Indexed In
- Academic Journals Database
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Ulrich's Periodicals Directory
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2019) Volume 10, Issue 1
The Experience of Being Tested for Allergies: The Views of Children and Their Parents
Helen Smith1,2*, Clare Brown1, Annalee Robertson1, Laura Stuttaford1, Rabia Rashid3 and Christina J Jones12Lee Kong Chian School of Medicine, Nanyang Technological University Singapore, Singapore
3Royal Sussex County Hospital, Brighton, UK
Received: 16-Feb-2019 Published: 04-Mar-2019
Abstract
Background: Children with suspected allergies can be tested for IgE sensitivities with in vivo or in vitro testing, but parents’ and childrens’ experiences of these different allergy test modalities have not been studied.
Objective: To investigate parents’ and childrens’ experiences and views of allergy testing (Skin Prick Testing (SPT) and allergen-specific IgE blood tests).
Methods: Qualitative study of children and their parents attending a paediatric allergy clinic. Semi-structured interviews were conducted by telephone using an interview guide that explored their experience of allergy testing. Interviews were digitally recorded and transcribed verbatim. Thematic content analysis was performed.
Results: 16 parents and 6 children were interviewed. The characteristics of skin prick tests particularly valued were the immediacy and visibility of results, which enabled testing and interpretation to be achieved within a single clinic appointment. In vitro testing offered simplicity and speed, with only a single puncture site and procedural speed. Some perceived it to be a superior test as it was a laboratory-based test. Parental accounts of in vitro testing often included reference to their own discomfort, as well as their young child’s discomfort as they were restrained for venepuncture.
Conclusion and clinical relevance: Several areas for improvement in allergy testing service provision were highlighted, particularly a need for greater information in advance about what will happen in the allergy clinic to reduce anxiety and misunderstandings. Also, SPT with an already identified allergen can cause concern and distress as it appeared to contradict previous instructions given for allergen avoidance.
Keywords
Children; Parents; Allergy testing; Preference
Introduction
Allergy tests are used, together with the clinical history, to diagnose allergy. Two methods are commonly used for confirming IgE-mediated sensitisation: in vivo SPT or in vitro blood tests for specific IgE. SPT requires specialist training. Drops of allergen reagent are placed onto the skin and a 1 mm lancet is utilised to puncture the epidermis. Positive responses are indicated by development of a wheal and flare response. The blood test measures serum allergen-specific IgE by immunosorbent-linked assay. The SPT is considered the gold standard but blood tests are used when patients have severe eczema, dermatographism or are unable to discontinue using their antihistamines [1].
Adults and parents perceptions of the pathways and accessibility have been investigated [2], including one study of adult’s views of allergy testing [3] but none has addressed childrens ’ or parents ’ experiences of the testing modalities. The UK NHS reform programme, ‘Creating a Patient-Led NHS’ has challenged us to move away from a traditional health service that ‘does things for its patients ’ towards patients having greater involvement in care organisation and delivery [4]. In this context, we explored parents ’ and childrens ’ experiences of allergy testing to enable the development of more patientfocused care, which may improve satisfaction, health outcomes and physicians’ performance [5].
Methods
We chose a qualitative approach that allows participants to raise issues important to them. Parents and children were recruited from a teaching hospital paediatric allergy clinic in southern England. Inclusion required the child to have undergone allergy testing during their most recent outpatient consultation. Children over eight years were eligible to be interviewed concurrently. We provided an age-appropriate information leaflet; children who agreed to be interviewed signed an assent form and their parent a consent form.
In semi-structured telephone interviews the interviewer (LS, AR) enquired about the experience of allergy testing, probing for further detail of any positive or negative characteristics mentioned. Interviews were recorded and transcribed verbatim before analysis using Burnard’s method (a structured approach to thematic content analysis) [6]. To enhance reliability, data were analysed by four researchers working independently (CB, HS, LS, AR). Emerging themes were discussed and agreed with all co-authors.
Ethical approval for the study was granted by the Dulwich branch of the National Research Ethics Service (NRES) Committee London (Ref 11/LO/1816).
Results and Discussion
16 children undergoing allergy testing were interviewed (age range 18 months to 13 years; 11 boys, 5 girls). For seven children (44%) it was their first contact with an outpatient allergy service. 15/16 parental interviews were with the mother. 7/9 children aged >8 agreed to be interviewed, but one later declined. Four parents (2P, 6P, 9P, 16P) had experience of their child having IgE and SPT allergy testing at some stage, and a fifth parent (4P) had experience of both tests in another child (Table 1).
| Child’s Age in Years, Gender (ID if interviewed) | Presenting Problem to Allergy Clinic | Previous Allergy Tests | Previous Venepuncture (not allergy-related) | Details of Parent Interviewed and ID | Most Recent Allergy Test |
|---|---|---|---|---|---|
| 12, Male (1C) | Eczema Peanut allergy Vomiting after cereal | SPT | Yes | Mother (39), play worker, 2 children (1P) | SPT |
| 7, Male | Review of multiple food allergies (including nuts and fish) | IgE | Yes | Mother (43), book keeper and cleaner (2P) | SPT |
| 18 months, Female | Peanut triggered rash and facial swelling | None | No | Mother, nutritional therapist, experience of being phlebotomist (3P) | SPT |
| 12, Male | Hay fever | None | Yes | Mother (32), hotelier, has daughter who has undergone IgE testing previously (4P) | SPT |
| 2, Female | Oral symptoms and wheeze on eating carrots and apples Severe eczema and facial swelling | None | Yes | Mother, 2 children, home maker (5P) | SPT |
| 10, Female (6C) | Review of nut and peanut allergy, rhinitis and asthma | SPT, IgE, patch tests | Yes | Mother, 45, home maker (6P) | SPT |
| 13, Male (7C) | Review of nut allergy | SPT | Yes | Mother, home maker (7P) | SPT |
| 3, Male | Known nut allergy, ‘bad reaction’ to playing with feather pillow | SPT | Yes | Mother, 3 year old twins and one other child, nurse (8P) | SPT |
| 8, Male (9C) | Review of longstanding nut allergy | None | No | Mother, 42, previously worked in pharmaceutical industry (9P) | SPT, IgE |
| 9, Female | Rash and breathing difficulties having stroked horse | None | Yes | Mother, home maker (10P) | SPT |
| 12, Male (11C) | Reacting to cashew containing fruit bars and curries | None | No | Father 49, town planner (11P) | SPT |
| 2, Male | Known egg allergy, started to point to mouth after eating peanuts | SPT | No | Mother, 39, accountant (12P) | SPT |
| 2, Male | Reacting badly to eggs | None | No | Mother 40, TV producer (13P) | SPT |
| 8, Male (14C) | Review of food allergy | SPT | Yes | Mother, 37, three children, Housewife (14P) | SPT |
| 2, Female | Review of cow’s milk protein and egg allergy | SPT | Yes | Mother, 31, Social worker (15P) | SPT |
| 8, Male | Review of allergic status (aeroallergens and food allergens (sesame, nuts)) | SPT and IgE | Yes | Mother, 40, hairdresser, three children (16P) | SPT |
Table 1: Participants (children and parents) and their characteristics
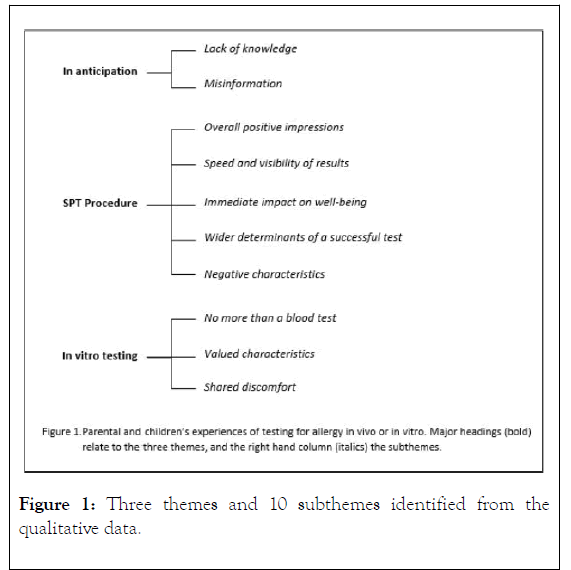
Three themes and 10 subthemes were identified from the qualitative data (Figure 1). The findings are illustrated with verbatim quotes.
Figure 1: Three themes and 10 subthemes identified from the qualitative data.
Lack of knowledge and unfamiliarity: Prior to their first outpatient visit parents and children recalled their poor awareness of allergy testing methods:
‘Neither of us knew what to expect, I didn’t know if they were going to put tiny little needles or what’ (4P)
‘Even with a strong family history of allergy, I actually didn’t know what to expect’ (13P)
When parents had some knowledge of allergy, the investigation they were familiar with was SPT:
‘SPT is the only type of allergy test I‘ve heard of and that’s what I assumed would be happening’ (10P)
Misinformation: Prior to their first allergy clinic appointment some children had gleaned misinformation about allergy testing from their peers:
‘…..She was a little bit nervous about the SPT because she had spoken to girls at school, her friends at school were all saying it really hurts, loads of blood comes out, you know you can imagine how it’s all exaggerated’ (10P)
Theme 2: Skin Prick Testing as a Largely Positive Experience
Overall positive impressions of SPT: Despite prior unfamiliarity with allergy testing modalities, parents recalled the SPT procedure accurately and in detail. They spoke spontaneously about many positive attributes of SPT, predominantly its speed (‘It’s really quick and easy’ (11P)) and minimal discomfort. Both parents and children reported the skin pricking process with words such as ‘ok’ or ‘comfortable’.
‘It didn’t hurt which was good. He didn’t even flinch actually, or cry, or anything’ (12P)
‘I had forgotten how quick it was, it was only 10 minutes or something wasn’t it. So the results were really quick’ (7P)
The visibility of SPT results was frequently commented upon; this was often linked with observations of how witnessing the reaction contributed to greater understanding:
‘I could see there were loads of [allergens]’ (1C)
Parents felt it was beneficial for their child to see their own reaction.
‘I think it’s quite good for children as well to see the different reactions ….It’s an obvious way of knowing there’s a reaction, I think that’s a good idea for [son] to notice there was a bad reaction to cashew…. And there wasn’t with other nuts’ (11P). The child also reflected these feelings ‘…you can actually understand what’s happening, and what and how that’s happening, and how bad the reaction is’ (11C).
Immediate impact on wellbeing: Having the SPT results within the same consultation meant lifestyle changes could be adopted immediately, reducing the risk of an allergic reaction.
It’s quite good you can start doing things without worrying about your allergy. Yeah, I recommend it’ (7C)
The ability of the SPT to offer diagnostic certainty and to inform future management exceeded expectations, whether confirming or excluding an allergy:
‘I didn’t know it would be that conclusive actually. I was expecting it to be quite inconclusive, ‘maybe he is, maybe he isn’t’, but they were very conclusive and said there’s absolutely no egg allergy showing up at all, which we were really pleased about’ (13P)
Wider determinants of a successful test: Parents recognised that it was not the test per se but also the environment and professionalism of staff which contributed to a successful skin prick testing experience.
‘The staff was very patient, he [nurse] explained what he was gonna do, and everything and X was quite, you know, relaxed by it all’ (1P)
Negative characteristics: The experiences of SPT process were not completely positive, there was a shift in vocabulary used when recounting the immediate test (pricking phase) to the development phase. More negative characteristics were experienced after the introduction of the allergens into the skin. Several children described how their arm became ‘uncomfortable’ or ‘itchy’, some found it ‘very painful’.
‘He said he barely felt it at all, I think he said it was afterwards as he started reacting to things that he was the most uncomfortable’ (4P)
The children talked about how challenging it was to resist scratching.
‘Well it was quite itchy and I was tempted to itch, but I wasn’t supposed to itch, so that was quite hard to try not to itch, but after it had gone down then it was fine’ (7C)
As well as this discomfort, which persisted in some for several hours, children also commented on the persistence over days of pen marks indicating the test site or outlining the responses on their forearms.
Respondents also discussed how age, co-morbidity (e.g., eczema) and allergenicity sometimes made SPT more difficult. The testing of a young, mobile and energetic child was perceived as problematic:
‘ ….It all takes a long time doesn’t it, you know because you have to, they have to be weighed and you have to see the doctor, and then have the test, and then see them again. And then see the doctor, so that’s all a bit tedious when they’re at that age, because they just want to run around’ (5P)
Some concerns were voiced by children previously diagnosed with an allergy who was undergoing further testing to ascertain persistence of their allergies:
‘It’s weird having, like knowing that I can never go near nuts and then you’ve got, like a nut on your arm, it’s a bit weird’ (6C)
The children did not vocalise their fears until returning home, but their behaviour was indicative of their concerns, for e.g.
‘She was crying and she sort of covered her arm and she just didn’t want it to happen…. And it was because she knew they; she was being retested for nuts again. And she had all her life, since she can remember, been told how important it was that she doesn’t go near nuts and she said ‘and then they were going to put it on my arm’ (6P). The mother said she wished she had the foresight to say ‘do you know that this is so minute.’
Theme 3: In-vitro Testing in Brief
No more than a blood test: In contrast to the SPT accounts, those of in vitro testing were very brief, focussing mostly on the venepuncture. No one mentioned what happened to the blood after collected, how it was prepared for testing or the purpose of the test.
Valued characteristics of in vitro testing: Characteristics valued included the familiarity of blood tests, its routine nature, and the speed of the procedure. Some parents recognised that a blood sample could be tested for a larger number of allergens as well as other markers of disease.
‘Use that one sample for various different things’ (12P)
Shared discomfort: Whilst the explanation of in vitro allergy testing process was brief and superficial, the process of venepuncture was described graphically, detailing discomfort from the needle and from restraint. Often parents recalled previous experiences of venepuncture in other settings, of clinicians having difficulty accessing a vein to emphasise the unpleasantness of the procedure and justify their childrens ’ dislike, ‘he remembers it to this day’. Parents also described their own discomfort observing venepuncture and ‘guilt’ restraining their child.
‘There were [six] four of us trying to keep him still to get the blood out of him. It was horrible, I will never forget it, I don’t think he will ever forget it’ (2P)
Some parents reported differing experiences of venepuncture depending on the child’s age.
‘it [venepuncture]was fine when she was really small, when she was new-born, you know but when she got to kind of, I don’t know about two months it was just awful’ (5P)
The children themselves were often more sanguine
‘Well at first, when I started having blood tests, I was kind of quite nervous ‘cause I had a very bad phobia of needles, but as I had more blood tests I wasn’t that afraid, cause I got used to it’ (7C)
Conclusion
Exploring parents’ and children’s experiences of allergy testing in open ended interviews demonstrated many positive views about SPT, including the immediacy of results, the opportunity to see the results, not having to come back for second appointments and SPT being less invasive than blood tests. In vitro allergy testing was valued for its convenience, speed, simplicity, the single puncture site rather than many lancet pricks, and no lasting discomfort or itchiness. Without any understanding of what happened to blood samples, in vitro testing was perceived as technically superior.
Strengths and Weaknesses of the Study
One previous study has explored the experiences of allergy testing in adults [3] but not in children and another explored the experiences of allergy testing for serious allergic disorders, but did not focus on the tests themselves [2]. Interviews produced rich information, the semi-structured approach enabled participants to discuss issues important to them. Sampling of parents continued until we had data saturation (when three consecutive interviews did not reveal any further themes). A systematic, fully documented approach to data analysis was undertaken by four researchers independently to minimise researcher bias. With its narrow aim, high specificity (participants had all recently undergone allergy testing) and the focused dialogue this study would be categorised as a qualitative study with high information power [7].
One limitation of our study is the small number of children interviewed. Children are the best source of data about themselves and children as young as three can recall events and give graphic descriptions [8]. However, working with younger children requires specialised skills and different techniques, such as prompts, drawing, role play and observation. For an exploratory study, we chose to rely on parents as proxy respondents for children below the age of eight, but further work is needed to better understand younger children ’ s experiences.
One limitation of our study is the small number of children interviewed. Children are the best source of data about themselves and children as young as three can recall events and give graphic descriptions [8]. However, working with younger children requires specialised skills and different techniques, such as prompts, drawing, role play and observation. For an exploratory study, we chose to rely on parents as proxy respondents for children below the age of eight, but further work is needed to better understand younger children ’ s experiences.
Implications for Clinical Practice
From participants’ accounts of testing we identified several areas for service improvement. The information provided with the outpatient appointment notification, asked for antihistamines to be discontinued but did not detail what would happen in clinic or the type of testing that might be undertaken. The lack of information fuelled misconceptions and heightened anxiety about attending allergy clinic. Children who already had confirmed food allergies, and instructed to avoid certain foods completely, were confused by the purposeful exposure to forbidden allergens for SPT. Having recognised this apparent anomaly they became distressed, but said nothing as testing went ahead. Whilst repeat testing with known allergens is routine in clinic, health professionals need to be attentive of lay perceptions of danger and address this in their pre-test briefing.
Blood testing
Parents did not know, or appear interested in what happened in in vitro allergy testing beyond taking the blood sample. This is consistent with an adult venepuncture study that found that blood tests were considered ordinary and unremarkable; something ‘they just do in hospitals’ [9]. It is accepted without questioning, and not perceived as worthy of discussion as it is everyday practice, and one which patients submit to by common consent: as de Certau [10] describes, it is the ‘law of the place’. However, parents spoke at length about the impact of venepuncture on their children, most linking the distress and fright to the needles and physical invasiveness of the procedure; fewer mentioned the sight of blood. Previous studies have similarly documented this emotional impact and physical invasiveness from the observations of nurses, parents and children [11,12]. In a study where children drew pictures of their experience of venepuncture, their images emphasised the size of the needle and syringe [13]. Despite several proven interventions that reduce the impact of venepuncture, such as topical anaesthesia, play therapy and distraction, it seems these are used less frequently than expected. The interpersonal skills of the clinical staff involved in skin prick testing was positively commented upon, but no such commendations related to venepuncture: this may reflect that staff feel venepuncture is so routine that they fail to recognise the need to reassure and explain fully to young patients and their parents.
This naturalistic study provides insight into childrens ’ and parents’ experiences and views of allergy testing. Several areas for improvement were identified, particularly more information about what will happen in clinic to reduce anxiety and misunderstandings. SPT with an already known allergen can cause concern as it appeared to contradict previous allergen avoidance instructions.
Acknowledgements
We would like to thank the parents and the children who participated in this study and the staff in the paediatric allergy clinic who assisted with the process of recruitment.
Author Contributions
Helen Smith and Christina J Jones were responsible for the conception and design of the study. Annalee Robertson and Laura Stuttaford were responsible for the acquisition of the data, recruiting and interviewing the respondents. All authors (Helen Smith, Clare Brown, Annalee Robertson, Laura Stuttaford, Rabia Rashid , and Christina J Jones) were involved in the data analysis, interpretation, and critical revision of the manuscript.
Funding
This study was funded by Brighton and Sussex Medical School Undergraduate Individual Research Project Funding.
REFERENCES
- Oppenheimer J, Durham S, Nelson H, Wolthers OD. Allergy diagnostic Testing. World Allergy Organization. 2014
- Burton C, Irshad T, Sheikh A. Understanding the experiences of allergy testing: a qualitative study of people with perceived serious allergic disorders. Postgrad Med J. 2010;86(1020):591-596.
- Brown CE, Jones CJ, Stuttaford L, Robertson A, Rashid RS, Smith HE. A qualitative study of the allergy testing experiences, views and preferences of adult patients. Clin Trans Allergy. 2016;6:34.
- Department of Health. Creating a Patient-led NHS: Delivering the NHS Improvement Plan. 2005
- Irwin RS, Richardson ND. Patient-focused care: Using the right tools. Chest. 2006;130(1):73S-82S.
- Burnard P. A method of analysing interview transcripts in qualitative research. Nurse Educ Today. 1991;11(6):461-466.
- Malterud K, Siersma VD, Guassora AD. Sample size in qualitiative interview studies: guided by information power. Qual Health Res. 2015;26(13).
- Docherty S, Sanelowski M. Focus on qualitative methods: Interviewing children. Res Nursing and Health. 1999;22(2):177-185.
- Pfeffer N, Laws S. ‘It's only a blood test’: What people know and think about venepuncture and blood. Soc Sci Med. 2006;62(12):3011-3023.
- De Certau M. The practice of everyday life. University of California Press, Berkley, USA. 2011.
- Davies PS, Collins DL, Gregory JR, Clarke PC. Parents’ and children’s reactions to taking blood in a nutrition survey. Arch Dis Child. 1996;5(4):309-313.
- Hands C, Round J, Thomas J. Evaluating venepuncture practice on a general children’s ward. Nursing Children and Young People. 2010;22(2):32-35.
- Hands C, Round J, Thomas J. “When someone stabs you”: children’s perspectives of venepuncture. Arch Dis Child. 2009;94(6):466.
Citation: Smith H, Brown C, Robertson A, Stuttaford L, Rashid R, Jones CJ (2019) The Experience of Being Tested for Allergies; the Views of Children and their Parents. J Allergy Ther 10:1.
Copyright: © 2019 Smith H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Sources of funding : This study was funded by Brighton and Sussex Medical School Undergraduate Individual Research Project Funding.