Indexed In
- RefSeek
- Hamdard University
- EBSCO A-Z
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2021) Volume 6, Issue 1
The Association between Root Caries, Xerostomia and Blood Glucose in a Patient with Type 2 Diabetes
Shona Sawhney, Khair Ul Bariya Ali, Ashleigh Mungur and Aylin Baysan*Received: 23-Jun-2021 Published: 14-Jul-2021, DOI: 10.35248/2572-5629.21.6.143
Abstract
Dental caries is the most prevalent infectious disease worldwide. A chronic and progressive disease can occur in primary or permanent dentition and can take place in any tooth surface of the crown or root. This slow destruction is related to the dynamic interaction process between the tooth structure, microbial biofilm and dietary carbohydrates, together with the influence of saliva and genetic factors. Reported oral complications associated with diabetes include xerostomia (dry mouth), dental caries, tooth loss, periodontal disease, denture intolerance and soft tissue lesions of the tongue and oral mucosa. The reduction in saliva flow rate and subsequent diminished buffering capacity with calcium and phosphate contents result in an increase in mouth acidity, which contributes to the loss of minerals from the tooth surface and subsequently development of dental caries. These complications would result in compromised quality of life and this is a burden to the healthcare system. Therefore, it is crucial that dental caries in Diabetes patients is identified early and managed effectively. In this case report, multiple root carious lesions in a patient with type 2 diabetes have been discussed by highlighting the potential contributing factors such as salivary components and polypharmacy. A high blood glucose finding highlighted that the patient presented lack of understanding related to the importance of managing Type 2 diabetes.
Keywords
Diabetes type 2; Xerostomia; Dental caries; Oral health; Blood glucose
Introduction
Dental caries is the most prevalent infectious disease worldwide. A chronic and progressive disease can occur in primary or permanent dentition and can take place in any tooth surface of the crown or root. This slow destruction is related to the dynamic interaction process between the tooth structure, microbial biofilm and dietary carbohydrates, together with the influence of saliva and genetic factors. Reported oral complications associated with diabetes include xerostomia (dry mouth), dental caries, tooth loss, periodontal disease, denture intolerance and soft tissue lesions of the tongue and oral mucosa. The reduction in saliva flow rate and subsequent diminished buffering capacity with calcium and phosphate contents result in an increase in mouth acidity, which contributes to the loss of minerals from the tooth surface and subsequently development of dental caries. These complications would result in compromised quality of life and this is a burden to the healthcare system. Therefore, it is crucial that dental caries in Diabetes patients is identified early and managed effectively. In this case report, multiple root carious lesions in a patient with type 2 diabetes have been discussed by highlighting the potential contributing factors such as salivary components and polypharmacy. A high blood glucose finding highlighted that the patient presented lack of understanding related to the importance of managing Type 2 diabetes.
Clinical relevance
This case report highlights the importance of taking holistic and tailored approach for patients when carrying out dental treatment. Patients might fail to understand the necessity of taking their medication. Despite not being medical practitioners, there is a duty of care to ensure that patients are educated and understand the reasoning behind managing their conditions and the impact on their oral health and general wellbeing.
Objective statement
The reader should understand the clinical implications of a Diabetes type 2 patients with high blood glucose levels and polypharmacy presenting multiple root carious lesions and generalized chronic periodontitis in a routine clinical practice. In addition, the importance of raising awareness in oral health for general health within general public should be emphasized among health care professionals.
Case Presentation
A 69-year-old male attended the undergraduate restorative clinic at Barts and the London School of Medicine and Dentistry due to “dull and constant” pain at the LR8 for a period of three days. On a scale of 1 to 10, the patient described the pain as a 5/10. This patient is a regular attender.
His medical history revealed Type 2 diabetes since 1992, coronary bypass surgery in August of 2017 due to multiple blocked coronary arteries, asthma for 10 years, indigestion, and hypertension with hypercholesterolemia for 3-5 years. The patient is currently on multiple medications and has no known allergies or family history of diseases (Table 1).
| Medication | Dose | Frequency | Reason |
|---|---|---|---|
| Insulin Glulisine (Apidra) | 30 units | Three times daily | Diabetes mellitus |
| Aspirin | 75 mg | Once daily | Secondary prevention since coronary bypass |
| Atorvastatin | 40 mg | Once daily | High cholesterol |
| Bisoprolol | 7.5 mg | Once daily | High blood pressure |
| Clopidogrel | 75 mg | Once daily | Secondary prevention since coronary bypass |
| Insulin needles (Glucorx) | When needed | Diabetes Mellitus | |
| Lansoprazole | 15 mg | Once daily | Indigestion |
| Insulin Glargine (Lantus) | 30 units | Once daily | Diabetes Mellitus |
| Metformin | 1 g | Twice daily | Diabetes Mellitus |
| Beclometasone Dipropionate inhaler (Qvar) | 2 puffs | Two doses to be inhaled twice a day | Asthma |
| Salbutamol | One puff | One dose every 6-8 hours | Asthma |
| Ramipril | 2.5 mg | Once daily | High blood pressure |
| Tramadol | 37.5 mg | Three times daily | Pain management |
Table 1: Baseline demographics and clinical characteristics.
Dental history
His plaque control included brushing twice a day with a manual toothbrush and standard fluoridated toothpaste (1,450 ppm) twice a day however the patient was unsure about the duration. Mouthwash or any interdental aids have not been used previously.
The patient wears an upper complete acrylic tissue supported denture. Regarding the denture history, the patient has had numerous partial acrylic dentures over the past 15 years due to multiple midline fractures during mastication and takes the partial denture out regularly at night by keeping it in a glass of water alone. The denture is being cleaned sometimes with soap and water.
The patient is retired and used to work as a taxi driver. He is currently not stressed and lives with his wife, children and grandchild. He is non-drinker and has been an ex-smoker for six years, previously smoked for 22 years and usually had 10 cigarettes a day.
Clinical assessment
The dentition was minimally restored as presented in the hard tissue chart (Figure 1). Generalised marginal and interproximal calculus deposits were visible.
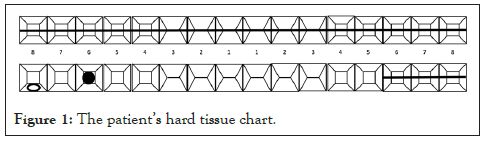
Figure 1: The patientâ??s hard tissue chart.
The Basic Periodontal Examination (BPE) scores were -/343 with immediate bleeding on probing in lower arch. The gingivae appeared inflamed with generalised gingival recession (between 2 and 6mm). There was generalised tooth surface loss reaching to dentine due to erosion and attrition. Regarding the upper partial denture bearing area, there was no apparent bone resorption, flabby tissue or soreness. There were clinically no interproximal lesions detected due to extensive calculus deposits.
Clinical examination revealed a large buccal cavity extending subgingivally at the LR8. The tooth in question was tender to palpation, percussion, air from the 3-in-1 syringe and cold testing (Endofrost, -50 degrees) (Table 2).
| Findings | Radiograph | |
|---|---|---|
| PA 1 | • Teeth present: LR8, LR7 and part of the LR6 • 3 mm horizontal bone loss between LR6 and LR7 • Vertical bone loss 2 mm between LR7 and LR8 • Radiolucency interproximal present on the mesial of the LR7 and LR6 • Interproximal radiolucency present distally of LR7 • Mesial interproximal radiolucency present on the LR8 • LR8 not in close proximity to the inferior alveolar canal |
PA 1 |
| PA 2 | • Teeth present: part of LR8, LR7, LR6, LR5 and part of LR4 • LR7: interproximal radiolucency mesially • LR6: secondary radiolucency beneath amalgam restoration and interproximal mesial and distal radiolucencies • LR5: interproximal radiolucencies mesially and distally • LR4: interproximal distal radiolucency |
 |
| PA 3 | • Teeth Present: LR1, LL1, LL2 and part of LL3 • Roughly 6 mm bone loss horizontally • LL2: interproximal radiolucency mesially and distally • LL3: interproximal radiolucency mesially |
PA 3 |
| PA 4 | • Teeth present: LL3, LL4 and LL5 • Roughly 4.5 mm horizontal bone loss • Interproximal radiolucencies mesially and distally of the LL3, LL4 and LL5 |
 |
Table 2: Shows the periapical radiographs taken to assess bone levels, any pathology and extent of dental caries.
The full-mouth periapical radiography revealed further radiolucencies consistent with root caries:
Radiolucencies consistent with root caries on the:
• LR5-mesial and distal
• LR4-distal
• LL1-distal
• LL2-mesial and distal
• LL3-mesial and distal
• LL4-mesial and distal
• LL5-mesial and distal
• LR6-mesial and distal
• LR7-mesial and distal
• Occlusal radiolucency consistent with secondary caries beneath t e amalgam restoration at the LR6
• Generalised 10-30% horizontal bone loss with localised severity in the lower anterior region (40-60%)
Due to the patient’s complex medical history including drug side effects of xerostomia and the patient’s root caries pattern, investigations into the patient’s salivary flow rate, pH and buffer capacity were carried out to identify a causal factor of the patient’s extensive root caries. The patient ate an hour before the salivary tests were completed (Table 3).
| Type of saliva | Consistency | Methodology | Flow rate (ml/min) | pH indicator | Buffer capacity |
|---|---|---|---|---|---|
| Unstimulated | Very viscous |
|
0.3 –indicated normal | 6.4 – moderately acidic | 4 – indicated very low |
| Stimulated | Very watery |
|
1.2 – indicated normal | 6.4 – moderately acidic | 3 – indicated very low |
Table 3: The patient’s salivary test outcome.
Caries risk assessment
It was decided to manage the patient’s dental caries via the Caries Management by Risk Assessment (CAMBRA) [1].
As seen on the form, patient was found to be at extreme risk of caries, looking at disease indicators, biological risk and protective factors. A tailored treatment plan including chemical therapy such as fluoride and minimally invasive restorative procedures to conserve tooth structure and function were considered [2].
The following diagnoses were subsequently made:
• Dental caries at the LR8 deemed unrestorable
• Root caries of the LL1, LL2, LL3, LL4, LL5, LR4, LR5, LR6, LR7
• Occlusal secondary caries of the LR6
• Generalised chronic moderate to severe periodontitis or based on the new classification–generalised periodontitis stage 3 Grade B–Currently Unstable–Risk: sub-optimally controlled diabetes2
• A combination of mild tooth surface loss just within dentine due to attrition (parafunctional habits; grinding) and extrinsic erosion due to acid reflux
• Acquired tooth loss due to periodontal disease and dental caries
Treatment plan
The treatment plan was devised to alleviate any pain, reduce the patient’s extreme caries risk and restore the teeth to function, to stabilise the patient’s periodontal condition and to make a complete upper cobalt-chrome denture that is retentive, stable and supportive (Table 4).
| Disease indicators | Check if Yes | ||
|---|---|---|---|
| 1. New cavities or lesions into dentin (radiographically) | X | ||
| 2. New white spot lesions on smooth surfaces | X | ||
| 3. New noncavitated lesions in enamel (radiographically) | X | ||
| 4. Existing restorations in last three years (new patient) or the last year (patient of record) | X | ||
| Biological or environmental risk factors | Check if Yes | ||
| 1. Cariogenic bacteria quantity not currently available | |||
| 2. Heavy plaque on the teeth | X | ||
| 3. Frequent snacking > 3 times daily | X | ||
| 4. Hyposalivatory medications | X | ||
| 5. Reduced salivary function (measured low flow rate)** | X | ||
| 6. Deep pits and fissures | |||
| 7. Recreational drug use | |||
| 8. Exposed tooth roots | X | ||
| 9. Orthodontic appliances | |||
| Protective factors | Check if Yes | ||
| 1. Fluoridated water | X | ||
| 2. F toothpaste once a day | |||
| 3. F toothpaste 2X daily or more | X | ||
| 4. 5000 ppm F toothpaste | |||
| 5. F varnish last 6 months | |||
| 6. 0.05% sodium fluoride mouthrinse daily | |||
| 7. 0.12% chlorhexidine gluconate mouthrinse daily seven days monthly | |||
| 8. Normal salivary function | |||
| Column 1 | Column 2 | Column 3 | |
| Final Score: Yes in Column 1:Indicates high or extreme risk Yes in columns 2 and 3: Consider the caries balance ** Hyposalivation plus high risk factors=extreme risk |
 |
||
| Final overall caries risk assessment category (check) determined as per guidelines on next page EXTREME  HIGH HIGH  MODERATE MODERATE  LOW LOW  |
|||
Table 4: The patient’s CAMBRA outcome.
Emergency phase: Extract the LR8 under the local anaesthetic since extensive dental caries at this tooth deemed unrestorable
Investigation, stabilisation and prevention phase:
• Prescription of high fluoride dentifrice containing 5000ppm fluoride (Duraphat, Colgate, UK) [3] due to having obvious active current dental caries.
• Saliva Testing: Investigating the flow rate (ml/min), pH and buffer capacity of the patient’s stimulated and unstimulated saliva to investigate the possible link between the patient’s saliva and his root caries pattern.
• Diet analysis (Table 5) and education: A diet sheet given to assess frequency of sugar intake in line with the Eat well Guide [3].
| Day | Breakfast | In-between | Mid-day | In-between | Evening | Before Bed |
|---|---|---|---|---|---|---|
| Thursday |
|
Tea with 3 tsp of honey |
|
Tea with 3 tsp of honey |
|
|
| Friday |
|
Tea with 3 tsp of honey |
|
Tea with 3 tsp of honey |
|
Tea with 3 tsp of honey |
| Saturday |
|
Tea with 3 tsp of honey |
|
Tea with 3 tsp of honey |
|
Tea with 3 tsp of honey |
| Sunday |
|
Tea with 3 tsp of honey |
|
Tea with 3 tsp of honey |
|
Tea with 3 tsp of honey |
Table 5: The patient’s initial diet analysis sheet.
• Oral Hygiene Instructions (OHI): Using interdental cleaning aids, brushing for two minutes with an appropriate brushing technique [3].
• Denture hygiene instructions: always clean over a bowl of water in case of dropping them, clean every night with soap and a toothbrush.
• Prescription of daily fluoride mouth rinse daily (0.05% NaF - Colgate FluoriGard) [3] due to having obvious active current root caries.
• Apply fluoride varnish to teeth twice yearly (2.2% NaF Colgate, Duraphat) [3] due to having obvious active current caries.
• Plaque and Bleeding Indices (100%) to monitor oral hygiene and gingival health [4].
• Full mouth six-point periodontal pocket chart before and after any treatment [4].
• Initial periodontal therapy – removal of plaque retentive factors including supra and subgingival calculus via supra/subgingival scaling [4].
• Supra and subgingival debridement, once plaque levels are below 20% [4].
Restorative and rehabilitation phase:
• Remove and restore the interproximal dental root caries with glass ionomer restorations.
• Remove and restore the occlusal secondary caries of the LR6 with amalgam due to patient preference.
• Make a complete upper cobalt-chrome denture to prevent further midline fractures due to being opposed to natural dentition.
Monitoring and maintenance phase:
• Reinforcement of OHI and denture hygiene.
• PIaque and bleeding indices to monitor oral and periodontal health [4].
• Blood glucose tests to continually monitor the patient’s blood glucose levels.
• Comprehensive periodontal assessment including six-point periodontal pocket chart post treatment - recall after 8 weeks of nonsurgical periodontal treatment to allow tissues to heal [4].
• Due to the patient being a high caries risk – clinical assessment with bitewing radiographs every six months [5].
• Recall scheduled within a three-month period due to high caries risk [6].
• Apply fluoride varnish to teeth twice yearly (2.2% NaF) [3]. due to having obvious active current caries
Further appointments highlighted the importance of educating the patient of their periodontal and caries status. A diet sheet was completed by the patient (Figure 2) and three teaspoons of honey in his tea (5-6 cups of a day) was identified (Table 5).
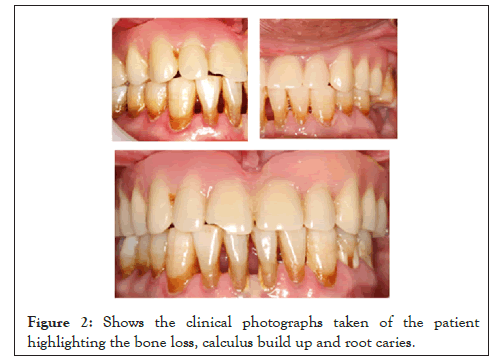
Figure 2: Shows the clinical photographs taken of the patient highlighting the bone loss, calculus build up and root caries.
When extracting the LR8, a blood glucose test was performed, from which the patient confessed he did not take his medication regularly. It was necessary to educate the patient about the importance of taking his medication for his oral health and general well-being. Review appointments showed the patient attempted to focus on managing Type 2 diabetes effectively in addition to improving plaque control in order to prevent new carious lesions and stabilise the periodontal condition.
The CAMBRA assessment was repeated after six months to assess the caries risk factor–see Table 6. As highlighted, the patient’s risk has been reduced to high risk due to the increase in protective factors and a decrease in disease indicators and environmental risk factors.
| Disease indicators | Check if Yes | ||
|---|---|---|---|
| 1. New cavities or lesion(s) into dentin (radiographically) | |||
| 2. New white spot lesions on smooth surfaces | |||
| 3. New noncavitated lesion(s) in enamel (radiographically) | |||
| 4. Existing restorations in last three years (new patient) or the last year (patient of record) | X | ||
| Biological or environmental risk factors | Check if Yes | ||
| 1. Cariogenic bacteria quantity not currently available | |||
| 2. Heavy plaque on the teeth | |||
| 3. Frequent snacking > 3 times daily) | |||
| 4. Hyposalivatory medications | X | ||
| 5. Reduced salivary function (measured low flow rate)** | |||
| 6. Deep pits and fissures | |||
| 7. Recreational drug use | |||
| 8. Exposed tooth roots | X | ||
| 9. Orthodontic appliances | |||
| Protective factors | Check if Yes | ||
| 1. Fluoridated water | X | ||
| 2. F toothpaste once a day | |||
| 3. F toothpaste 2X daily or more | X | ||
| 4. 5000 ppm F toothpaste | X | ||
| 5. F varnish last 6 months | X | ||
| 6. 0.05% sodium fluoride mouth rinse daily | X | ||
| 7. 0.12% chlorhexidine gluconate mouth rinse daily seven days monthly | |||
| 8. Normal salivary function | |||
| Column 1 | Column 2 | Column 3 | |
| Final Score: Yes in Column 1:Indicates high or extreme risk Yes in columns 2 and 3: Consider the caries balance ** Hyposalivation plus high risk factors=extreme risk |
 |
||
| Final overall caries risk assessment category (check) determined as per guidelines on next page EXTREME  HIGH HIGH  MODERATE MODERATE  LOW LOW |
|||
|
|||
Table 6: The patient’s CAMBRA outcome.
Results and Discussion
The patient has presented with a complex medical history, coupled with polypharmacy and uncontrolled diabetes, it is important to discuss how these aspects can affect the patient’s oral health.
The increase in the older population has resulted in root caries becoming a more prominent dental issue, as seen with the patient discussed in this case report. The patient had numerous root caries on the interproximal surfaces of his teeth, where it commonly presents due to factors such as microbial plaque, poor diet and decreased salivary flow. As this form of dental caries could also occur beneath the gingivae, it can prove difficult for some patients, including people with reduced dexterity like a proportion of the older population, to clean these areas by themselves. Increased risk has also been positively correlated with age and gingival recession, both of which are features of this patient [7].
There are number of other risk factors that contribute to root caries including properties of saliva (quality and quantity). Saliva provides key actions in keeping the oral cavity healthy including reducing the solubility of enamel, as well as buffering and neutralising acids ingested through diet and produced by the oral microflora [8].
Hyposalivation is a risk factor for root caries as the reduction in saliva leads to impaired oral clearance as well as difficulty regulating the processes of remineralisation and demineralisation of the enamel. As seen in Table 4, the patient in this case had a normal flow rate however, their buffer capacity both in unstimulated and stimulated saliva were very low being pH 4 and pH 3 respectively. Buffering capacity is an integral function of saliva. The resting pH of plaque is generally slightly acidic, becoming more acidic following the metabolism of carbohydrates during eating. Low saliva buffering capacity has been linked to being a potential risk factor for root caries in older adults due to increased enamel solubility. The buffering mechanisms of saliva, through phosphate, calcium and proteins, acts to restore the pH above the critical pH of 5.5 and back to neutral [9]. It might be worthwhile to analyse the composition of the saliva of patients with a reduced buffering capacity who present with root caries to investigate whether a reduction or an increase in certain compounds is a contributing factor to their condition.
The patient has a number of medical conditions including type 2 diabetes. Gingival recession could occur as a result of periodontal diseases in type 2 diabetes mellitus which exposes the root surfaces making the teeth more liable to root carious lesions. The patient also has acquired tooth loss due to chronic periodontitis and dental caries. In addition, wearing an upper complete acrylic denture might explain the reduced level of plaque control that could contribute to the development of dental caries on the root surfaces [10]. The two-way relationship between diabetes mellitus and periodontitis has been widely documented ergo the patient not managing their diabetes well may additionally be linked to their widespread root caries. Due to a shortage of thorough investigations into the link, more research is required to investigate if there is any direct association between diabetes and dental caries especially root caries.
The patient was on a number of different medications as listed in Table 1. Polypharmacy can have a number of different unwanted effects. Although not present with the patient in this case report, multiple medications could reduce the amount of saliva production through altered salivary gland function including drugs used to treat common conditions such as hypertension, hypercholesterolemia and asthma. Due to its aforementioned role in neutralising acids, a reduction in saliva may increase the risk of caries through decreased inhibition of bacterial growth. Another manner in which medications may lead to a higher risk of caries is if a person is on long-term medication containing sugars such as sucrose, glucose or fructose [11]. Changing to a sugar-free version could be recommended in these cases. As a result of the decreased antimicrobial actions that a number of medications would cause, a higher number of microorganisms may remain in the oral cavity due to reduced capability to prevent microbial aggregation as well as less clearance of substrates. If saliva composition is being affected by polypharmacy, it may compromise the remineralisation of the tooth leaving the root more susceptible to developing carious lesions.
Conclusion
This case highlighted the lack of understanding for the importance of managing medical conditions, emphasising the need to educate patients about how underlying diseases can affect their oral health, and how poor management can have serious complications. In addition, this report also emphasises the value of taking accurate drug histories and further investigations, allowing us to enhance our understanding on how factors such as the patient’s saliva components and polypharmacy could have an effect on their rampant root caries. As a summary, a greater emphasis should be placed on ensuring not only patients, but dental care professionals also need to be informed regarding health conditions and medications to provide a holistic care.
REFERENCES
- Featherstone JD, Chaffee BW. The evidence for caries management by risk assessment (CAMBRA®). Adv Dent Res. 2018;29(1):9-14.
- Implementing the 2017 Classification of Periodontal Diseases to Reach a Diagnosis in Clinical Practice. Br Society Periodontology; 2018.
- Public Health England. Delivering better oral health: an evidence-based toolkit for prevention.2017.
- Needleman I. The good practitioner’s guide to periodontology. Br Soc Periodontol. 2016:10-4.
- Horner K, Heaton K. Selection criteria for dental radiography standards. Faculty of General Dental Practitioners of the Royal College of Surgeons of England (FGDP). 2018.
- National Institute for Health and Clinical Excellence (NICE). Dental checks: intervals between oral health reviews. Clinical Guideline (CG19). 2004.
- Faine MP, Allender D, Baab D, Persson R, Lamont RJ. Dietary and salivary factors associated with root caries. Special Care in Dentistry. 1992;12(4):177-182.
- Mandel ID. Relation of saliva and plaque to caries. J Dent Res. 1974;53(2):246-266.
- Bardow A, Moe D, Nyvad B, Nauntofte B. The buffer capacity and buffer systems of human whole saliva measured without loss of CO2. Archives of Oral Biology. 2000;45(1):1-2.
- Hintao J, Teanpaisan R, Chongsuvivatwong V, Dahlen G, Rattarasarn C. Root surface and coronal caries in adults with type 2 diabetes mellitus. Community Dent Oral Epidemiol. 2007;35(4):302-309.
- Gati D, Vieira AR. Elderly at greater risk for root caries: a look at the multifactorial risks with emphasis on genetics susceptibility. Int J Dent. 2011.
Citation: Sawhney S, Ul Bariya Ali K, Mungur A, Baysan A (2021) The Association between Root Caries, Xerostomia and Blood Glucose in a Patient with Type 2 Diabetes. Diabetes Case Rep. 6:143.
Copyright: © 2021 Sawhney S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
