Indexed In
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2025) Volume 9, Issue 1
The Effectiveness of Septal Ablation versus Septal Myectomy on Survival for Patients with Hypertrophic Cardiomyopathy
Priya Sharma*Received: 03-Jan-2020, Manuscript No. JSA-24-3049; Editor assigned: 08-Jan-2020, Pre QC No. JSA-24-3049 (PQ); Reviewed: 22-Jan-2020, QC No. JSA-24-3049; Revised: 15-Jul-2024, Manuscript No. JSA-24-3049 (R); Published: 31-Mar-2025, DOI: 10.35248/2684-1606.24.8.255
Abstract
Background: Hypertrophic cardiomyopathy is an autosomal dominant condition affecting males and females across all ages and ethnicities. This condition results in the thickening of the heart’s myocardium, leading to reduced cardiac output, with subsequent complications including heart arrhythmias and Sudden Cardiac Death (SCD). Currently, septal myectomy, a type of open heart surgery, continues to be the gold standard treatment for reducing the Left Ventricular Outflow Tract (LVOT) obstruction. However, in recent years, septal ablation has emerged as a newer, less invasive procedure which aims to obliterate the obstruction via injection of alcohol into the hypertrophied septum.
Objectives: The aim of this systematic literature review is to establish whether septal myectomy or septal ablation is more effective in prolonging survival in hypertrophic cardiomyopathy patients.
Methodology: The methods used in this research were in accordance to a systematic literature review. The databases: PubMed, Cochrane and Scopus were utilised to extract relevant studies to further analyse and then to critically appraise using CASP tools.
Key findings: All studies included in this systematic literature review appreciated that the effects of septal myectomy and septal ablation were comparable, to an extent, when assessing clinical outcomes and survival for hypertrophic cardiomyopathy patients.
Conclusion: Despite septal ablation being a more advanced and minimally invasive procedure with optimistic clinical outcomes, septal myectomy remains superior due to its long-term relief from symptoms and increased likelihood of survival.
Keywords
Hypertrophic cardiomyopathy; Septal myectomy; Septal ablation; Hypertrophied septum
Introduction
Background
Hypertrophic cardiomyopathy is a cardiovascular disease which can affect both males and females across all ages and ethnicities. The condition results in the myocardium of the ventricular walls of the heart becoming hypertrophic due to an increase in the size of myocytes. The myocardium is the middle-layer of the wall of the heart which is collected of cardiac muscle fibres that enable contractility.
Patients who suffer from the disease are at risk of several complications, namely heart failure, sudden cardiac death and atrial fibrillation which increases the risk of an embolic stroke.
Pathophysiology
Hypertrophic cardiomyopathy results in asymmetrical thickening of the myocardium and a range of patterns of left ventricular wall hypertrophy exist. Due to the walls of the ventricles becoming thick/stiff, they do not relax to a sufficient degree, meaning they cannot fill with blood, consequently this reduces cardiac output.
Hypertrophic cardiomyopathy is inherited in an autosomal dominant approach, meaning that one of the alleles is faulty; it is most commonly caused by a mutation in one of 12 genes which encode various thick and thin myofilament constituents of the sarcomere. The mutations in hypertrophic cardiomyopathy are linked to a predisposition in the modification of cardiac contractility and animal studies on mice and rabbits have exhibited that the effects of mutations in genes, which are also present in humans, cause increased fibrosis and hypertrophy of cardiac muscle.
One of the mutations for familial hypertrophic cardiomyopathy is in exon 13 of the beta cardiac myosin heavy chain. The genes that are most frequently affected are the myosin-binding protein C as well as the β myosin heavy chain. Most cases in younger patients are associated with congenital syndromes, metabolic conditions and neuromuscular diseases. In adults, however, having hypertrophic cardiomyopathy is linked to familial diseases [1].
Materials and Methods
Treatments
The goal of treating hypertrophic cardiomyopathy is to obliterate LVOT obstruction. This obstruction can cause symptoms of heart failure and reduce survival. Medical therapy is used as a first-line treatment; beta blockers, for example propanolol are used for symptomatic LVOT obstruction.
If there is initial treatment failure after the use of drugs and there is sub-aortic obstruction, then the options for treatment are either alcohol septal ablation or septal myectomy.
Septal myectomy, which is the current gold standard treatment for hypertrophic cardiomyopathy, is an open-heart surgery where excess muscle from the hypertrophic septum is removed to reduce LVOT obstruction. It is known that patients experience swift relief from their symptoms post-procedure. Despite the benefits of septal myectomy, there are some drawbacks, including the fact that patients who are elderly or have multiple co-morbidities are not eligible for the treatment due to periprocedural risks, such as infection and arrhythmias. Due to these reasons, septal ablation, a newer treatment used to eradicate the LVOT obstruction can be employed in its place.
Septal ablation, which was originally introduced in 1994, is a negligibly invasive modality for the treatment of hypertrophic obstructive cardiomyopathy. The procedure works by injecting alcohol into the septal perforator which allows for an infarction of the hypertrophic septum to take place, this reduces the thickening of the septum and eliminates the LVOT obstruction. Similar to septal myectomy, there are complications associated with this procedure, for example heart blocks and the need for reintervention.
The MeSH (Medical Subject Headings) search was then conducted. A MeSH search is a way of searching synonyms or alternate forms of individual terms or phrases in a question. In this systematic review, it applied to the individual PICO terms. The results of the MeSH search can be seen in Table 1.
| Population | Intervention | Comparator | Outcome |
|---|---|---|---|
| Patients with hypertrophic cardiomyopathy | Septal ablation | Septal myectomy | Effectiveness on survival |
| Hypertrophic cardiomyopathy | Septal ablation | Septal myectomy | Effectiveness on survival |
| Cardiomyopathies, hypertrophic | Alcohol septal ablation | Myectomy, septal | |
| Hypertrophic cardiomyopathies | Ablation, septal | ||
| Cardiomyopathy, hypertrophic obstructive | |||
| Cardiomyopathies, hypertrophic obstructive | |||
| Hypertrophic obstructive cardiomyopathies | |||
| Hypertrophic obstructive cardiomyopathy | |||
| Obstructive cardiomyopathies, hypertrophic | |||
| Obstructive cardiomyopathy, hypertrophic |
Table 1: MeSH terms obtained from a PubMed MeSH search.
The next stage of the systematic review was to conduct a boolean search from the MeSH terms that had been obtained. A boolean search is a type of advanced search which allows for the combination of keywords with the use of operators such as ‘AND’ and ‘OR’ to broaden relevant search results and to make them more specific to the topic of interest. The boolean search terms and number of results across all the chosen databases can be seen in appendix A [2].
Inclusion and exclusion criteria
Once the keywords had all been combined using the boolean operators and the search results had been obtained, limitations/ inclusion criteria and exclusion criteria available on the databases, as seen in Table 2, were set to narrow down the results further to make them more specific to the relevant treatments for hypertrophic cardiomyopathy.
| Inclusion criteria/limitations | Exclusion criteria |
|---|---|
| Clinical trials | Systematic reviews |
| Clinical studies | Meta-analyses |
| Comparative studies | Articles not in English |
| Controlled clinical trials | Articles older than 10 years (older than 2009) |
| Multicentre studies | |
| Observational studies | |
| Pragmatic clinical trials | |
| Human species | |
| English language | |
| Articles published within the last 10 years (2009-2019) |
Table 2: Inclusion criteria/limitations and exclusion criteria.
Results
Screening and data extraction
Results from the searches were screened to check for their eligibility in the systematic review. The screening of the results can be seen in the PRISMA flow diagram in Figure 1.
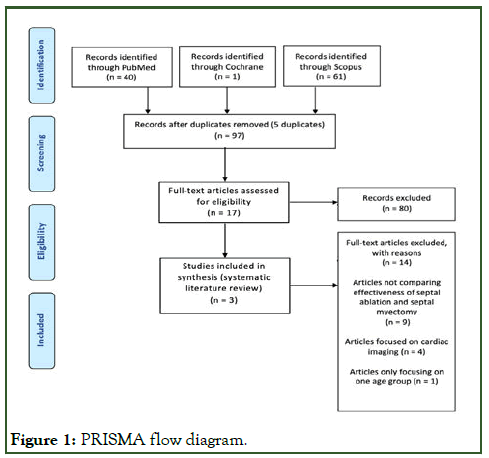
Figure 1: PRISMA flow diagram.
Summary of studies
The methods across all three studies were very similar; as expected with this type of condition and its treatments, they were all non-randomised, observational studies. Studies A and B carried out the procedures many years ago compared with study C which carried out the treatments recently from 2011 to 2015, meaning there could have been differences in how the treatments were performed, affecting the results. All studies had a set of baseline characteristics for the patients that they were going to include, studies A and B chose a similar number of males and females, study C had more males in the study overall and so more male patients were allocated to both septal ablation and septal myectomy. Across all three studies, the age groups for septal ablation were higher than those for septal myectomy, this may have affected the survival rates and clinical outcomes. The sample sizes for studies A and C were relatively reasonable at 263 patients and 226 patients, respectively, however study B had a far superior sample size at 574 patients for the ablation and myectomy groups [3].
Graphs reflecting survival
Figure 2 depicts the percentages of annual cardiac death and periprocedural death from both septal ablation and septal myectomy in study A. The percentage of both annual cardiac death and periprocedural death was lower in alcohol septal ablation, with 0.7% and 1.2%, respectively.
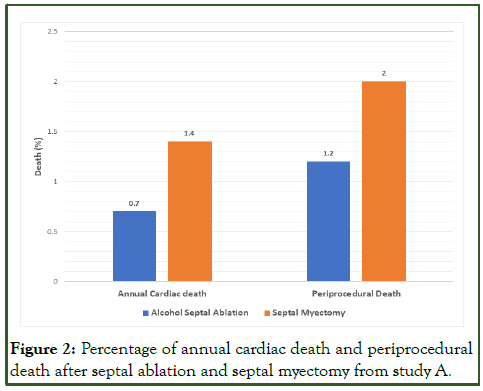
Figure 2: Percentage of annual cardiac death and periprocedural death after septal ablation and septal myectomy from study A.
Figure 3 depicts the differences between 5 and 10-year survival rates after undergoing each of the treatments; it can be seen that septal ablation and septal myectomy had similar 5-year survival rates, at 91% and 92%, respectively. The 10-year survival rates for the treatments did contrast slightly, with septal myectomy having a slightly higher percentage at 85% compared to septal ablation which had a percentage of survival of 82%.
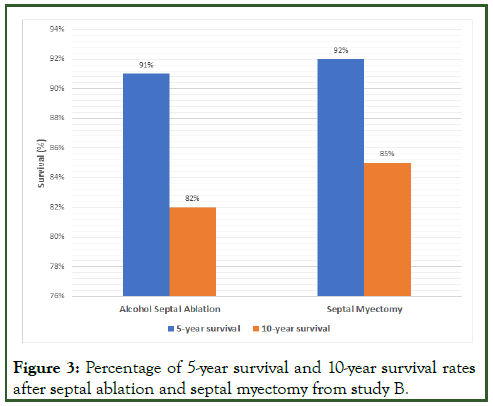
Figure 3: Percentage of 5-year survival and 10-year survival rates after septal ablation and septal myectomy from study B.
Figure 4 illustrates the differentiation between post-procedure and late mortality, post-procedural mortality was higher in septal ablation at 2.94% compared to septal myectomy which had a mortality rate of 1.27%. Late mortality reduced at 1.47% for septal ablation and stayed the same at 1.27% for septal myectomy, consistently being lower than ablation [4].
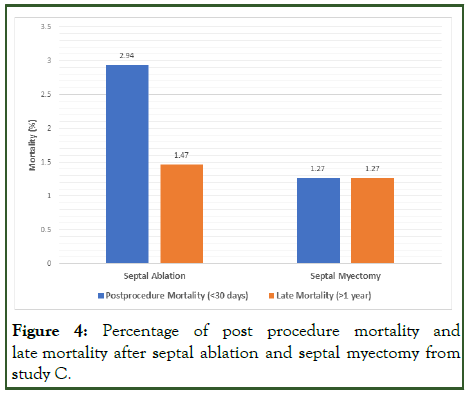
Figure 4: Percentage of post procedure mortality and late mortality after septal ablation and septal myectomy from study C.
Above, Figure 5 represents the comparisons of the median measurements of LVOT gradients before and after the patients had undergone both treatments. Before the treatments, the median LVOT gradient of the septal ablation group was 32 mm Hg and the LVOT gradient for the septal myectomy group was 50 mm Hg.
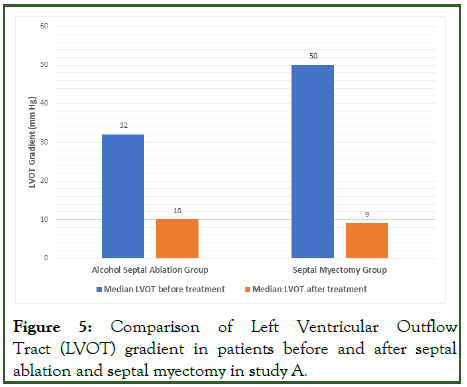
Figure 5: Comparison of Left Ventricular Outflow Tract (LVOT) gradient in patients before and after septal ablation and septal myectomy in study A.
After being exposed to the treatment, the LVOT gradient in the septal ablation group reduced by 22 mm Hg, going down to 10 mm Hg and the gradient in the septal myectomy group dropped the greatest, by 41 mm Hg, going down to 9 mm Hg [5].
Critical appraisal summary
For this systematic review, all the studies were of an observational/cohort nature and so the cohort study CASP tool was utilised (the complete CASP tool results can be seen in appendix B).
In general, all papers were of good quality as they can have implications in practice and be applied to the local population. Study A was superior than the others, study B was a good paper with the only drawbacks being the duration of the followup period and the slight bias from patients being recruited from tertiary referral centres. Study C was the weakest with the shortest follow up period, meaning the results would not have been as reliable as the results from studies A and B. The confidence interval was also not provided in study C, meaning the precision of the results could not be assessed. Therefore, studies A and B were of good quality and study C was of satisfactory quality [6].
Discussion
Rationale
This systematic literature review aimed to explore the effectiveness of septal ablation versus septal myectomy in relation to survival for patients suffering with hypertrophic cardiomyopathy, in order to establish which treatment would be better for prolonging the life of patients. A systematic literature review on this topic is important as there is a lack of ample literature comparing the effectiveness of septal ablation and septal myectomy on survival. Collating this information from different studies would be beneficial to both healthcare professionals and patients; healthcare professionals such as doctors and physician associates would profit from this evidence as it would aid them in deciding which treatment would be better suited to individual patients to maintain patient-centred care. This information can then be relayed onto patients to help them remain autonomous when choosing their desired treatment [7].
Main findings
All three papers could come to a generalised conclusion based on their results. Studies A and C analysed the LVOT gradient before and after both treatments (Figure 5 shows the LVOT gradient measured in study A). The gradient in both studies was lowest after septal myectomy (10 mm Hg post-procedure in study A and 13.95 mm Hg ± 9.94 mm Hg post-procedure in study C). A high LVOT gradient results in greater obstruction and has been correlated with an amplified risk of Sudden Cardiac Death (SCD), severe heart failure and a lower survival rate. This can be supported by a single-center study which found that septal ablation had a higher rate of sudden cardiac death. On the other hand, a study by Spaziano, Sawaya and Lefvre showed that the 5 and 10-year survival rate for septal ablation was 94.1% and 86.9%, respectively, which is analogous to the septal myectomy 5 and 10-year survival rates shown in Figure 3 of 92% and 85%, respectively [8].
The studies investigated mortality rates after follow-up, cardiac death was higher after myectomy compared to ablation in study A, seen in Figure 2, at 1.4%, conversely study C found late mortality after myectomy was lower than ablation, seen in Figure 4, at 1.27% and 1.47%, respectively. The rate of annual SCD in study B was measured and found myectomy to have a lower frequency at 0.8% per year. This figure is considerably lower than the rate of annual SCD without treatment, which a study conducted in 2007 found to be 4.3% in a non-myectomy group.
In terms of assessing mortality/survival alone, all the studies highlighted that both septal ablation and septal myectomy were mostly comparable with the mortality and survival rates being similar. To support this, current literature has discovered that post-procedural and late mortality rates between both treatment groups are low, however septal ablation has required a higher need for re-intervention due to complications [9].
Significance and implications
The results from the studies are significant to the extent that they reinforce what is currently known about the area. The focus of this systematic literature review is on which treatment would be more effective in relation to survival and other studies have found that long-term SCD and mortality rates were comparable. Another aspect which has been strengthened is that ablation remains secondary to myectomy due to the increasing need for reintervention post-procedure.
The results can be implicated in practice as the evidence demonstrates that both treatments are effective in relieving the outflow tract obstruction and subsequently improving survival, however myectomy improves the LVOT gradient the greatest and so will remain the preferred treatment. However, septal myectomy requires great surgical knowledge and so is not widely available in all centres and so patients would benefit from knowing about the advantages of septal ablation [10].
Limitations
Sample size plays a vast factor in assessing the reliability and representability of the results. The sample sizes in the three papers were small considering that the condition affects 1 in 500 people in the entire population. The sample sizes for the papers were in the hundreds, meaning the results may not have been as precise and generalizable to the population. A larger sample size (at least over a thousand patients) would have solved this problem.
Study A had a respectable period of 11 years, however studies B and C had a shorter follow-up duration meaning the results may not have been complete enough to apply into practice. A longer duration would increase the usefulness of the research and review any new changes.
Despite the limitations, the CASP summary displays that studies A and B were of good quality, whereas study C was satisfactory [11].
Additionally, a limitation in this systematic review included a lack of searches on various databases; only three databases were used to search literature. Using more databases such as MEDLINE and Embase may have expanded search results, meaning more than three relevant papers may have been found to make the results and conclusion stronger. On the other hand, using databases such as PubMed and Cochrane in this systematic review would be a strength as they contain a wide range of literature and have several inclusion and exclusion criteria, which helps to narrow down the results to make them specific to the topic.
Further research
Added studies, similar to the ones analysed in this systematic review, would have to take place to make the results more reliable and representative and this reliability could be elevated by having larger sample sizes in future observational studies. Additional research being carried out in England would also be valuable as having knowledge about the outcomes from studies in this country would increase the applicability of the results in the NHS [12].
Conclusion
A systematic literature review was performed to ascertain the effectiveness in relation to survival of septal ablation versus septal myectomy on patients with hypertrophic cardiomyopathy. PubMed, Cochrane and Scopus were the selected databases utilised for the literature searches, from which three studies were chosen and further explored.
Analysis of the literature determined that both septal ablation and septal myectomy yield positive clinical outcomes in terms of improving survival rates in patients with hypertrophic cardiomyopathy. Nevertheless, it is recognised that septal myectomy will remain the gold standard treatment due to its rapidity in liberating symptoms and greater clinical outcomes in comparison with septal ablation. The findings of this systematic literature review may be implemented in practice and used in further research. Though, considering that septal ablation is a relatively new treatment and has not been applied in practice to the extent that septal myectomy has, further research is required to solidify this debate.
Conflicts of Interest
No conflicts of interest.
Ethical Approval
No ethical approval was required.
References
- Biau DJ, Kerneis S, Porcher R. Statistics in brief: The importance of sample size in the planning and interpretation of medical research. Clin Orthop Relat Res. 2008;466(9):2282-2288.
[Crossref] [Google Scholar] [PubMed]
- Davies MJ. The cardiomyopathies: An overview. Heart. 2000;83(4):469-474.
[Crossref] [Google Scholar] [PubMed]
- Elliott P, McKenna WJ. Hypertrophic cardiomyopathy. Lancet. 2004;363(9424):1881-1891.
[Crossref] [Google Scholar] [PubMed]
- Geisterfer-Lowrance AA, Kass S, Tanigawa G, Vosberg HP, McKenna W, Seidman CE, et al. A molecular basis for familial hypertrophic cardiomyopathy: A β cardiac myosin heavy chain gene missense mutation. Cell. 1990;62(5):999-1006.
[Crossref] [Google Scholar] [PubMed]
- Guo HC, Li JH, Jiang TY, Ren CW, Dai J, Zhou YJ, et al. Comparison of clinical effects between percutaneous transluminal septal myocardial ablation and modified morrow septal myectomy on patients with hypertrophic cardiomyopathy. Chin Med J. 2018;131(05):527-531.
[Crossref] [Google Scholar] [PubMed]
- Houston BA, Stevens GR. Hypertrophic cardiomyopathy: A review. Clin Med Insights Cardiol. 2014;8:CMC-S15717.
[Crossref] [Google Scholar] [PubMed]
- Jacoby DL, dePasquale EC, McKenna WJ. Hypertrophic cardiomyopathy: Diagnosis, risk stratification and treatment. CMAJ. 2013;185(2):127-134.
[Crossref] [Google Scholar] [PubMed]
- Sorajja P, Valeti U, Nishimura RA, Ommen SR, Rihal CS, Gersh BJ, et al. Outcome of alcohol septal ablation for obstructive hypertrophic cardiomyopathy. Circulation. 2008;118(2):131-139.
[Crossref] [Google Scholar] [PubMed]
- Maron BJ, Ommen SR, Semsarian C, Spirito P, Olivotto I, Maron MS. Hypertrophic cardiomyopathy: Present and future, with translation into contemporary cardiovascular medicine. J Am Coll Cardiol. 2014;64(1):83-99.
[Crossref] [Google Scholar] [PubMed]
- Maron BJ, Nishimura RA. Surgical septal myectomy versus alcohol septal ablation: Assessing the status of the controversy in 2014. Circulation. 2014;130(18):1617-1624.
[Crossref] [Google Scholar] [PubMed]
- Alam M, Dokainish H, Lakkis N. Alcohol septal ablation for hypertrophic obstructive cardiomyopathy: A systematic review of published studies. J Interv Cardiol. 2006;19(4):319-327.
[Crossref] [Google Scholar] [PubMed]
- Nagueh SF, Groves BM, Schwartz L, Smith KM, Wang A, Bach RG, et al. Alcohol septal ablation for the treatment of hypertrophic obstructive cardiomyopathy: A multicenter north American registry. J Am Coll Cardiol. 2011;58(22):2322-2328.
[Crossref] [Google Scholar] [PubMed]
Citation: Sharma P (2024) The Effectiveness of Septal Ablation versus Septal Myectomy on Survival for Patients with Hypertrophic Cardiomyopathy. J Surg Anesth. 8:255.
Copyright: © 2024 Sharma P. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
