian-Tsao and its active compound in spontaneously hypertensive rats. J Nutr Biochem. 2009;20:866–875.
- Testa MA. Quality of life during antihypertensive therapy: Techniques for clinical assessment and evaluation. Br J Clin Pharmacol. 1987;23:9S-13S.
- Munir S, Karim A. South Asian herbal plants as anti-hypertensive agents-A review. Sci Int. 2013;1(1):2–12.
- Black H, Elliott W, Grandits G, Grambsch P, Lucente T, White W, et al. Principal results of the Controlled Onset Verapamil Investigation of Cardiovascular End Points (CONVINCE) Trial. JAMA. 2003;289:2073–2082.
- Dahlof B, Devereux R, Kjeldsen S, Julius S, Beevers G, Faire U, et al. Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint Reduction in Hypertension Sudy (LIFE): A randomised trial against atenolol. Lancet. 2002;359:995–1003.
- Cushman W, Ford C, Cutler J, Margolis K, Davis B, Grimm R, et al. Success and predictors of blood pressure control in diverse North American settings: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). J Clin Hypertens (Greenwich). 2002;4:393–404.
- Cooper D, Krainik A, Lubner S, Reno H. The Washington manual of medical therapeutics. In: 32th edition. New York, USA: Lippincott Williams & Wilkins; 2007.
- Wang J, Xiong X. Outcome measures of chinese herbal medicine for hypertension: an overview of systematic reviews. Evid Based Complem Alternat Med. 2012;2012:697237.
- Patel P, Vaghasiya J, Thakor A, Jariwala J. Antihypertensive effect of rhizome part of Acorus calamus on renal artery occlusion induced hypertension in rats. Asian Pacific Journal of Tropical Disease. 2012;2:6–10.
- Hong F, Ming L, Yi S, Zhanxia L, Yong-Quan W, Chi L. The antihypertensive effect of peptides: A novel alternative to drugs. Peptides. 2008;29:1062–1071.
- Qian Z, Jung W, Lee S, Byun H, Kim S. Antihypertensive effect of an angiotensin I-converting enzyme inhibitory peptide from bullfrog (Rana catesbeiana Shaw) muscle protein in spontaneously hypertensive rats. Process Biochem. 2007;42:1443–1448.
- Patel V, Yahyavi H, Arabian M. Antispasmodic activity of onion (Allium cepa L.) peel extract on rat ileum. Iranian J Pharm Res. 2008;7:155–159.
- Farnsworth N, Soejarto D. Global importance of medicinal plants. In: In The observation of medicinal plants. Akerele O, Heywood V and Synge H. (Eds) Cambridge University Press, UK. 1991:25–51.
- Shengji P. Ethnobotanicalapproaches of traditional medicine studies: some experiences from Asia. Pharma Botany. 2001;39:74–79.
- Lulekal E, Asfaw Z, Kelebessa E, Van Damme P. Ethnoveterinary plants used in Ankober District, North Shewa Zone, Amhara Region, Ethiopia. J Ethnobiol Ethnomed. 2014;10:21.
- Kibebew F. The status and availability of oral and written knowledge on traditional health care on traditional health care in Ethiopia. In: Conservation and sustainable use of medicinal plants in Ethiopia. Addis Ababa, Ethiopia: Institute of Biodiversity Conservation and Research; 1998:107–119.
- Tadesse M, Mesfin B. A review of selected plants used in the maintenance of health and wellness in Ethiopia. Ethiopian e-journal for Research & Innovation foresight. 2010;2:85–102.
- Dawit A, Ahadu A. Medicinal plants and enigmatic health practice of north Ethiopia. In Addis Ababa, Ethiopia: Berhanina Selam Printing Enterprise; 1993:341.
- Birhane E, Aynekulu E, Mekuria W, Endale D. Management, use and ecology of medicinal plants in the degraded dry lands of Tigray, Northern Ethiopia. J Hortic For. 2011;3:32–41.
- Getahun A. Some common medicinal and poisonous plants used in Ethiopian folk medicine. Addis Ababa, Ethiopia: Addis Ababa University; 1976.
- Giday M, Asfaw Z, Woldu Z. Ethnomedicinal study of plants used by Sheko ethnic group of Ethiopia. Journal of Ethnopharmacology. 2010;132:75–85.
- Bekalo T, Woodmatas S, Woldemariam Z. An ethnobotanical study of medicinal plants used by local people in the lowlands of Konta Special Woreda, southern nations, nationalities and peoples regional state, Ethiopia. J Ethnobiology Ethnomedicine. 2009;5:26.
- Megersa M, Asfaw Z, Kelbessa E, Beyene A. An ethnobotanical study of medicinal plants in Wayu Tuka District, East Welega Zone of Oromia Regional State, West Ethiopia. Journal of Ethnobiology and Ethnomedicine. 2013;6:68.
- Zhang H. Bioactive natural products: Detection, isolation, and structural determination. Phytomedicine. 2011;18:902–903.
- Singh R. Medicinal plants: A review. J Plant Sci. 2015;3:50–55.
- Nakanishi N, Li W, Fukuda H. Multiple risk factor clustering and risk of hypertension in Japanese male office workers. Ind Health. 2003;41:327–331.
- Maghrani M, Zeggwagh N, Haloui M, Eddouks M. Acute diuretic effect of aqueous extract of Retama raetam in normal rats. J Ethnopharmacol. 2005;99:31–33.
- Joshi U, Ganatra T, Bhalodiya P, Desai T, Tirgar P. Comparative review on harmless herbs with allopathic remedies as antihypertensive. RJPBCS. 2012;3:673–687.
- Benefits of Vitapharmica.
- Ghorbani M. Iranian traditional medicine for treatment of type II diabetes, anxiety and hypertension with introduction of zebrafish model system for their screening. Int J Herbal Med. 2014;2:13–19.
- Singh P, Mishra A, Singh P, Goswami S, Singh A, Dev Tiwari K. Hypertension and herbal plant for its treatment: a review. Indian Journal of Research in Pharmacy and Biotechnology. 2015;3:358.
- Uddin K, Mahbubur Rahman A, Rafiul Islam A. Taxonomy and Traditional Medicine Practices of Polygonaceae (Smartweed) Family at Rajshahi, Bangladesh. IJAR. 2014;2:459–469.
- Gescher K, Hensel A, Hafezi W, Derksen A, Kühn J. Oligomeric proanthocyanidins from Rumex acetosa L. inhibit the attachment of herpes simplex virus type-1. Antiviral Research. 2011;89:9–18.
- Jiang L, Zhang S, Xuan L. Oxanthrone Cglycosides and epoxynaphthoquinol from the roots of Rumex japonicus. Phytochemistry. 2007;68:2444–2449.
- Liang H, Dai H, Fu H, Dong X, Adebayo A, Zhang L, et al. Bioactive compounds from Rumex plants. Phytochemistry Letters. 2010;3:181–184.
- Mei R, Liang H, Wang J, Zeng L, Lu Q, Cheng Y. New seco-anthraquinone glucosides from Rumex nepalensis. Planta Med. 2009;75:1162–1164.
- Wegiera M, Smolarz H, Wianowska D, Dawidowicz A. Anthracene derivatives in some species of Rumex L. genus. Acta Soc Bot Pol. 2007;76:103–108.
- Saleh N, El-Hadidi M, Arafa R. Flavonoids and anthraquinones of some Egyptian Rumex species (Polygonaceae). Biochemical systematics and ecology. 1993;21:301–303.
- Süleyman H, Demirezer L, Kuruüzüm A, Banoğlu Z, Göçer F, Ozbakir G, et al. Anti-inflammatory effect of the aqueous extract from Rumex patientia L. roots. J Ethnopharmacol. 1999;65:141–148.
- Ghosh L, Gayen J, Murugesan T, Sinha S, Pal M, Saha B. Evaluation of purgative activity of roots of Rumex nepalensis. Fitoterapia. 2003;74:372–374.
- Demirezer L, Kuruuzum-Uz A, Bergere I, Schiewe H, Zeeck A. The structures of antioxidant and cytotoxic agents from natural source: Anthraquinones and tannins from roots of Rumex patientia. Phytochemistry. 2001;58:1213–1217.
- Rouf A, Islam M, Rahman M. Evaluation of antidiarrhoeal activity Rumex maritimus root. J Ethnopharmacol. 2003;84:307–310.
- Gebrie E, Makonnen E, Debella A, Zerihun L. Phytochemical screening and pharmacological evaluations for the antifertility effect of the methanolic root extract of Rumex steudelii. J Ethnopharmacol. 2004;96:139–143.
- Cos P, Hermans N, Bruyne T, De Apers S, Sindambiwe J, Witvrouw M, et al. Antiviral activity of Rwandan medicinal plants against human immunodeficiency virus type-1 (HIV-1). Phytomedicine. 2002;9:62–68.
- Singh S, Kaur R, Sharma S. Antinociceptive, anti-inflammatory and antipyretic activities of Rumex hastatus D. Don stem and roots Der Pharmacia Sinica. 2013;4:95–102.
- Rao K, Sunitha C, Banji D, Sandhya S, Mahesh V. A study on the nutraceuticals from the genus Rumex hygeia. JD Med. 2011;3:76–88.
- Mekonnen T, Urga K, Engidawork E. Evaluation of the diuretic and analgesic activities of the rhizomes of Rumex abyssinicus Jacq in mice. J Ethnopharmacol. 2010;127:433–439.
- Ahmad S, Ullah F, Ayaz M, Sadiq A, Imran M. Antioxidant and anticholinesterase investigations of Rumex hastatus D. Don, potential effectiveness in oxidative stress and neurological disorders. Biol Res. 2015;48:20.
- Hussain F, Hameed I, Dastagir G, Khan I, Ahmad B. Cytotoxicity and phytotoxicity of some selected medicinal plants of the family Polygonaceae. African Journal of Biotechnology. 2010;9:770–774.
- Dangupen M, Januszewska R, Lino L, Tagarino D, Viaene J, Arguelles R, et al. Consumers behavior toward lemongrass (Cymbopogon citratus) tea in Benguet Province, Northern Philippines. BANWA: A Multidisciplinary Journal. 2009;6:1–12.
- Akande I, Samuel T, Agbazue U, Olowolagba B. Comparative proximate analysis of ethanolic and water extracts of Cymbopogon citratus (lemon grass) and four tea brands. Plant Sci Res. 2011;3:29–35.
- Ekpenyong C, Akpan E, Udokang N. Clinical correlates of physiochemical changes in urinary composition in subjects treated with Cymbopogon citratus infusion. Elixir Human Physio. 2014;68:22081–22086.
- Tarkang P, Agbor G, Tsabang N, Tchokouaha R, Tchamgoue D, Kemeta D. Effect of long-term oral administration of the aqueous and ethanol leaf extract of Cymbopogon citratus (DC. Ex Ness) Stapf. Annals Biol Res. 2012;3:5561–5570.
- Negrelle R, Gomes E. Cymbopogon citratus (DC) Stapf: Chemical composition and biological activities. Rev Bras Pl Med. 2007;9:80–92.
- Akhila A. Essential oil bearing plants: The genus Cymbopogon. Edited by: Anand Akhila [M]. Broca Raton, FL: CRC Press Taylor & Francis Group; 2010.
- Miean K, Mohamed S. Flavonoid (Myricitin, Quercetin, Kaempferol, Luteolin, and Apigenin) content of edible tropical plants. J Agric Food Chem. 2001;49:30106–30112.
- Faruq M. TLC technique in the component characterizations and quality determination of Bangladeshi lemongrass oil (Cymbopogon citratus) (DC) Stapf.). Bangladesh J Sci Ind Res. 1994;29:27–38.
- Cheel J, Theoduloz C, Rodriguez J, Schmeda-Hirschmann G. Free radical and antioxidants (Cymbopogon Citratus (DC) Staff.). J Agric Food Chem. 2005;53:2511–2517.
- Bharti S, Kumar A, Prakash O, Krishnan S, Gupta A. Essential oil of Cymbopogon citratus against diabetes: validation by in vivo experiments and computational studies. J Bioanal Biomed. 2013;5:194–203.
- Aftab K, Ali M, Aijaz P, Beena N, Gulza H, Sheikh K. Determination of different trace and essential element in lemon grass samples by X-ray fluorescence spectroscopy technique. Int Food Res J. 2011;18:265–270.
- Wannissorn B, Jarikasem S, Siriwangchai T, Thubthimthed S. Anti-bacterial properties of essential oils from Thai Medicinal plants. Fitoterapia. 2005;76:233–236.
- Nakagawa T, Mazzali M, Kang D, Kanellis J, Watanebe S, Sanchez-Lozada L, et al. Hyperuricemia causes glomerular hypertrophy in the rat. Am J Nephrol. 2003;23:2–7.
- Holetz F, Ueda-Nakamura T, Filho B, Cortez B, Morgado-Diaz J, Nakamura C. Effect of Essential Oil of Ocimum gratissimum on the Typanosomatid herpetomonas Samuelpessoai. Acta Protozool. 2003;42:269–276.
- Puatonachokchai R, Kishida H, Denda A, Murata N, Konishi Y, Vinitketkumnuen U. Inhibitory Effects of Lemon Grass (Cymbopogon citratus Stapf) Extract on The Early Phase of Hepatocarcinogenesis after Initiation with Ethyinitrosamine in Male Fischer 344 Rats. Cancer Letters. 2002;183:9–15.
- Abe S, Maruyama N, Hayama K, Inuoye S, Oshima H, Yamauchi H. Suppression of neutrophils recruitment in mice by geranium essential oil. Mediators Inflamm. 2004;13:21–24.
- Masuda T, Odaka Y, Ogawa N, Nakamoto K, Kuninaga H. Identification of Geranic Acid, a Tyrosinase Inhibitor in Lemongrass (Cymbopogon citratus). J Agric Food Chem. 2008;56:597–601.
- Gazola R, Machado D, Ruggiero C, Singi G, Mecado M. Lippia alba, Melissa Officinalis and Cymbopogon Citratus Effects of the Aqueous Extracts on the Isolated Hearts of Rats. Pharmacol Res. 2004;50:477–480.
- Tognolini M, Barocelli E, Ballabeni V, Bruni R, Biandi M, Impicciatore M. Comperative screening of plants essential oils, phenylpropanoid as basic core for antiplatelet activity. Life Science. 2006;78:1419–1432.
- Mansour H, Newairy A, Youset M, Sheweita M. Biochemical Study on the Effects of Some Egyptian Herbs in Alloxan-Induced Diabetic Rats. Toxicology. 2002;170:221–228.
- Carlini E, De-Contar J, Siloai-Filho A, DeSilreiral-Filho N, Fronchtengarten M, Bveno O. Pharmacology of Lemon Grass (Cymbopogon citratus Stapf). J Ethnoparmacol. 1986;17:37–64.
- Peigen X. Recent Developments on Medicinal Plants in China. J Ethnopharmacol. 1983;7:95–109.
- Tchoumbougnang F, Zollo P, Dagne E, Mekonnen Y. In vivo Anti malaria activity of essential oils from Cymbopogon Citratus and Ocimum Gratissimum on Mice Injected with Plasmodium Berghei. Planta Medica. 2005;71:20–23.
- Lorenzetti B. Myrcene mimics the peripheral analgesic activity of lemongrass tea. J Ethnopharmacol. 1991;34:43–48.
- De-Oliveira A, Ribeiro-Pinto L, Otto S, Goncalves A, Paumgartten F. Induction of liver mono-oxygenase by β-myrcene. Toxicology. 1997;124:135–140.
- Carlini E, De-Contar J, Siloai-Filho A, De-Silreiral-Filho N, Fronchtengarten M. Bveno Of Pharmacology of Lemon Grass (Cymbopogon citrates Stapf). J Ethnoparmacol. 1986;17:37–64.
- Figueirinha A, Paranhos A, Perez-Alonso J, Santos-Buelga C, Batista M. Cymbopogon citratus leaves. Characterisation of flavonoids by HPLC-PDA-ESI/MS and an approach to their potential as a source of bioactive polyphenols. Fd Chem. 2008;110:718–728.
- Sugumaran M, Joseph S, Lee K, Wong K. Herbs of Malaysia. Shah Alam: Federal Publication. 2005.
- Promila P, Madan V. A review on the phytochemistry and pharmacology of Cymbopogon citratus Stapf. (Lemongrass). Pharma Innovation. 2018;7:300–304.
- Korir E, Joyce J, Neil R, Nivan M, Neil A. Isoflavones from Calpurnia aurea Subsp. aurea and their anticancer activity. Afr J Tradit Complement Altern Med. 2014;11:33–37.
- Gemechu A, Mirutse G, Adane W, Gobena A. In vitro Anti-mycobacterial activity of selected medicinal plants against Mycobacterium tuberculosis and Mycobacterium bovis Strains. BMC Complementary and Alternative Medicine. 2013;13:291.
- Waka M, Hopkins R, Curtis C. Ethnobotanical survey and testing of plants traditionally used against hematophagous insects in Eritrea. Journal of Ethnopharmacology. 2004;95:95–101.
- Mulata N, Seifu D, Umeta M, Wendwesson E, Natesan G. Protective Effects of Calpurnia aurea Seed Extract on HAART Hepatotoxicity. EJMP. 2015;9:1–12.
- Desta B. Ethiopian traditional herbal drugs. Part III: Anti-fertility activity of 70 medicinal plants. Journal of Ethnopharmacology. 1994;44:199–209.
- Jansen P. Spices, condiments and medicinal plants in Ethiopia, their taxonomy and agricultural significance: Pudoc; 1981. [Dissertation, internally prepared]. [Netherlands]: Biosystematiek-Diertaxonomie; 1981.
- Abebe W. A survey of prescriptions used in traditional medicine in Gondar region, northwestern Ethiopia: general pharmaceutical practice. Journal of Ethnopharmacology. 1986;18:147–165.
- Asres K, Bucar F, Kartnig T, Witvrouw M, Pannecouque C, De Clercq E. Antiviral activity against human immunodeficiency virus type 1 (HIV-1) and type 2 (HIV-2) of ethnobotanically selected Ethiopian medicinal plants. Phytotherapy Research. 2001;15:62–69.
- Tadeg H. Phytopharmaceutical Studies of Some Selected Medicinal Plants Locally Used in the Treatment of Skin Disorders [B. Pharm]. [Ethiopia]: Addis Abeba University. 2004.
- Morales R. The history, botany and taxonomy of the genus Thymus. In: Thyme: The Genus Thymus. In: Stahl-Biskup, E. & Sáez, F. London, England: CRC Press Taylor & Francis Group; 2002:1–43.
- Ozudogru E, Kaya E, Kirdok E. Development of protocols for short-, medium and long-term conservation of thyme. Acta Horticulturae. 2011;918:43–50.
- Stahl-Biskup E. Thyme as a herbal drug pharmacopoeias and other product characteristics. In: Thyme: The Genus Thymus. In: Stahl-Biskup E. & Sáez F. (Eds) London, England: CRC Press Taylor & Francis Group; 2002:293–316.
- Huang M, Ho C, Wang Z, Ferraro T, Lou Y, Stauber K, et al. Inhibition of skin tumorigenesis by rosemary and its constituents carnosol and ursolic acid. Cancer Research. 1994;54:701–708.
- Liu J. Pharmacology of oleanolic acid and ursolic acid. J Ethnopharmacol. 1995;49:57–68.
- Liu J. Oleanolic acid and ursolic acid: Research perspectives. J Ethnopharmacol. 2005;100:92–94.
- Rey C, Sáez F. Field culture, in vitro culture and selection of Thymus. In: Thyme, the Genus Thymus. In: StahlBiskup E. & Sáez F. London, England: Taylor & Francis; 2002:177–196.
- Shabnum S, Wagay M. Micropropagation of different species of Thymus. J Res Dev. 2011;11:71–81.
- Snigdha M, Kumar S, Sharmistha M, Lalit S, Tanuja S. An overview on herbal medicines as diuretics with scientific evidence. Scholars Journal of Applied Medical Science. 2013;1:209–214.
- Haji H, Makonnen E, Debella A, Geleta B. Evaluation of diuretic and antihypertensive activity of leaf extracts of Thymus schimperi in Rats. British J Pharmacol Toxicol. 2016;7:1–8.
- Geleta B, Eyasu M, Kebamo S, Debella A, Makonnen E, Abebe A. In vitro vasodilatory effect of aqueous leaf extract of Thymus serrulatus on thoracic aorta of Guinea pigs. Asian Pacific Journal of Tropical Biomedicine. 2015;5:15–18.
- Fichtl R, Adi A. Honeybee flora of Ethiopia. DED (German Development Service) and Ministry of Agriculture-Livestock and Fishery Resources. Margraf Verlag. Weikersheim, Germany: Margraf Verlag. 1994:510.
- Dagne E. Natural Database for Africa (NDA). Version 1.0. 2009.
- Hedberg I, Kelbessa E, Edwards S, Demissew S, Persson E. Flora of Ethiopia and Eritrea: Gentianaceae to Cyclocheilaceae. In: The National Herbarium. 5th ed. Uppsala Sweden and Addis Ababa, Ethiopia: Department of Systematic Botany, 2006.
- Bekele T. Antidiabetic activity and phytochemical screening of crude extracts of Stevia rebaudiana Bertoni and Ajuga remota Benth grown in Ethiopia on alloxan-induced diabetic mice [MSc Thesis]. [Ethiopia]: Addis Ababa University; 2008.
- Andarge E, Shonga A, Agize M, Tora A. Utilization and conservation of medicinal plants and their associated Indigenous Knowledge (IK) in Dawuro Zone: An ethnobotanical approach. International Journal of Medicinal Plant Research. 2015;4:330–337.
- Vohra A, Kaur H. Chemical investigation of medicinal plant Ajuga bracteosa Organic Chemistry (Natural Product). J Nat Prod Plant Resour. 2011;1:37–45.
- Alebie G, Urga B, Worku A. Systematic review on traditional medicinal plants used for the treatment of malaria in Ethiopia: trends and perspectives. Malaria Journal. 2017;16:307.
- Giday M, Asfaw Z, Woldu Z. Medicinal plants of the Meinit ethnic group of Ethiopia: An ethnobotanical study. J Ethnopharmacol. 2009;124:513–521.
- Teklay A, Abera B, Giday M. An ethnobotanical study of medicinal plants used in Kilte Awulaelo district, Tigray Region of Ethiopia. J Ethnobiol Ethnomedicine. 2013;9:65.
- Assefa B, Glatzel G. Measuring soil fertility under Hagenia Abyssinica (bruce) jf gmel by the bio test method. International Journal of Agronomy. 2010;2010:5.
- Bekele G, Reddy P. Folklore medicinal uses of Hagenia abyssinica (Bruce) J.F. Gmel to treat human ailments by Guji Oromo tribes in Abaya district, Borana Zone, Oromia regional state Ethiopia. IJPSS 2014;4:394.
- Assefa B, Glatzel G, Buchmann C. Ethnomedicinal uses of Hagenia abyssinica (bruce) j f gmel. Among rural communities of Ethiopia. J Ethnobiol Ethnomed. 2010;6:20.
- Regassa R. Assessment of indigenous knowledge of medicinal plant practice and mode of service delivery in Hawassa city, southern Ethiopia. J Med Plant Res. 2013;7:517–535.
- Githiori J. Evaluation of anthelmintic properties of ethnoveterinary plant preparations used as livestock dewormers by pastoralists and small holder farmers in Kenya [Doctoral thesis]. [Uppsala, Sweden]: Swedish University of Agricultural Sciences, 2004.
- Pankhurst R. Europe’s discovery of the Ethiopian taenicide--kosso. Medical history. 1979;23.
- Kumilign A. Estimation of sex− related genetic diversity of Hagenia Abyssinica (bruce) j f gmel using random amplified polymorphic [MSc Thesis]. [Ethiopia]: Addis Ababa University, 2005.
Citation: Melaku L (2021) The Pharmacology and Therapeutic Value of Conventional Antihypertensive Drugs in the Management of Hypertension: An Ethno-Botanical Review of Commonly Used Antihypertensive Medicinal Plants in Arsi Zone, South-East Ethiopia. J Plant Pathol Microbiol 12:549.
Copyright: © 2021 Melaku L. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.