Indexed In
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Proquest Summons
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2022) Volume 13, Issue 2
Evidence of Pancytopenia, Secondary to Nutrition Deprived Vitamin B12 Deficiency in an Epileptic Child having Cerebral Palsy: A Rare Case Report
Dipa Saha1*, Richmond Ronald Gomes2, Chinmoy Kumar Saha3 and Kazi Selim Anwar42Department of Medicine, Ad-din Women’s Medical College Hospital (AWMCH), Dhaka, Bangladesh
3Department of Medicine, Cumilla Medical College Hospital, Dhaka, Bangladesh
4Department of Medicine, Ad-din Research Unit, Ad-din Women’s Medical College Hospital (AWMCH), Dhaka, Bangladesh
Received: 09-Feb-2022, Manuscript No. JBDT-22-15620; Editor assigned: 11-Feb-2022, Pre QC No. JBDT-22-15620 (PQ); Reviewed: 23-Feb-2022, QC No. JBDT-22-15620; Revised: 25-Feb-2022, Manuscript No. JBDT-22-15620 (R); Published: 02-Mar-2022, DOI: 10.4172/2155-9864.22.13. 488.
Abstract
Megaloblastic anemia and neurological manifestations are the hallmarks of Vitamin B12 deficiency. Pancytopenia is less frequently observed in vitamin B12 deficiency. We reported a case of 21-year-old boy with quadriplegic CP and epilepsy presented with poor feeding, generalized weakness and progressive pallor for 8 months. He was found to have Pancytopenia. Extensive workup revealed low vitamin B12 level secondary to nutritional deficiency. Vitamin B12 deficiency should be ruled out in all patients presenting with unexplained pancytopenia.
Keywords
Cerebral palsy; Pancytopenia; Epilepsy; Vitamin B12
Introduction
Megaloblastic anemia is rare but a known and treatable cause of pancytopenia that responds well to the treatment. Increased activity within bone marrow and defect in oxygenation to temperature regulatory area are proposed mechanisms. Easy availability and low cost of peripheral blood smear helps in screening these patients at an early stage. After measurement of Vitamin B12 and folic acid levels, a trial of treatment based on these results can cause a rapid response and obviate the need further investigations and unnecessary antibiotic use.
Case Report
A 21 years old boy came to our hospital for generalized weakness, poor feeding and progressive pallor for 8 months. He was a 2nd issue of non-consanguineous parents, had asphyxiated birth after normal vaginal delivery with delayed developmental milestone predominantly motor delay. He was unable to stand yet. Since his 4 months of age he had recurrent focal to bilateral tonic clonic seizure, initially occurred 2-3 times/day and treated with inadequate doses of different anti-epileptic drugs. For the last 12 years he took Carbamazepine (10 mg/kg/day), Clonazepam and Topiramate (3 mg/kg/day). And still he had seizures occurring 3-4 times/month. Along with this he had behavioral abnormality, aggressiveness, and visual impairment. For the last 8 months he took inadequate diet due to poor appetite and developed generalized weakness and progressive pallor. He had no history of feeding and swallowing difficulty. Any involuntary movement and bleeding manifestation was absent. On admission, the patient was drowsy and confused. He was afebrile, pulse: 66/min, BP: 110/60 mmHg, weight: 80 kg, had microcephaly (OFC: 47 cm). He was severely pale. There were no lymphadenopathy, bleeding spots and organomegaly but had knuckle hyperpigmentation. Neurological examination showed impaired higher psychic function, restlessness and poor communication. Slurred speech with spastic quadriplegia was noted. Extensor plantar responses and clonus were present bilaterally. Fundal examination and tests for proprioception and vibration sense could not be performed as the patient was not cooperative.
Investigation
CBC showed pancytopaenia (haemoglobin 3.2 g/dl; total count be 1540 cells/mm ; platelets 16,000 cells/mm ), HCT-9.9%, MCV-93.4fL, MCH-30.2pg, MCHC-32.3 g/dl, RDW-22.1%. Peripheral blood film shows dimorphic red cell (macrocyte and microcyte) with few tear drop cell and eliptocyte, WBCs were mature, total and differential count were within normal limit, neutrophil showed hyper segmentation, platelets were reduced suggestive of combined deficiency anemia with thrombocytopenia, reticulocyte count was low normal (1.08%). Iron profile was normal (S. Ferritin-95.74 ng/ml, S. Iron-220.23 microg/dl, S. TIBC-246.90 microg/dl). LDH level was high (1710 U/L). There was dyselectrolytaemia (sodium 136 mEq/l; potassium 2.95 mEq/l; calcium 8 mg/dl; serum magnesium: 2.1 mg/dl; serum albumin: 3.4 g/dl). Direct coombs test was negative. Blood sugars performed at admission and repeated over the course of hospital stay were normal. Further work-up for the cause of pancytopaenia revealed low serum vitamin B12 levels (149 pg/ml) and normal serum Folate level. Metabolic workup showed normal serum methylmelonic acid and urine homocystine level. EEG was abnormal showing focal epileptiform discharge from left fronto temporal region suggestive of seizure disorder of focal origin. MRI showed encephalomalacic change in left fronto parietal region. After admission, patient was treated with intramuscular cyanocobalamin 1 mg every alternate day for 6 doses along with blood transfusion followed by oral vitamin supplementation. During treatment with cyanocobalamin he developed hypokalemia which was managed accordingly. Repeat CBC was done which was found normal. There is a plan to continue intramuscular cyanocobalamin every three monthly life long and follow him with regular complete blood count on an outpatient door basis.
Results and Discussion
Pancytopenia is diagnosed when there is a reduction in all three hematopoetic cell lines. This is seen as reduction in the white cell count, hemoglobin, and platelet count [1,2]. The evaluation of a patient with pancytopenia requires a comprehensive approach and identifying the underlying cause can be challenging given the wide range of etiologies including drugs, autoimmune conditions, malignancies, infections, hemophagocytosis, and inheritable conditions [3].
The basic pathophysiology of pancytopenia is impaired cell production due to bone marrow failure and marrow infiltration problems, peripheral destruction of distinct cell lines for hypersplenism or a combination of these. Hematological study can differentiate these three processes, but the crucial first steps of evaluation must include thorough history, physical examination, complete blood count, peripheral blood smear, reticulocyte count. Pancytopenia along with macrocyte in peripheral film is commonly found in megaloblastic anemia, aplastic anemia and myelodysplastic syndrome. These conditions can be differentiated by doing reticulocyte count, LDH level.
Our patient had pancytopenia with increased MCV (macrocyte), low normal reticulocyte count and increased LDH which virtually exclude aplastic anemia. In aplastic anemia the peripheral blood smear may show macrocytic red blood cells but the absolute reticulocytes are reduced and sometimes totally absent. So antiepileptic drug induced aplastic anemia is unlikely for this case. Myelodysplastic syndrome is a clonal stem cell disorder characterized by dysplastic bone marrow. It usually affects people over the age of 65 with a male predominance [3], however, chemotherapy related MDS can occur at any age. The peripheral blood smear may show PelgerHuet – like abnormal neutrophil [3].
Pancytopenia is a rare manifestation of vitamin B12 deficiency [3]. Folate and vitamin B12 deficiencies can cause megaloblastic anemia, thesemight present with pancytopenia as well [4]. In one Indian study of 201 patients with documented cobalamin (Vit B12) deficiency, two-thirds of patients showed hematologic abnormalities. Macrocytosis was the most commonly observed finding (54%), followed by anemia (37%), hypersegmented neutrophils (32%), leukopenia (13.9%), and thrombocytopenia (9.9%). Pancytopenia was seen in 5% of patients and hemolytic anemia in 1.5% [5]. Vit B12 (Cobalamine; Cbl) is required for the hematopoietic cell formation and an important cofactor involved in the synthesis of the DNA, fatty acids, and myelin. Inadequate intake of it with diet, malabsorption, autoimmune and metabolic diseases causes Vitamin B12 deficiency [6]. Pancytopenia occurs in cases of severe vitamin B12 deficiency that are sustained over time. The mechanism of the cytopenias is defective DNA synthesis [7]. While all hematopoietic cell lines are affected, the impact on erythrocytes is greatest. Thrombocytopenia is usually due to ineffective platelet production.Cobalamin deficiency leads to deformity of the Red Blood Cell (RBC) membrane as well as hyperhomocysteinemia promoting endothelial dysfunction [8-10]. In both intramedullary and extramedullary hemolysis, serum LDH levels will be high while haptoglobin levels will be low. In pseudothromboticmicroangiopathy, the reticulocyte count should be low.
Cynthia et al. [11] reported a case of 2 years old girl with pancytopenia due to Vit B12 deficiency, who presented with only feature of progressive pallor. They found a homozygous mutation of the amnionless gene (AMN) as an underlying etiology of Vit B12 deficiency. Megaloblastic anemia and neurological manifestations are the hallmarks of Cobalamine (Cbl) deficiency. Cobalamine acts as an important cofactor (adenosylcobalamin) for the conversion of Methylmalonyl CoA to succinyl CoA, recycling of homocystine to methionine and fatty acid metabolism as well as play a crucial role in myelination. Clinically patient may have apathy, anorexia, developmental regression, metabolic decompensation, coma, myelopathy, peripheral neuropathy, optic atrophy [12]. Our patient was quariplagic CP with epilepsy. So we initially thought whether it could be inborn error of vit B12 metabolism. He had low Vit B12 level but MMA level and urine Homocystine level were normal. His dietary history revealed inadequate food intake for last 1 year. He had no feature of autoimmune disease (rash, arthritis). So it could be assumed that his pancytopenia was due to nutritional Vit B12 deficiency. Naha et al. [13] reported a case with recurrent generalized seizure due to Vit B12 deficiency. Akaike et al. [14] demonstrated that demyelinated neurons are more susceptible to the excitatory effects of glutamate, providing a link between demyelination and the development of seizures. B12 deficiency can elevate serum folate levels via the methyl-folate trap, and that all folate derivatives are highly epileptogenic that is hypothesized by Reynolds (Figure 1 ) [15].
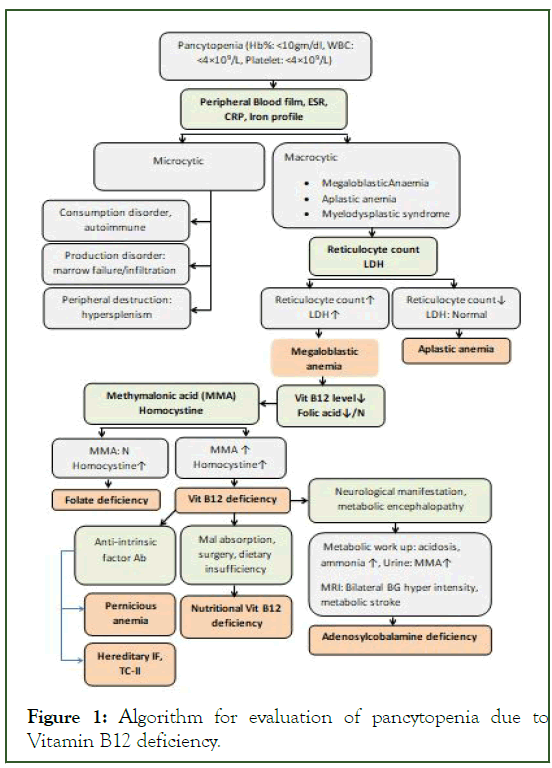
Figure 1: Algorithm for evaluation of pancytopenia due to Vitamin B12 deficiency.
Conclusion
Children with epilepsy should be screened for Vitamin B12 level specially if presented with pancytopenia. If nutritional deficiency was excluded from history and by investigation, metabolic work up and genetic testing should be advised.
REFERENCES
- Young NS. Aplastic anemia, myelodysplasia, and related bone marrow failure syndromes. Harrisons Principles of Internal Medicine. 2005; 16(1):617.
- Guinan EC. Acquired and inherited aplastic anemia syndromes. Wintrobe's Clinical Hematology. 2004:1396-1419.
- Premkumar M, Gupta N, Singh T, Velpandian T. Cobalamin and folic acid status in relation to the etiopathogenesis of pancytopenia in adults at a tertiary care centre in North India. Anemia. 2012; 2012.
[cross ref] [google scholar] [pubmed]
- Gnanaraj J, Parnes A, Francis CW, Go RS, Takemoto CM, Hashmi SK. Approach to pancytopenia: Diagnostic algorithm for clinical hematologists. Blood Rev. 2018; 32(5):361-367.
[cross ref] [google scholar] [pubmed]
- Andres E, Affenberger S, Zimmer J, Vinzio S, Grosu D, Pistol G, et al. Current hematological findings in cobalamin deficiency. A study of 201 consecutive patients with documented cobalamin deficiency. Clin Lab Haematol. 2006; 28(1):50-56.
[cross ref] [google scholar] [pubmed]
- Ankar A, Kumar A. Vitamin B12 deficiency (cobalamin). 2020.
- Wadood Khan ZA, Vidyasagar S, Bekur R, Belurkars S, Shailaja S. Subhyaloid haemorrhage in a patient with vitamin B12 deficiency: A unique presentation. J Clin Sci Res. 2013; 2:161-164.
- Malla M, Seetharam M. To treat or not to treat: A rare case of pseudo‐thrombotic thrombocytopenic purpura in a Jehovah's Witness. Transfusion. 2016; 56(1):160-163.
[cross ref] [google scholar] [pubmed]
- Tuten N, Bennett C, Babcock W. Thrombotic thrombocytopenic purpura or cobalamin deficiency? A case report and review. Clin Case Rep Rev. 2015; 1(8):157-159.
- Acharya U, Gau JT, Horvath W, Ventura P, Hsueh CT, Carlsen W. Hemolysis and hyperhomocysteinemia caused by cobalamin deficiency: Three case reports and review of the literature. J Hematol Oncol. 2008; 1(1):1-5.
[google scholar] [pubmed]
- Ho CH, Thomas M, McGuire E, Yano S. 2-Year-old girl with pancytopenia due to vitamin B12 (cobalamin) deficiency. J Paediatr Child Health. 2014; 50(11):926-928.
[google scholar] [pubmed]
- Demir N, Koc A, Ustyol L, Peker E, Abuhandan M. Clinical and neurological findings of severe vitamin B12 deficiency in infancy and importance of early diagnosis and treatment. J Paediatr Child Health. 2013; 49(10):820-824.
[cross ref] [google scholar] [pubmed]
- Naha K, Dasari S, Vivek G, Prabhu M. Vitamin B12 deficiency: An unusual cause for recurrent generalised seizures with pancytopaenia. Case Rep. 2012; 2012:bcr2012006632.
[cross ref] [google scholar] [pubmed]
- Akaike A, Tamura Y, Sato Y, Yokota T. Protective effects of a vitamin B12 analog, methylcobalamin, against glutamate cytotoxicity in cultured cortical neurons. Eur J Pharmacol. 1993; 241(1):1-6.
[cross ref] [google scholar] [pubmed]
- Reynolds E. Vitamin B12, folic acid, and the nervous system. The lancet neurology. 2006; 5(11):949-960.
[cross ref] [google scholar] [pubmed]
Citation: Saha D, Gomes RR, Saha CK, Anwar KS (2022) Evidence of Pancytopenia, Secondary to Nutrition Deprived Vitamin B12 Deficiency in an Epileptic Child having Cerebral Palsy: A Rare Case Report. J Blood Disord Transfus. 13: 488.
Copyright: © 2022 Saha D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

