Indexed In
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2023) Volume 8, Issue 3
The Association of Radiological Severity with Inflammatory Biomarkers for Prognostic Prediction in Patients with COVID-19
Yousra Zouine*, Meriam Benzalim and Soumaya AljReceived: 21-Mar-2023, Manuscript No. JIDD-23-20221; Editor assigned: 23-Mar-2023, Pre QC No. JIDD-23-20221 (PQ); Reviewed: 06-Apr-2023, QC No. JIDD-23-20221; Revised: 13-Apr-2023, Manuscript No. JIDD-23-20221 (R); Published: 20-Apr-2023, DOI: 10.35248/2576-389X.23.08.213
Abstract
Background: COVID-19, brought on by SARS-CoV-2, has spread worldwide. It progresses quickly and brings on serious and deadly complications. It would be helpful in screening, classifying patients, and avoiding severe complications to link radiological severity with useful biomarkers like CRP, leucocytes, lymphocytes, and D-Dimer.
Aims and objectives: To identify patients at risk of fatal complications, the research looked into the relationship between inflammatory biomarker levels and HRCT chest findings.
Materials and methods: The Ibn Tofail hospital COVID-19 dedicated center undertook this retrospective monocentric observational research. The research included 177 patients>18 years old who were admitted between September 1, 2020 and November 30, 2020 with a laboratory-confirmed diagnosis of COVID-19. Retrospective data collection from patient records was done on demographics, illness severity, laboratory measurements, and radiology imaging. Based on CT Severity scoring, the illness severity was divided into three categories: light, mild to severe, and critical. Every patient had an HRCT Chest and inflammatory biomarkers sent in at the time of admission, and the results were documented.
Results: In our research, 61 female patients and 116 male patients participated. Patients with severe lung involvement have an average age of 61.9 years, whereas those with non-severe lung involvement have an average age of 56.8 years, and there is a substantial correlation between age and the severity of lung involvement (p-value: 0.017). According to HRCT chest results, patients with elevated CRP levels (P-value 0.001), D-Dimer levels (P value 0.032), and low lymphocyte levels (P value 0.001) had more severe lung involvement. Additionally, it was discovered that radiological severity among COVID-19 patients was strongly correlated with capillary oxygen SATURATION. The CT severity score had greater sensitivity, specificity, and overall accuracy in predicting severe, critical cases, and short-term mortality when compared to CRP, leukocytes, lymphocytes, and D-Dimeres levels.
Conclusion: Because COVID-19 disease severity is correlated with radiological severity and inflammatory markers, it will be easier to classify patients into various risk groups as soon as they are diagnosed in order to ensure efficient resource allocation.
Keywords
CT severity score, Covid prognosis, Inflammatory bio markers, Chest-CT, COVID-19
Introduction
On March 12, 2020, the World Health Organization (WHO) declared COVID-19 to be an epidemic [1]. The number of cases and deaths reported globally to date total 667,815,009, with 6,729,542 deaths, and the daily death toll is rising as new variants and mutants appear [2,3].
Since CT was found to have a high sensitivity in SARS-CoV-2- infected patients, it is frequently used to categorize patients, aid in clinical care, and avert life-threatening complications. The most visible measure that can indicate the degree of inflammation is the extent of chest Computed Tomography (CT) involvement [4].
D-Dimer, CRP, IL6, and LDH are biomarkers that are frequently examined to determine how severe COVID-19 illnesses.
In patients with SARS-COV-2 pneumonia, the D-dimer level may be more closely linked to the degree of inflammation than to the hypercoagulable state [5].
A sign of lung deterioration and progression, CRP substantially increased in the early stages of severe COVID-19 patients [6].
In order to determine whether there is a correlation between them and evaluate the value of CT versus biomarkers as a prognostic value for COVID-19 disease severity and short-term clinical outcome, we looked at the relationship between levels of inflammatory markers and CT severity score in patients with SARS-COV-2 pneumonia in this study.
Materials and Methods
It was a retrospective monocentric observational study undertaken at Ibn Tofail hospital COVID-19 dedicated center. 177 Patients>8 year of age who were admitted from September 1, 2020 up to November 30, 2020 with laboratory confirmed diagnosis of COVID-19 were included in the study. Data was collected on demography, disease severity, laboratory measurements, radiology imaging retrospectively from records of patients. The disease severity was classified into light, mild to severe and critic based on CT severity scoring. HRCT Chest and inflammatory biomarkers were sent in patients at the time of admission and the outcome was recorded.
The severity of the disease was classified according to the French Society of Radiology classification which proposed a harmonization of the estimation of the total lung extension, qualified as mild between 0%-25%, moderate between 25%-50%, severe between 50%-75% and critical beyond 75% (Figure 1).

Figure 1: Chest CT scans demonstrating the extent of the COVID-19 lesions.
Calculating frequencies for qualitative variables, using measures of central tendency (means) and dispersion (standard deviation) for quantitative variables.
The t-test was used to compare means of quantitative data between 2 groups to determine whether there is a statistically significant difference between the means. For comparing means between more than 2 groups, the one-way Analysis of Variance (ANOVA) was used to determine whether there are any statistically significant differences between the means. Bivariate analysis was conducted to determine whether there is any relationship between 2 qualitative variables using chi-squared (χ²) test. The level of significance was set to 0.05 for the study.
To study the specificity and sensitivity of CT versus biomarkers, we used the Receiver Operating Characteristic Curve (ROC curve), which allowed us to specify the area under the curve of each element, called Area under the ROC Curve "AUC". The AUC of the curve of the biomarker studied must be greater than or equal to 0.5 in order for it to perform well. The ROC curves also allow the detection of the best CT threshold value and biomarkers for the detection of severe cases.
Results
There were 116 male patients and 61 female patients in our study. The mean age of patients with severe to critical lung involvement was 61.9 years, compared with 56.8 years for patients with mild to mild lung involvement (compare means, p-value 0.017) (Table 1).
| Biomarkers | Reference values |
|---|---|
| Leukocytes | 4000 elm-10000 elm |
| Lymphocytes | 1500 elm-4000 elm |
| CRP | <6 mg/L |
| D-Dimeres | <500 ug/L |
Table 1: Reference values for inflammatory biomarkers.
Significant association between age and severity of lung involvement we have shown that there is a significant inverse relationship (p-value<0.001) between CT severity and capillary oxygen saturation (Table 2).
| Evolution | |||||
|---|---|---|---|---|---|
| Poor prognosis | Good prognosis | P | |||
| Extension | Light to mild | N | 9 | 77 | 0.033 |
| % | 0.105 | 0.895 | |||
| Severe to critical | N | 69 | 20 | ||
| % | 0.775 | 0.225 | |||
Table 2: Association of prognosis and lung involvement.
A statistically significant correlation was found between the CT extent of the lesion and patient outcome, p=0.033 (Table 3). Of the 177 patients in our study, 28 with severe to critical lung involvement had elevated D-dimer levels (P-value=0.032) (Table 4).
| Extension | N | Mean | Standard deviation | p | |
|---|---|---|---|---|---|
| Age | Light to mild | 86 | 56.85 | 16.123 | 0.017 |
| Severe to critical | 89 | 61.91 | 11.163 | ||
| SaO2 | Light to mild | 85 | 93.54 | 4.067 | p<0.001 |
| Severe to critical | 88 | 86.61 | 7.188 | ||
| Leucocytes | Light to mild | 67 | 9244.18 | 3585.765 | 0.13 |
| Severe to critical | 77 | 11670.13 | 12610.69 | ||
| CRP | Light to mild | 68 | 87.46 | 72.483 | p<0.001 |
| Severe to critical | 78 | 161.08 | 120.679 | ||
| Lymphocytes | Light to mild | 65 | 1351.848 | 669.073 | 0.001 |
| Severe to critical | 71 | 998.6338 | 589.5543 | ||
| CREAT | Light to mild | 62 | 8.44 | 3.159 | 0.216 |
| Severe to critical | 66 | 9.81 | 8.133 | ||
| TP | Light to mild | 18 | 28.389 | 3.5721 | 0.88 |
| Severe to critical | 39 | 28.274 | 2.0953 | ||
| DD | Light to mild | 34 | 1479.368 | 1386.617 | 0.032 |
| Severe to critical | 28 | 5757.036 | 9932.427 | ||
Table 3: Comparison of age, capillary blood saturation and biological findings between patients who have light to mild, and severe to critical lung involvement.
In our study, of 146 patients with elevated CRP, 78 had severe pulmonary involvement and 68 had mild to mild pulmonary involvement.
In contrast, there were 31 patients with normal CRP levels, of which 10 had severe lung involvement and 21 had non-severe lung involvement. There was significant association between levels of CRP and severity of lung involvement (p value p<0.001) (Table 4).
| Area under the curve | |||||
|---|---|---|---|---|---|
| Test result variables | Area | Standard error | Asymptotic sig. | 95% asymptotic confidence interval | |
| Lower boundary | Higher boundary | ||||
| Age | 0.663 | 0.075 | 0.045 | 0.515 | 0.81 |
| Leukocytes | 0.572 | 0.085 | 0.376 | 0.405 | 0.739 |
| CRP | 0.746 | 0.071 | 0.002 | 0.606 | 0.886 |
| Creatinine | 0.447 | 0.082 | 0.516 | 0.286 | 0.608 |
| DD | 0.651 | 0.076 | 0.063 | 0.503 | 0.799 |
Table 4: Areas under the curve.
There were 136 patients with lymphopenia, out of which 71 were having severe lung involvement and 65 had non-severe lung involvement. In contrast, there were 41 patients with normal lymphocytes levels, of which 9 had severe lung involvement and 32 had non-severe lung involvement. There is significant association between levels of lymphopenia and severity of lung involvement (p value=0.001) (Table 4).
Out of 177 patients that we have included in our study, 49 patients had isolated raised creatinine. It showed weak association with severe lung involvement (p=0.2).
In our study, the calculated AUCs were as follows: age 0.663, saturation 0.797, leukocytes 0.572, lymphocytes 0.682, DD 0.651, CRP 0.746. Biomarkers with AUC<or equal to 0.5 were excluded from the next step (Creatinine) (Figure 2).
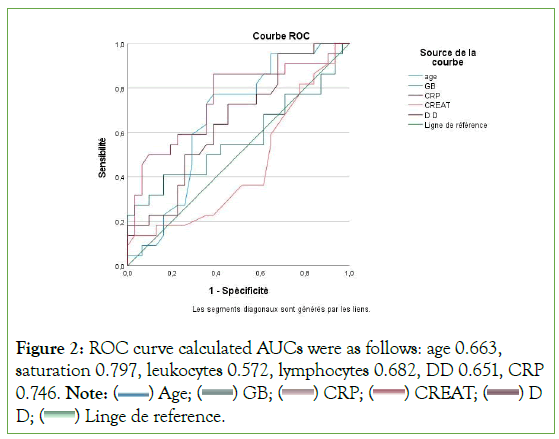
Figure 2: ROC curve calculated AUCs were as follows: age 0.663,
saturation 0.797, leukocytes 0.572, lymphocytes 0.682, DD 0.651, CRP
0.746. Note: ( ) Age; (
) Age; ( ) GB; (
) GB; ( ) CRP; (
) CRP; ( ) CREAT; (
) CREAT; ( ) D
D; (
) D
D; ( ) Linge de reference.
) Linge de reference.
ROC curve analysis showed that the Area Under the Curve (AUC) was significantly elevated using CT severity score cut-off ≥ 50%, CRP cut-off ≥ 95 mg/L, leukocyte cut-off ≥ 11210 elm/mm³ and DD cut-off ≥ 700 ug/L for severe COVID-19 cases, with a sensitivity, specificity of 85%-58%, compared with 75%-55% for CRP, 85%-55%, compared with 62%-55% for leukocytes and 80%- 48% compared with 70%-40% for DD respectively (Figure 3).
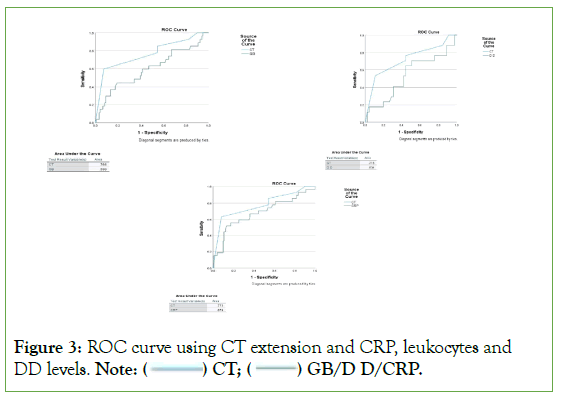
Figure 3: ROC curve using CT extension and CRP, leukocytes and
DD levels. Note: ( ) CT; (
) CT; ( ) GB/D D/CRP.
) GB/D D/CRP.
Discussion
The diagnosis of pulmonary abnormalities often involves the use of a lung Computed Tomography (CT) scan, which also plays a significant part in the diagnosis and clinical grading of patients who are suspected of having infections [7].
Ground-glass opacities that are bilateral and multilobar are the most typical forms of this infection [8,9]. Additionally, it has been established that the lower and periphery regions of the lung are most commonly impacted. Additional research also revealed other radiological patterns for COVID-19-infected individuals, including crazy paving pattern, airway change, and inverted halo sign [10,11].
A few studies have also highlighted the connection between the results of CT scans and patients' clinical conditions, illuminating the potential value of lung CT scans in assessing the severity and spread of illness [12].
Our research aims to evaluate the level of radiological and biomarker severity in relation to COVID-19 disease severity. CRP is a sensitive biomarker of tissue damage, infection, and inflammation and is a non-specific acute-phase protein produced by IL-6 in the liver. According to studies, CRP levels were substantially correlated with the severity of lung involvement (p=0.0346, RR of 2.02, Odds Ratio of 2.37) in severe COVID-19 patients at the initial stage, which is an indication of lung deterioration and disease progression [11]. Our research supports and affirms that CRP levels can serve as a marker for serious illness and escalating inflammation [13,14].
A higher D-dimer level was also linked to in-hospital mortality, according to several investigations [15,16]. The most popular theory put forth was that the hypercoagulable condition, which could be indicated by a high D-dimer level, might cause thrombotic events, leading to detrimental consequences. However, it was believed that the coronavirus-induced local and systemic inflammation was what led to the coagulopathy. D-dimer is also recognized as an inflammatory indicator [17].
Therefore, Lan Wang and colleagues put forth the theory that in SARS-COV-2 pneumonia patients, the D-dimer level may be more closely linked to the degree of inflammation than to the hypercoagulable state. Additionally, it was discovered that patients with D-dimer levels>0.7 mg/L had substantially higher CT scores (12.0 (P 0.001)) and more cases of reticulation and/or traction bronchiectasis on chest CT images (83.3% vs. 46.2%, P=0.002) than those with levels ≤ 0.7 mg/L. The CT score was considerably correlated with the natural logarithm of the D-dimer level (rS=0.586, P 0.001) [5].
Multiple virus-infected illnesses, including SARS, MERS, and respiratory syncytial virus, have been linked to lymphopenia [18- 23]. According to a prior study, lymphopenia in SARS patients may result from improved vascular sequestration brought on by higher levels of soluble vascular cell adhesion molecule-1 [24].
In our study lymphopenia was a good predictor of severe lung involvement which agrees with the study of Jiheng Liu and all that showed the correlation of Lymphopenia with severity grades of pneumonia (P<0.001). Lymphopenia was associated with a prolonged duration of hospitalization (17.0 days vs.14.0 days, P=0.002) [25].
Conclusion
Older age (>61 years), elevated D-dimer, CRP and low lymphocyte count are significantly correlated with severe lung injury and are risk factors for poor prognosis in patients with COVID-19. CT severity scoring has high accuracy and significant predictive power compared to other biomarkers. In particular, it has higher sensitivity, specificity and accuracy than CRP, WBC, lymphocytes and D-dimer. Our study revealed that CT scoring is a powerful means to determine the risk of death from COVID-19 disease in patients and to triage the need for hospitalization. It is also useful for prioritizing medical resources to make better decisions for the best clinical outcomes.
Disclosures
Human subjects: Consent was obtained or waived by all participants in this study.
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
Conflicts of Interest
In compliance with the ICMJE uniform disclosure form, all authors declare the following:
Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Ethical Approval
This is a retrospective study that doesn’t implement any experiment on human subjects and therefore we didn’t need the ethics committee consent.
References
- Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med. 2020;382(13):1199-1207.
[Crossref] [Google Scholar] [PubMed]
- Ai T, Yang Z, Hou H, Zhan C. WHO Director-General's opening remarks at the media briefing on COVID-19. 2020.
- Scherer PM, Chen DL. Imaging pulmonary inflammation. J Nucl Med. 2016;57(11):1764-1770.
[Crossref] [Google Scholar] [PubMed]
- Wang L, Yang L, Bai L, Huang Z, Peng Y. Association between D-dimer level and chest CT severity score in patients with SARS-CoV-2 pneumonia. Sci Rep. 2021;11(1): 11636.
[Crossref] [Google Scholar] [PubMed]
- Tan C, Huang Y, Shi F, Tan K, Ma Q, Chen Y, et al. C‐reactive protein correlates with computed tomographic findings and predicts severe COVID‐19 early. J Med Virol. 2020;92(7):856-862.
[Crossref] [Google Scholar] [PubMed]
- Li W, Cui H, Li K, Fang Y, Li S. Chest computed tomography in children with COVID-19 respiratory infection. Pediatr Radiol. 2020;50:796-799.
[Crossref] [Google Scholar] [PubMed]
- Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus disease 2019 (COVID-19): a systematic review of imaging findings in 919 patients. AJR Am J Roentgenol. 2020;215(1):87-93.
[Crossref] [Google Scholar] [PubMed]
- Wang W, Gao R, Zheng Y, Jiang L. COVID-19 with spontaneous pneumothorax, pneumomediastinum and subcutaneous emphysema. J Travel Med. 2020;27(5):taaa062.
[Crossref] [Google Scholar] [PubMed]
- Ye Z, Zhang Y, Wang Y, Huang Z, Song B. Chest CT manifestations of new coronavirus disease 2019 (COVID-19): a pictorial review. Eur Radiol. 2020;30:4381-4389.
[Crossref] [Google Scholar] [PubMed]
- Ali TF, Tawab MA, ElHariri MA. CT chest of COVID-19 patients: what should a radiologist know? Egypt J Radiol Nucl Med. 2020;51:1-6.
- Aalinezhad M, Alikhani F, Akbari P, Rezaei MH, Soleimani S, Hakamifard A. Relationship between CT severity score and capillary blood oxygen saturation in patients with COVID-19 infection. Indian J Crit Care Med. 2021;25(3):279-283.
[Crossref] [Google Scholar] [PubMed]
- Soraya GV, Ulhaq ZS. Crucial laboratory parameters in COVID-19 diagnosis and prognosis: an updated meta-analysis. Med Clin (Barc). 2020;155(4):143-151.
[Crossref] [Google Scholar] [PubMed]
- Gupta P, Halani A, Samuel T, Singh DP. Association of inflammatory biomarkers with radiological severity for COVID-19 patient risk stratification: An Indian perspective. Asian J Med Sci. 2021 Apr 1;12(4):1-7.
- Zhang L, Yan X, Fan Q, Liu H, Liu X, Liu Z, et al. D‐dimer levels on admission to predict in‐hospital mortality in patients with Covid‐19. J Thromb Haemost. 2020;18(6):1324-1329.
[Crossref] [Google Scholar] [PubMed]
- Cummings MJ, Baldwin MR, Abrams D, Jacobson SD, Meyer BJ, Balough EM, et al. Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study. Lancet. 2020;395(10239):1763-1770.
[Crossref] [Google Scholar] [PubMed]
- Agapakis DI, Tsantilas D, Psarris P, Massa EV, Kotsaftis P, Tziomalos K, et al. Coagulation and inflammation biomarkers may help predict the severity of community‐acquired pneumonia. Respirology. 2010;15(5):796-803.
[Crossref] [Google Scholar] [PubMed]
- He Z, Zhao C, Dong Q, Zhuang H, Song S, Peng G, et al. Effects of Severe Acute Respiratory Syndrome (SARS) coronavirus infection on peripheral blood lymphocytes and their subsets. Int J Infect Dis. 2005;9(6):323-330.
[Crossref] [Google Scholar] [PubMed]
- Booth CM, Matukas LM, Tomlinson GA, Rachlis AR, Rose DB, Dwosh HA, et al. Clinical features and short-term outcomes of 144 patients with SARS in the greater Toronto area. JAMA. 2003;289(21):2801-2809.
[Crossref] [Google Scholar] [PubMed]
- Liu CY, Huang LJ, Lai CH, Chen HP, Chen TL, Fung CP, et al. Clinical characteristics, management and prognostic factors in patients with probable Severe Acute Respiratory Syndrome (SARS) in a SARS center in Taiwan. J Chin Med Assoc. 2005;68(3):110-117.
[Crossref] [Google Scholar] [PubMed]
- Yang YM, Hsu CY, Lai CC, Yen MF, Wikramaratna PS, Chen HH, et al. Impact of comorbidity on fatality rate of patients with Middle East respiratory syndrome. Sci Rep. 2017;7(1):1-9.
[Crossref] [Google Scholar] [PubMed]
- Arabi YM, Arifi AA, Balkhy HH, Najm H, Aldawood AS, Ghabashi A, et al. Clinical course and outcomes of critically ill patients with Middle East respiratory syndrome coronavirus infection. Ann Intern Med. 2014;160(6):389-397.
[Crossref] [Google Scholar] [PubMed]
- O'Donnell DR, Carrington D. Peripheral blood lymphopenia and neutrophilia in children with severe respiratory syncytial virus disease. Pediatr Pulmonol. 2002;34(2):128-130.
[Crossref] [Google Scholar] [PubMed]
- Chen RF, Chang JC, Yeh WT, Lee CH, Liu JW, Eng HL, et al. Role of vascular cell adhesion molecules and leukocyte apoptosis in the lymphopenia and thrombocytopenia of patients with Severe Acute Respiratory Syndrome (SARS). Microbes Infect. 2006;8(1):122-127.
[Crossref] [Google Scholar] [PubMed]
- Liu J, Li H, Luo M, Liu J, Wu L, Lin X, et al. Lymphopenia predicted illness severity and recovery in patients with COVID-19: A single-center, retrospective study. PLoS One. 2020;15(11):0241659.
[Crossref] [Google Scholar] [PubMed]
- Manal M, Abdelilah E, Mohammed M, Rajae A, Amine BM, Houssam B, et al. Lymphopenia in Covid-19: A single center retrospective study of 589 cases. Ann Med Surg. 2021;69:102816.
[Crossref] [Google Scholar] [PubMed]
Citation: Zouine Y, Benzalim M, Alj S (2023) The Association of Radiological Severity with Inflammatory Biomarkers for Prognostic Prediction in Patients with COVID-19. J Infect Dis Diagn. 8:212.
Copyright: © 2023 Zouine Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

