Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- ResearchBible
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Proquest Summons
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- MIAR
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2023) Volume 14, Issue 6
The Effect of Psychoactive Substances used on Clinical Outcomes in Injured Drivers Referred to Emergency Medicine: Case-Control Study
Nader Tavakoli1, Zahra Mousavi2, Alireza Amanollahi1 and Tannaz Babeveynezhad2*2Department of Pharmaceutical Sciences, Tehran Azad University, Tehran, Iran
Received: 17-Nov-2023, Manuscript No. JPP-23-23934; Editor assigned: 22-Nov-2023, Pre QC No. JPP-23-23934 (PQ); Reviewed: 07-Dec-2023, QC No. JPP-23-23934 ; Revised: 15-Dec-2023, Manuscript No. JPP-23-23934 (R); Published: 22-Dec-2023, DOI: 10.35248/2153-0645.23.14.072
Abstract
Objective: The use of psychoactive substances increases the risk of accidents. This study evaluated the relationship between the type of psychoactive substances among traffic injured admitted to the medical center.
Methods: Injured drivers (100 used drugs), (260 control group), who were transferred to 7-Tir Hospital from April 2021 to March 2022 were studied. The information related to the accident scene, personal characteristics, and the substance used was collected from the police and the medical center documents. We used multiple logistic regressions to find the important factor in outcomes.
Results: The mean age of the case group (37.49 ± 13.61) compared to the control group (34.18 ± 14.05) was significant (p=0.044). The most common substances in the case group were opioids which had the highest mean age (41.90 ± 13.541). Injured who used sedatives had higher signs of head trauma than the others. Also, being guilty had a remarkable difference in the groups (94.6 vs. 62.4 p=<0.001). Motorcyclist drivers were 185(65%) as responsible for the accident, in addition, 69(69%) were in the case group. Head trauma, type of accident, and level of triage had a significant effect on the death of the injured.
Conclusion: These are using sedatives causes increased head trauma. Driving under the effect of psychoactive drugs is more common among motorcycle drivers, and a large percentage of them were guilty of accidents.
Keywords
Psychoactive substances; Traffic injuries; Road accidents; Emergency medicine; Mortality
Introduction
World Health Organization (WHO) reported that the number of deaths due to road accidents has reached 1.35 million people worldwide. This statistic for Iran is 16,426 based on the latest surveys conducted (Nhan Tran coordinated the writing of the report with contributions by Jeanne Breene and Meleckidzedeck Khayesi 2018). 48.7% of accidents that lead to deaths in Iran are caused by motor vehicles (4 wheels) and 24.1% by motor vehicles (2 wheels) [1]. Driving under the influence of alcohol in people over 65 years of age is getting attention [2]. The mean age of accidental injuries in the group of users (46 years) is much smaller than that of those who did not use drugs (54 years) [1]. On the other hand, 68.2% of the injured who drive under the influence of psychoactive substances are between the ages of 25 and 84 [3]. The amount of conflict between alcohol consumption and opioids occurs more in the 25 to 34 years old, so the rate of accidents decreases with the increased age of drivers [1]. Among drivers involved in accidents, 61% had an illegal concentration for sedatives, 38% for stimulants, 20% for Tetrahydrocannabinol (THC), and 10% for opioid abuse [4,5]. Methadone (34.7%) and morphine (27.5%) are the most common substances in motorcyclists who had an accident [6]. Motorcyclist drivers were injured in Nigeria, 87% were alcohol, 42.2% were smoking marijuana, and 12.4% were tramadol [7]. Driving under the influence of amphetamine increases the risk of death by OR=20.9 [8].
Using the psychoactive substances has been increasing in recent years and thus, it has a direct relation with decreasing the level of consciousness and increasing the probability of accidents. The aim of this study was to research the effect of psychoactive substance use among injured drivers and its clinical outcome.
Materials and Methods
Study design
This case-control study was conducted from April 2021 to March 2022. The study site was 7 Tir Hospital affiliated with the Iran University of Medical Sciences, located in the southeast of Tehran. The protocol of the study was approved by the institutional review board and written informed consent was obtained from all patients who participated in the study. Only drivers injured in accidents and who went to the hospital by emergency 115 (pre-hospital services) were included in the study and were clinically tested for psychoactive substance use, which included stimulants, sedatives, opioids, hallucinogens, and cannabis. The injured who had positive results for psychoactive substances were in the case group (N=100), and the other injured were in the control group (N=260).
Data sources
The sampling method for this study is convenience, which is divided into two case groups (used substances) and the control group (not used) based on the criterion of the injured driver.
Clinical data such as frequency of substances, severity of injury, level of consciousness, triage level, and death were collected through the patient documents in the hospital, accident scene information (device, role, type of accident, and time) through the traffic police records, and demographics data such as age and gender were collected by asking the patient or his companion that all of them were written in the medical documents of the injured and available in the hospital. All the information about the outcomes of the study was collected during the hospitalization.
Statistical analysis
The results were analyzed in two sections. In the descriptive section, using the indicators available in descriptive statistics, such as mean and standard deviation for continuous variables and number and percentage for categorical variables were used. In addition, the independent sample T-test were used to compare continuous variables between groups, and the chi-square and Fisher exact test were used for categorical analysis. For determining important factors in death we used multiple logistic regressions. Evaluation of the model with Hosmer-Lemeshow and the ROC curve, all tests were assumed out at a significant level of 5% with spss26 software have been analyzed.
Results
Participants and descriptive data
The drivers involved in road accidents in Tehran Province, Iran, in during the study were referred to 7-Tir Hospital and were included in the study. Injured drivers (N=360) were examined. All of them were men. Among the case group, 59 patients used only one of the psychoactive substances within 24 hours before the accident, while 41 patients were multi-used. The results show that they used at least 2 or more substances used simultaneously or within at least 12 hours before the accident. Opioids are the most commonly used among the injured (n=61), and had the oldest mean age (41.9 ± 13.541), however, the hallucinogens (n=5), in this study was 3,4-Methylenedioxymethamphetamine (MDMA), had the youngest mean age (27 ± 4.159). Generally, people who used psychoactive substances were older than others in the control group (Figure 1).

Figure 1: Mean age in type of psychoactive substance use.
The most observed damage among the injured was related to hallucinogens and sedatives had a significant effect on the head trauma. Also, there is a significant difference between the use of stimulants, opioids, hallucinogens, and cannabis with the level of consciousness during triage. Out of the total study population (N=360), 250 injured were guilty and 94 of them had used psychoactive substances. The motorbike riders created a larger population of traffic injured than the car drivers (283 vs. 77, 4 p=<0.001), as among them 185 were guilty. The types of accidents that were reported included: Overturning, hitting a block, crashing two motorcyclists with each other, hitting a car and a motorcycle with each other, and accidents two cars with each other. All the overturning cases were guilty of the accident (Table 1).
| Variables | Case (N=100) | Control (N=260) | p-value |
|---|---|---|---|
| Age | 37.49 ± 13.61 | 34.18 ± 14.05 | 0.044 |
| Level of consciousness | |||
| A | 73 (73) | 230 (88.5) | 0.003* |
| P | 8 (8) | 7 (2.7) | |
| V | 16 (16) | 19 (7.3) | |
| U | 3 (3) | 4 (1.5) | |
| Role of accident | |||
| guilty | 94 (94) | 156 (60.0) | <0.001 |
| no guilty | 6 (6) | 104 (40.0) | |
| Device | |||
| car | 31(31) | 46 (17.7) | 0.006 |
| motorcycle | 69 (69) | 214 (82.3) | |
| Type of accident | |||
| overturning | 47 (47) | 78 (30.0) | <0.001 |
| hitting a block | 25 (25) | 26 (10.0) | |
| crashing two motorcyclists | 8 (8) | 20 (7.7) | |
| hitting a car and a motorcycle | 16 (16) | 119 (45.8) | |
| accidents two cars | 4 (4) | 17 (6.5) | |
| Time of arrival | |||
| 17:00 PM– 00:0 AM. | 52 (52) | 105 (40.4) | 0.008 |
| 1:00 AM-8:00 AM. | 24 (24) | 47 (18.1) | |
| 9:00 AM-16:00 PM. | 24 (24) | 108 (41.5) | |
Note: *Fisher exact test.
Table 1: Demographic information according the groups.
One of the essential aspects of this study was to research the relationship between the role of the accident and the use of psychoactive substances. The results showed that 26% of the studied population included injured who had used psychotropic substances and were guilty of the accident. Also, the results showed that there is a significant difference between the role of the injured and the type of accident (Table 2).
| Variables | Guilty | No guilty | p-value |
|---|---|---|---|
| Case | 94 (37.6) | 6 (5.5) | <0.001 |
| control | 156 (62.4) | 104 (94.5) | |
| Psychoactive | |||
| Single | 55 (58.5) | 4 (66.7) | >0.99 |
| Multi | 39 (41.5) | 2 (33.3) | |
| Stimulants | |||
| Yes | 32 (12.8) | 2 (1.8) | <0.001 |
| No | 218 (87.2) | 108 (98.2) | |
| Sedatives | |||
| Yes | 40 (16.0) | 3 (2.7) | <0.001 |
| No | 210 (84.0) | 107 (97.3) | |
| Opioids | |||
| Yes | 59 (23.6) | 2 (1.8) | <0.001 |
| No | 191 (76.4) | 108 (98.2) | |
| Device | |||
| Motorcycle | 185 (74.0) | 98 (89.1) | <0.001 |
| Car | 65 (26) | 12 (10.1) | |
| Type of accident | |||
| overturning | 125 (50.0) | 0 (0.0) | <0.001 |
| hitting a block | 50 (20.0) | 1 (0.9) | |
| crashing two motorcyclists | 17 (6.8) | 11 (0.1) | |
| hitting a car and a motorcycle | 47 (18.8) | 88 (80.0) | |
| accidents two cars | 11 (4.4) | 10 (9.0) | |
Table 2: psychoactive substance and accident information factors based on role of accident.
Outcome data
The linear regression results show that hallucinogens and sedatives cause the most damage. Head trauma, and then the decrease in consciousness, is one of the inevitable results of road accidents. Among the 45 injured who had symptoms of head trauma, 22 of them (48.9%) had used only one substance, and 23 (51.1%) had used more than one substance. The group that used sedatives had the most head trauma (60%) (Figure 2).
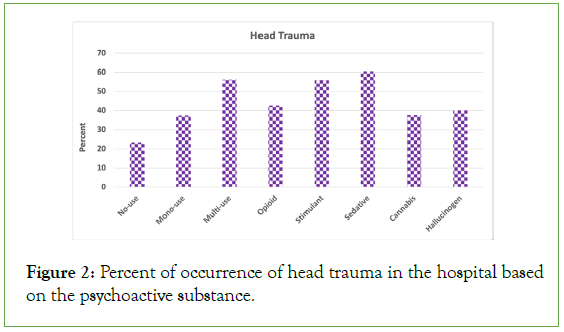
Figure 2: Percent of occurrence of head trauma in the hospital based on the psychoactive substance.
Most accidents were reported between 5:00 PM and 12:00 AM, 52 of them used substances and 50 were guilty. All of the motorcyclist riders that used substances (91.3%) were guilty, and the most common substances among them were opioids-34. Also, all the car drivers in the case group were guilty. 250 injured were guilty, and 94 used substances (Table 2). Among the studied groups, only 11 people died and 5 of them were just in the case group (Table 3).
| Variables | Alive (N=349) | Death (N=11) | p-value |
|---|---|---|---|
| Control | 254 (72.8) | 6 (54.5) | 0.184 |
| Case | 95 (27.2) | 5 (45.5) | |
| Single-used | 57 (60.0) | 2 (40.0) | 0.398*(fisher) |
| Multi-used | 38 (40.0) | 3 (60.0) | |
| Opioid | 58(61.1) | 3(60) | >.99* |
| Yes | 37(38.9) | 2(40) | |
| Stimulant | 33(34.7) | 1(20) | 0,659* |
| Yes | 62(65.3) | 4(80) | |
| Sedative | 39(41.1) | 4 (80) | 0.162* |
| Yes | 56(58.9) | 1(20) | |
| Time arrival | |||
| 17:00 PM-00:00 AM. | 150 (43) | 7 (63.6) | 0.342 |
| 01:00 AM-08:00AM. | 69 (19.8) | 2 (18.2) | |
| 09:00 AM-16:00 PM | 130 (37.2) | 2 (18.2) | |
| Type of accident | |||
| Overturning | 118 (33.8) | 7 (63.6) | 0.13 |
| Car and motorcycle | 180 (51.6) | 4 (36.4) | |
| Hitting a block | 51 (14.6) | 0(0.0) | |
| Role | |||
| Guilty | 242 (69.3) | 8 (72.7) | 0.99 |
| No guilty | 107 (30.7) | 3 (27.3) | |
Note: Due to the fact that all the traffic injured participating in this study were vehicle drivers (pedestrians, passengers, and cyclists were excluded), the number of deaths is very low.
Table 3: Compare psychoactive substance and accident information factors based on mortality.
Main result
Head trauma, type of accident, and level of triage have a significant effect on the death of the injured. Moreover, sedative substances have a greater effect on death. Also, the area under the Roc curve with a level of 92% shows that the model designed in this table predicts a 92% chance of death of the injured (Figure 3). There is a significant difference between the age and the role of people in the accidents between the case and the control group, which means that as the age increases, the probability of an accidental person being in the case group is 1.7%, also in the case group, the average age is 1.7% is more. On the other hand, this table states that 91% of the people who are guilty of accidents are in the case group (Table 4).
| Odds ratio | 95% CI | standard deviation | p-value | |
|---|---|---|---|---|
| Sedatives | 2.25 | (25.52-0.199) | 1.24 | 0.51 |
| Device | 2.77 | (13.21-0.58) | 0.79 | 0.20 |
| Type of accident | 0.33 | (1.004-0.105) | 0.57 | 0.05 |
| Head trauma | 7.65 | (43.220-1.353) | 0.88 | 0.02 |
| Time arrival | 0.63 | (1.461-0.275) | 0.43 | 0.28 |
| Substances | 0.41 | (5.235-0.033) | 1.29 | 0.49 |
| Severity of injury | 1.02 | (1.058-0.985) | 0.02 | 0.25 |
| Age | 0.98 | (1.039-0.934) | 0.03 | 0.58 |
| Multi-used | 2.04 | (18.279-0.228) | 1.12 | 0.52 |
| Triage level | 0.26 | (0.880-0.075) | 0.63 | 0.03 |
Table 4: Association between factors with mortality.

Figure 3: Roc Curve; the area under the Roc curve with a level of 92% shows that the model designed in this table predicts a 92% chance of death of the injured
Discussion
According to the results, the most common substances among the injured were related to opioids.
In Australia, 58% of drivers have reported driving under the influence of drugs, among which the use of marijuana is one of the three most essential factors in traffic violations. The most common substance among drivers is methamphetamine (39.4%), THC (34%), and the simultaneous use of these two substances together (21.9%). On the other hand, when examining cases that had used two or more psychoactive substances together, 64% reported methamphetamine, 59% THC, and 1.8% MDMA [9]. In Italy, 26% of drivers tested positive for alcohol and 20% for other psychoactive substances, among which the most common substances are cannabinoids at 9.7%, cocaine at 7.2%, and benzodiazepines at 4.1%, narcotics at 1.9% and other psychoactive substances such as amphetamines with 1.7%. Using psychoactive substances with alcohol at the same time was seen by 30% of the study population [10]. The use pattern of alcohol and illegal drugs was investigated in North-Eastern Italy and showed that among the population of 2160, 31 people used alcohol, 212 people used illegal drugs, and 131 people used several psychoactive substances simultaneously. It was reported that 165 drivers tested positive for cocaine, out of which it was determined that 122 people consumed alcohol and cocaine simultaneously [11]. In the United States of America, cannabis use was reported by 96% of the study population, followed by stimulants at 19% and sedatives at 9% as the most common substances reported among drivers [12].
In terms of the severity of the injury, most injuries seen for the hallucinogens, and sedatives users had higher symptoms of head trauma. It was also found that the use of sedatives has a greater effect on the death of the injured. We found that there is a significant difference between the use of psychoactive substances such as stimulants, opioids, hallucinogens, and cannabis and the level of triage of the injured when entering the hospital emergency room and all of the injured were only men. Only 5 injured among the case group died because drivers were studied just. Regarding injury severity, 31% of alcohol-used car accident deaths and 42% of fatal injuries were reported among drug-used drivers in the United States of America; however, in Canada, this statistic is 75 people killed and 4,407 injured among drivers who consumed cannabis [13,14]. Fatal accidents were occurred among 62.3% of drivers in Canada, 65% of drivers in the United States, and 95% of the drivers in Denmark who had used drugs and were all men, while driving under the influence of marijuana, alcohol, and drugs was reported among female students (54.1%) in the United States of America [15-18].
Opioids showed a higher mean age, and the hallucinogens had the youngest users. The mean age for alcohol, cocaine, and injectable drug use among drivers in Milan, Australia, and in Spain has been reported between 30 and 40 years, but in New Zealand, it was 47.26 years [15,18-20]. In Ontario, Canada, among drivers who use alcohol or opioid painkillers, it is reported 46 years old [21].
It is shown that in the case group, most of the injured were motorcyclists, of which the majority of them were guilty of accidents, and most accidents happened between 17:00 in the evening and midnight. In Australian 34.6% of drivers admitted that they drove for about 3 hours, and more than 50% drove for at least 7 hours after consuming cannabis [21]. Meanwhile, 56.4% of drivers in the United States of America reported driving within 2 hours after consuming cannabis [22].
Psychoactive substances are consumed in different ways, among the drivers who drove under the influence of marijuana, 94.1% used a pipe, 92.1% used as a joint (cigarette), 87.7% inhaled through tobacco-free water pipes, 72.4% inhaled through tobacco-free blunts, and 68% was ingested [23].
Limitations
Unfortunately, due to the replacement of the forensic specialist in the mentioned hospital, although all the drivers who visited the hospital from April 2021 to March 2022 due to injuries caused by road accidents were taken into account, however, we were only able to read the files of the injured in the period from April to September 2021, extract the desired information and carry out the necessary investigations.
If we had been able to access the history of drug use, the exact time, and the ways of using them, our report would be more complete, and we could cover all aspects of the initial hypothesis.
Conclusion
The risk of accidents increases with the use of psychoactive substances. The required data for the case and control groups were collected from the medical records and police reports, during it was found that the people in the case group were older than the control group, and among them, opioids were the most used. Using sedatives increases the symptoms of injury, including head trauma, and finally, most of the injuries who had an accident after using psychoactive substances were motorcycle riders.
Acknowledgment
We thank the Trauma and Injury Research Center for the consulting of the data collecting.
Authors Contributions
NT, ZM, AA, TB: Conceptualizations and study design, NT, TB: Data collection, AA, TB: Data analyzer and visualization, NT, ZM: Interpretation the result, AA, TB: Writing-original draft, NT, ZM: Writing review and editing. All authors have approved the final manuscript.
Funding
None
Conflict of Interest
The authors have no conflicts of interest to disclose
Data Availability Statement
Data are however available from the corresponding author upon reasonable request and with permission of the institute will be sent.
References
- Alvarez-Freire I, López-Guarnido O, Cabarcos-Fernández P, Couce-Sánchez M, Bermejo-Barrera AM, Tabernero-Duque MJ. Statistical analysis of toxicological data of victims of traffic accidents in galicia (spain). Prev Sci. 2023:1-9.
[Crossref] [Google Scholar] [PubMed]
- Myers MG, Bonar EE, Bohnert KM. Driving under the influence of cannabis, alcohol, and illicit drugs among adults in the United States from 2016 to 2020. Addict Behav. 2023;140:107614.
[Crossref] [Google Scholar] [PubMed]
- Hasan R, Watson B, Haworth N, Oviedo-Trespalacios O. What contributes to drug driving? An exploratory investigation into the influence of problematic substance use, roadside testing and alternative transport options. Accid Anal Prev. 2023;184:106990.
[Crossref] [Google Scholar] [PubMed]
- Abdel-Aty MA, Abdelwahab HT. Exploring the relationship between alcohol and the driver characteristics in motor vehicle accidents. Accid Anal Prev. 2000;32(4):473-482.
[Crossref] [Google Scholar] [PubMed]
- Gjerde H, Bogstrand ST, Jamt RE, Vindenes V. Crash-involved THC-positive drivers in Norway have a high frequency of polysubstance use. Drug Alcohol Depend. 2023;244:109800.
[Crossref] [Google Scholar] [PubMed]
- Divsalar P, Mohammadi M, Divsalar K. Drug use and pattern of injuries sustained by drivers involved in road traffic crashes. Traffic Inj Prev. 2021;22(3):195-200.
[Crossref] [Google Scholar] [PubMed]
- Bako IA, Atsaakaa HJ, Dane S. 2020. Perception and use of psychoactive substances among commercial motorcyclists in makurdi metropolis, nigeria. J Res Med Dent Sci. 8(3):229-236.
- Hayley AC, Downey LA, Shiferaw B, Stough C. Amphetamine-type stimulant use and the risk of injury or death as a result of a road-traffic accident: A systematic review of observational studies. Eur Neuropsychopharmacol. 2016;26(6):901-922.
[Crossref] [Google Scholar] [PubMed]
- Mills L, Freeman J, Davey J, Davey B. The who, what and when of drug driving in Queensland: Analysing the results of roadside drug testing, 2015–2020. Accid Anal Prev. 2021;159:106231.
[Crossref] [Google Scholar] [PubMed]
- Snenghi R, Pelletti G, Frigo AC, Forza G, Nalesso A, Montisci M, et al. The dangerous pattern of concurrent use of alcohol and cocaine among drunk-drivers of Northeast Italy. Alcohol Alcohol. 2018;53(6):735-741.
[Crossref] [Google Scholar] [PubMed]
- Favretto D, Visentin S, Stocchero G, Vogliardi S, Snenghi R, Montisci M. Driving under the influence of drugs: Prevalence in road traffic accidents in Italy and considerations on per se limits legislation. Traffic Inj Prev. 2018;19(8):786-793.
[Crossref] [Google Scholar] [PubMed]
- Bonar EE, Arterberry BJ, Davis AK, Cunningham RM, Blow FC, Collins RL et al. Prevalence and motives for drugged driving among emerging adults presenting to an emergency department. Addict Behav. 2018;78:80-84.
[Crossref] [Google Scholar] [PubMed]
- Marillier M, Verstraete AG. Driving under the influence of drugs. Wiley Interdisciplinary Reviews: Forensic Science. 2019;1(3):e1326.
- Wettlaufer A, Florica RO, Asbridge M, Beirness D, Brubacher J, Callaghan R, et al. Estimating the harms and costs of cannabis-attributable collisions in the Canadian provinces. Drug Alcohol Depend. 2017;173:185-190.
[Crossref] [Google Scholar] [PubMed]
- Dubois S, Bédard M, Weaver B. The association between opioid analgesics and unsafe driving actions preceding fatal crashes. Accid Anal Prev. 2010;42(1):30-37.
[Crossref] [Google Scholar] [PubMed]
- Li K, Simons-Morton B, Gee B, Hingson R. Marijuana-, alcohol-, and drug-impaired driving among emerging adults: Changes from high school to one-year post-high school. J Safety Res. 2016;58:15-20.
[Crossref] [Google Scholar] [PubMed]
- Rudisill TM, Smith GS. Risk factors associated with driving under the influence of drugs in the USA. Injury prevention. 2021;27(6):514-520.
[Crossref] [Google Scholar] [PubMed]
- Simonsen KW, Linnet K, Rasmussen BS. Driving under the influence of alcohol and drugs in the eastern part of Denmark in 2015 and 2016: Abuse patterns and trends. Traffic Inj Prev. 2018;19(5):468-75.
[Crossref] [Google Scholar] [PubMed]
- Li K S-MB, Gee B, Hingson R. Marijuana-, alcohol-, and drug-impaired driving among emerging adults: Changes from high school to one-year post-high school. J Safety Res. 2016.
[Crossref] [Google Scholar] [PubMed]
- Marillier M VA. Driving under the influence of drugs. Wiley Interdisciplinary Reviews: Forensic Science. 2019.
- Arkell TR, Lintzeris N, Mills L, Suraev A, Arnold JC, McGregor IS. Driving-related behaviours, attitudes and perceptions among Australian medical cannabis users: Results from the CAMS 18-19 survey. Accid Anal Prev. 2020;148:105784.
[Crossref] [Google Scholar] [PubMed]
- Bonar EE CJ, Arterberry BJ, Walton MA, Bohnert KM, Ilgen MA. Driving under the influence of cannabis among medical cannabis patients with chronic pain. Drug Alcohol Depend. 2019.
[Crossref] [Google Scholar] [PubMed]
- Berg CJ DC, Vu M, Li J, Martin K, Le L. Marijuana use and driving under the influence among young adults: A socioecological perspective on risk factors. Subst Use Misuse. 2018.
[Crossref] [Google Scholar] [PubMed]
Citation: Tavakoli N, Mousavi Z, Amanollahi A, Babeveynezhad T (2023) The Effect of Psychoactive Substances used on Clinical Outcomes in Injured Drivers Referred to Emergency Medicine; Case-Control Study. J Pharmacogenom Pharmacoproteomics. 14:072.
Copyright: © 2023 Tavakoli N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

