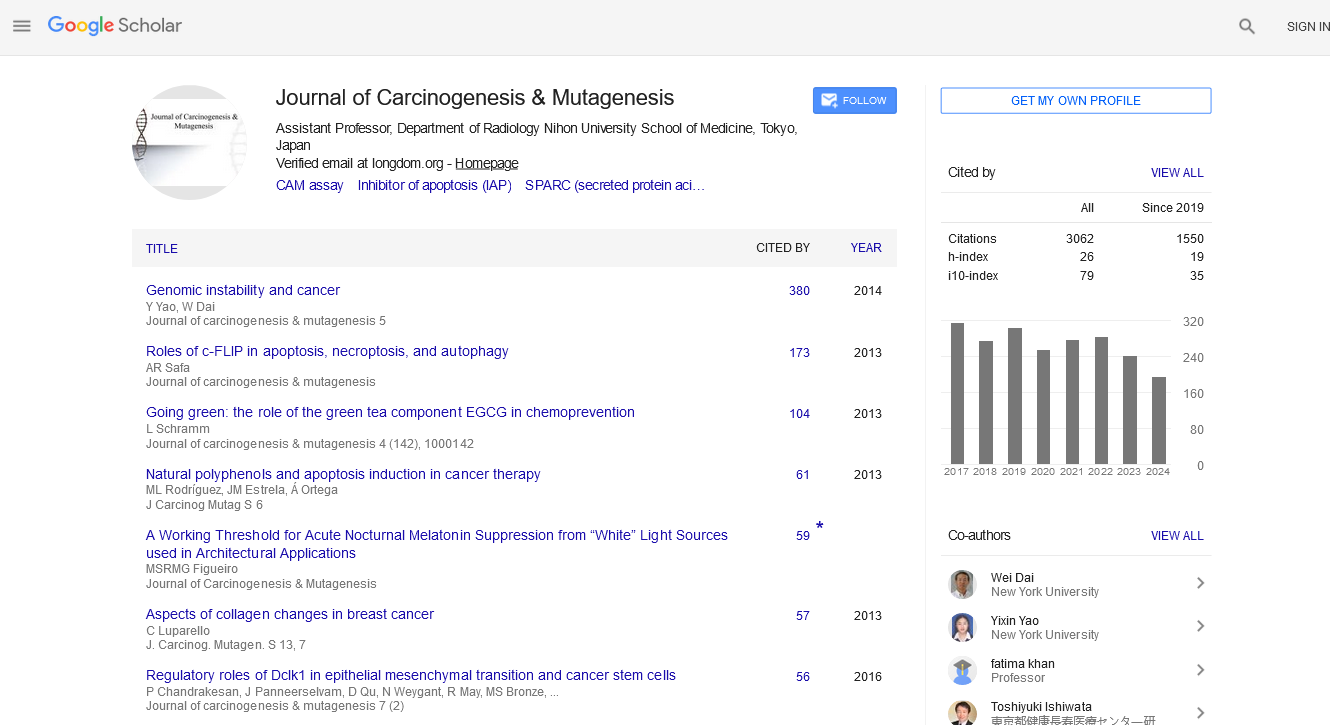
Indexed In
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Perspective - (2024) Volume 0, Issue 0
The Intersection of Genetics and Drug Therapy in Pharmacogenomics
Ya Gao*Received: 30-Jul-2024, Manuscript No. JCM-24-26910; Editor assigned: 01-Aug-2024, Pre QC No. JCM-24-26910 (PQ); Reviewed: 15-Aug-2024, QC No. JCM-24-26910; Revised: 22-Aug-2024, Manuscript No. JCM-24-26910 (R); Published: 30-Aug-2024, DOI: 10.35248/2157-2518.24.S45.004
Description
Pharmacogenomics, a expanding field at the intersection of pharmacology and genomics, holds the declaration of transforming how we approach medication and therapy. By studying how an individual's genetic makeup influences their response to drugs, pharmacogenomics aims to personalize treatment, optimizing efficacy and minimizing adverse effects. This article explains the the core concepts of pharmacogenomics, its current applications and the future it envisions for precision medicine.
The fundamentals of pharmacogenomics
Pharmacogenomics combines pharmacology the study of how drugs interact with the body and genomics, the study of genes and their functions. The goal of pharmacogenomics is to tailor drug treatments to the individual characteristics of each patient, based on their genetic profile. This approach contrasts with the traditional "one-size-fits-all" methodology, where treatments are developed based on the average responses of a population rather than individual variability.
Genetics influence drug response
Genetic variations, particularly Single Nucleotide Polymorphisms (SNPs), can significantly affect drug metabolism, efficacy and safety. For instance, the Cytochrome P450 (CYP) enzyme family, which plays a critical role in drug metabolism, exhibits genetic variability among individuals. Variations in CYP genes can lead to differences in drug metabolism rates. Some individuals may metabolize a drug too quickly, reducing its effectiveness, while others may metabolize it too slowly, increasing the risk of toxicity.
A classic example is the anticoagulant warfarin. The drug’s effectiveness and risk of bleeding complications are influenced by genetic variations in the VKORC1 and CYP2C19 genes. Pharmacogenomic testing can help determine the optimal dose of warfarin for each patient, minimizing risks and improving treatment outcomes.
Current applications of pharmacogenomics
Pharmacogenomics is already making a significant impact in several areas of medicine:
Oncology: In cancer treatment, pharmacogenomics helps tailor therapies based on genetic mutations present in tumors. For example, patients with specific mutations in the EGFR gene may benefit from targeted therapies like erlotinib or gefitinib, which are designed to inhibit cancer cell growth driven by these mutations.
Cardiology: Genetic testing can guide the use of drugs such as clopidogrel, a platelet inhibitor. Variants in the CYP2C19 gene can affect how well the drug works, influencing decisions about alternative medications or dosing strategies.
Psychiatry: Pharmacogenomic testing can inform the treatment of psychiatric disorders. Variations in genes related to neurotransmitter systems can affect responses to antidepressants and antipsychotics, helping clinicians choose the most effective medication with fewer side effects.
Pain management: Genetic differences can influence responses to opioid analgesics. Testing for variants in the OPRM1 gene, which encodes the mu-opioid receptor, can help predict which patients are more likely to experience effective pain relief or adverse effects from opioids.
Challenges and future directions
Despite its potential, pharmacogenomics faces several challenges. One major obstacle is the need for extensive validation and standardization of genetic tests. The clinical utility of many pharmacogenomic tests is still being evaluated and integrating these tests into routine practice requires robust evidence and consensus on best practices.
Moreover, there are ethical and privacy concerns related to genetic testing. Ensuring that genetic information is used responsibly and that patients’ privacy is protected is important as pharmacogenomics becomes more integrated into clinical practice.
Looking ahead, the field of pharmacogenomics is likely to evolve with advances in technology and a better understanding of the genetic basis of drug responses. The integration of pharmaco- genomic data with Electronic Health Records (EHRs) and the development of more comprehensive genetic databases will enhance the ability to personalize treatments further.
Conclusion
Pharmacogenomics represents a significant leap toward personalized medicine, where treatments are tailored to the genetic profiles of individual patients. By improving the efficacy and safety of drug therapies, pharmacogenomics has the potential to revolutionize healthcare, making treatments more precise and effective. As the field advances, it will continue to play an important role in the development of personalized treatment strategies, ensuring that patients receive the most appropriate care based on their unique genetic organization.
Citation: Gao Y (2024). The Intersection of Genetics and Drug Therapy in Pharmacogenomics. J Carcinog Mutagen. S45:004.
Copyright: © 2024 Gao Y. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.