Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- ResearchBible
- China National Knowledge Infrastructure (CNKI)
- Scimago
- Ulrich's Periodicals Directory
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- MIAR
- Scientific Indexing Services (SIS)
- Euro Pub
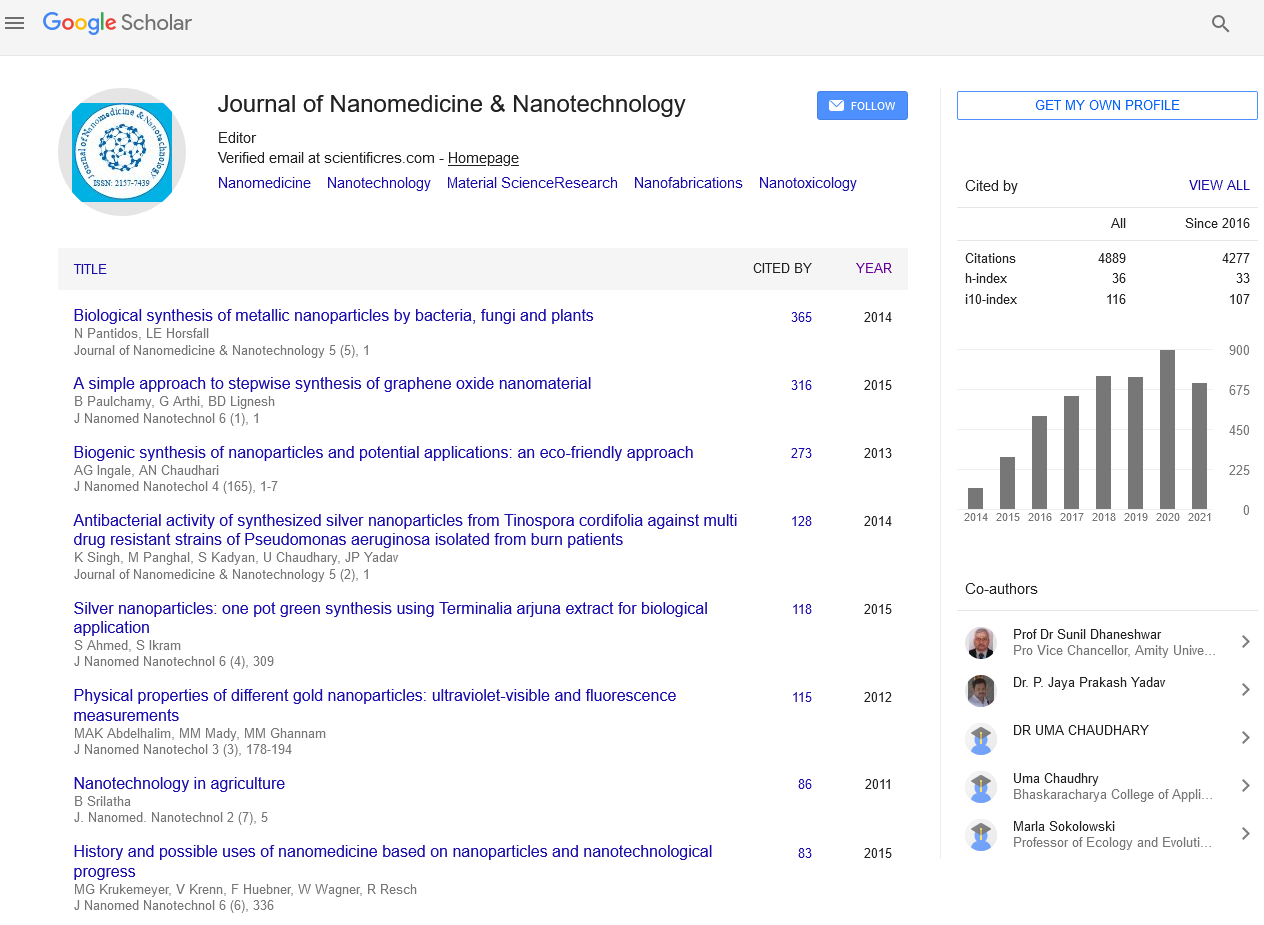
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2022) Volume 13, Issue 10
The Application of Nanotechnology in Microneedles for Drug Delivery
Mina Amir*Received: 03-Oct-2022, Manuscript No. jnmnt-22-18205; Editor assigned: 06-Oct-2022, Pre QC No. jnmnt-22-18205; Reviewed: 20-Oct-2022, QC No. jnmnt-22-18205; Revised: 24-Oct-2022, Manuscript No. jnmnt-22-18205; Published: 29-Oct-2022, DOI: 10.35248/2157-7439.22.13.641
Abstract
Microneedle (MN), a smart transdermal drug delivery system (TDDS), is a promising novel technology to deliver various drugs having different physicochemical properties. Such an approach and innovative technology attracted the attention of researchers worldwide to further study and discover the new technology due to the multiple advantages MN offers as it is a non-invasive TDDS with a fast onset of action besides sustained release properties. The combination of nanotechnology with microneedles’ technology presents an innovative and novel promising strategy aiming to merge the advantages of both technologies to allow safe and effective delivery with improved skin permeability of various drugs for the treatment, prevention, and diagnosis of various diseases. Several types of microneedles have been designed to improve patient compliance and reduce the dose frequency using the sustained release property, such as solid MNs, coated MNs, dissolving MNs, and hydrogel-forming MNs. In this review, we will discuss some examples from the previous research conducted on polymeric nanoparticles loaded microneedles, Lipidic nanoparticles loaded microneedles, metallic nanoparticles loaded microneedles, and nanocrystals loaded microneedles. In addition, we will discuss the applications of nanoparticles loaded microneedles in Vaccines, cancer, and diabetes. Lastly, we will present the main limitations to transfer the Nanoparticles loaded microneedles from bench to market.
Keywords
Microneedles; Metallic; Nanoparticles; Nanocrystals
INTRODUCTION
Over the past few years, Nanotechnology has been introduced to our research as well as our daily routine, such innovative technology is a key enabling technology, addressing unmet medical needs by offering and providing innovative medical solutions. Nanomedicine, the application of nanotechnology in the medical field, uses nanomaterials to monitor, diagnose, treat, and prevent targeted diseases. Due to the unique physicochemical properties of nanomaterials, their definition has been controversial. European Commission (EC) defined nanomaterials as materials having a size range, according to number size distribution, of 1-100 nm for ≥ 50% of particles and surface area to volume ratio ≥60 m2/ cm3, such materials could be manufactured, natural, or incidental In addition, the European medicine agency (EMA) also defined nanomedicines as newly targeted medical systems with at least one component within the nano-size range intended for clinical applications. Based on the EMA’s introduction of nanomedicine, the application of nanotechnology results in reproducible and unique characteristics as enhancing the targeting efficiency of drug delivery systems for the intended route of administration [1]. Although both EC and EMA established a clear introduction and definition of nanotechnology, Food and drug administration (FDA) didn’t give its definition of nanotechnology and/or nanomaterial, in addition, FDA usually advises the evaluation of nanotechnology in terms of safety, efficacy, and regulatory status due to the unique properties of nanotechnology [Table 1].
| Hypodermic Needles | Transdermal patches | Microneedles | Nanoparticles-loaded microneedles |
|
|---|---|---|---|---|
| Description | A hollow needle commonly used to inject the drug into the body |
Patches that adhere to the skin to deliver the drug | Micron-sized needles arranged on the surface of a small patch |
Micron-sized needles containing a nanoparticle-based drug delivery system arranged on the surface of a small patch |
| Mechanism of drug delivery to the skin | The needles go deep into the dermis layer, resulting in the delivery of 90%-100% of the drug, resulting in high drug bioavailability | The drug should cross the stratum corneum barrier, resulting in poor drug bioavailability | Bypass the stratum corneum barrier, resulting in direct 100% delivery of the drug to the epidermis or the upper dermis layer with sufficient drug bioavailability | Bypass the stratum corneum barrier, resulting in direct 100% delivery of the drug to the epidermis or the upper dermis layer with an extremely improved drug bioavailability due to either surface grafting of the designed nanoparticles or tuning the physicochemical properties of the designed nanoparticles |
| Onset of action | Fast | Slow | Fast | Fast |
| Pain | Invasive with poor patient compliance N.B: The pain receptors are present in the dermis layer in which the needle delivers the loaded drug. | Non-invasive, with appropriate patient compliance. |
Non-invasive with appropriate patient compliance. | Non-invasive with appropriate patient compliance. |
| Self-administration | Impossible | Possible | Possible | possible |
Table 1: Comparison between different Transdermal drug delivery systems as shown in figure (2)
Nanoparticle-based drug delivery systems can be administered via several routes of administration as oral administration, intravenous (IV) administration, parenteral administration, pulmonary administration, nasal administration, and ocular administration. The parenteral route of administration is known for its fast onset of action as well as the reduced dosage of the drug in comparison to that administered orally; furthermore, parenteral administration results in the direct administration of the drug in specific tissue and/or organ or the bloodstream directly. However, parenteral administration suffers poor patient compliance due to the usage of hypodermic needles resulting in severe pain, in addition, the usage of both needles and syringes results in increasing the disease transmission risk as some people tend to re-use needles besides increasing the medical waste burden. Such critical points resulted in the use and application of transdermal drug delivery systems (TDDS) as an alternative to parenteral administration, to enhance patient compliance [2].
The transdermal drug delivery system (TDDS), an alternative to hypodermic injection, is an attractive and promising tool for drug delivery. In 1979, the United States (US) approved the first TDDS, a three-day scopolamine-loaded TDDS for motion sickness treatment. A few years later, several transdermal patches were available in the market containing several APIs such as nicotine, Lidocaine, Estradiol, Fentanyl, and testosterone, intended for the treatment of multiple diseases. As shown in figure, the revolution in the TDDS field increased public attention to this attractive DDS and increased the TDDS profile in medicine, in comparison to the conventional DDS.
Microneedles (MNs), a smart transdermal drug delivery system (TDDS), have been deeply studied by various researchers worldwide as a TDDS tool for the delivery of wide scope of therapeutics ranging from low molecular weight therapeutics to vaccines in an attempt to overcome the skin permeation limitations faced by the previously mentioned conventional TDDS as the transdermal patches as well as hypodermic needles. The aim and gold standard of developing the smart microneedles’ technology is to allow disruption of stratum corneum (SC) by creating a micronsize transport pathway that is larger than that of the molecular dimensions and smaller in terms of size than the pores and/or holes formed by the hypodermic needles, hence increasing the skin permeability, and allowing large molecules to pass through SC. In comparison to the conventional TDDS, Microneedles show several advantages such as self- administration, fast onset of action, enhanced skin permeability, and improved drug bioavailability thus making it an attractive and promising TDDS [3] [Table 2].
| Material used | Fabrication method | Advantages | Limitations | References |
|---|---|---|---|---|
| Titanium | -Wet etching -Sintering process -Microelectrochemical systems (MEMS) |
Biocompatible Easy penetration to the skin |
-Complicated sintering process -Requires a clean room environment for microfabrication |
(21,30) |
| Stainless steel | -Sintering process -Electroplating -Electropolishing -Lithography Microstereolithography |
Biodegradable Store and protect gyroscopic drugs and biofluids extracts |
-Thick and rigid material -Complicated fabrication method |
(31) |
| silicon | -Electrochemical anodization -Etching -Lithography |
Biocompatible and biodegradable | -Limited MNs’ shape can be designed -Requires a clean room environment for microfabrication |
(32) |
| Bioceramics (CaS and CaP) | Mild Micro-moulding | Drug loading flexibility Drugs are added to the bioceramics before moulding |
Variation in the release of the drug because of the CaS and CaP water solubility |
(32) |
| Alumina | -Sintering process -Electrochemical anodization |
Tunable Porosity Strong mechanical properties | -Brittle -Non- biodegradable -The process requires heating at high temperatures |
(33–36) |
| Poly (lactic-co- glycolic acid) (PLGA) | Porogen leaching Moulding Emulsion and coating Hot embossing |
-Biocompatible and biodegradable -Tuneable Porosity through adjusting the porogen amount Used for the fabrication of dissolving MNs |
-A lengthy period of time for porogen removal -Expensive -Limited drug dose |
(37–39) |
| Polylactic acid (PLA) | fused deposition method (FDM) Emulsion and bonding Moulding | Biocompatible and biodegradable Rigid material (physically and chemically) High tensile strength |
-Complete removal of the organic solvent is required - Mechanical strength improvement is required -Expensive |
(40–42) |
| Cellulose acetate (CA) | -Phase inversion -Mould casting method |
Tuneable Porosity Tuneable mechanical strength Phase inversion method, a simple method, suitable for a wide type of polymers |
Usage of Dimethyl sulfoxide (DMSO) is toxic and harmful to the skin | (41,43) |
| Polydimethylsiloxane (PDMS) | -Porogen leaching -Micro-moulding -curing |
Tuneable Porosity through adjusting the Porogen amount | - A lengthy period for Porogen removal -Weak mechanical strength |
(41,44) |
| Poly (ethylene glycol-co- methacrylic acid) | -Phase separation -Bulk polymerization |
-Tuneable pore size -Mechanical strength |
|
(41,45) |
Table 2: Most common materials used in the fabrication of Microneedles arrays
The combination of nanotechnology with microneedles’ technology presents an innovative and novel promising strategy aiming to merge the advantages of both technologies to allow safe and effective delivery with improved skin permeability of various drugs having different physicochemical properties as well as improved and tuned sustained release effect.
• A non-invasive TDDS with a Sustained release property over a long period, resulting in the reduction of dosage frequency and the improvement of patient compliance.
• One or more Active Pharmaceutical Ingredients (APIs) with different physicochemical properties can be loaded within the nanoparticle-based drug delivery systems
• Protection of the loaded either single active pharmaceutical ingredient (API) or multiple APIs against physical, chemical, and proteolytic degradation, resulting in improving the stability of the encapsulated drug candidates.
• Elimination of the first pass metabolism in comparison to that of oral DDS. Resulting in the prolongation of drug residence time, increasing the half lifetime (T1/2), and reducing its body clearance.
• Increasing the drug’s bioavailability and targeting efficiency towards the intended site of action by either surface grafting of the designed nanoparticles or tuning the physicochemical properties of the designed nanoparticles, resulting in the reduction of the drug’s required dose hence reducing the possible toxicity as well as the possible side effects.
• Economical Noninvasive DDS can be self-administered easily compared to parenteral DDS, increasing the patient and reducing the possibility of disease transmission due to needle reuse in developing countries.
Universal Characteristics of Microneedle Arrays
Based on the type of microneedle and the material used in its fabrication, MNs are usually available in different sizes and shapes. MNs bypass the stratum corneum and deliver the drug directly into the epidermis which has a thickness equivalent to 1500 μm, as a result, MNs are usually designed with the following features and dimensions to avoid going in depth till reaching the dermis skin layer, rich in pain receptors, resulting in pain sensation due to their invasiveness as well as poor patient compliance [4]
• MNs length: 150 μm to 1500 μm
• MNs width: 50 μm to 250 μm
• MNs tip thickness: 1 μm to 25 μm
• MNs shapes: pointed, cylindrical, triangular, pentagonal, and octagonal.
MATERIALS USED FOR THE FABRICATION OF MICRONEEDLE ARRAYS
Polymer
Usually, both dissolving MNs arrays and hydrogel-forming MNs arrays are fabricated using polymeric materials. A wide range of polymers has been reported in the literature for the fabrication of MNs as Poly (lactic-co-glycolic acid) (PLGA), Polylactic acid (PLA), Polyglycolic acid (PGA), Poly (methyl methacrylate) (PMMA), Polystyrene, Polycarbonate, Polyvinyl alcohol (PVA), Polymethyl vinyl ether-co-maleic anhydride, and SU-8 Photoresist. In comparison to the other MNs fabricating material, Polymer-based MNs have less strength while stronger than both glass and ceramicbased MNs [5].
Carbohydrate
From a human health perspective, Carbohydrates are safe and economic materials, but they usually complicate the MNs’ fabrication process due to degradation at high temperatures. The most common carbohydrate used in MNs fabrication is Maltosewhile other carbohydrates can be used such as sucrose, galactose, mannitol, xylitol, trehalose, and polysaccharides. The carbohydrate-based MNs are fabricated as follows, with the aid of silicon or metal templates, slurries of carbohydrate are moulded, then to get the MN, the drug-loaded carbohydrate mixture is cast into the moulds [6]. Drug release in the skin is regulated by the time-based dissolution of the used carbohydrate.
Metal
Both Stainless steel and titanium are commonly used metals to fabricate metal-based MNs; stainless steel was the first metal used to fabricate MNs then researchers observed that Titanium is a good alternative to stainless steel. In addition, several metals such as palladium, palladium-cobalt, and nickel are also used as MNS fabricating materials. In comparison to the other materials used in the fabrication and production of MNs, Metal-based MNs are strong to prevent MNs’ breaking, thus more suitable for MNs fabrication than silicon.
Silicon
In 1990, the first MN was fabricated using silicon, versatile material, as it is a flexible material that allows the fabrication and batch production of multiple MNs of various sizes and shapes. The use of silicon to fabricate MNs is limited due to several factors as silicon is not only an expensive material but also a time-consuming material to fabricate MNs, resulting in a complicated MNs fabrication process. In addition, Silicon is known to be a brittle material, which could result in severe health issues as it could be broken directly after its application to the skin [7].
Silica glass
Boron silicate glass is commonly used, and it is composed of silica and boron trioxide. Although physiologically inert, Silica glass is known to be a brittle material. Nowadays, Silica glass-based MNs are only used for laboratory scale and/or experimental purposes and not for commercial applications.
Ceramic
Because of its chemical resistance, Alumina, Al2O3, is commonly used as it forms a stable oxide due to the covalent and ionic bonds between Aluminum and Oxygen atoms. In addition, several types of ceramics such as Gypsum, chemically known as calcium sulfate dihydrate (CaSO4 0.2H2O), and Brushite, chemically known as calcium phosphate dihydrate (CaHPO4.2H2O) are also used for the fabrication of ceramic-based MNs [8]. Recently, Ormocer, organically modified ceramic, has been used for the fabrication of ceramic-based MNs.
FABRICATION TECHNIQUES OF MICRONEEDLE ARRAYS
Various manufacturing techniques have been used to produce a wide scope of MNs; the selection of a specific manufacturing method depends on several factors such as the material used to produce and design the MN, the type of microneedle, and the geometry of the desired MN [Table 3].
| Type of MNs | Material used | Fabrication method | Advantages | Limitations |
|---|---|---|---|---|
| Solid MNs | silicon, stainless steel, titanium, nickel with polymers methyl vinyl ether polymethylmethacrylate, maleic anhydride, polycarbonate, maltose, Poly(lactide), Poly(lactide-co-glycolide) | microfabrication (micro- electromechanical system) and other methods such as using microreactors and micropumps | High mechanical strength resulting in skin piercing | Poor patient compliance |
| Coated MNs | Poly (lactic-co-glycolic acid) (PLGA), Polylactic acid (PLA), Polyglycolic acid (PGA), Polyvinyl alcohol (PVA), Titanium, Stainless steel |
The method used for MNs coating is spraying or dip coating, piezoelectric inkjet printing | Single step process | -a limited amount of drug can be coated on its surface (tip and shaft of the MN) |
| Hollow MNs | Ceramic, silicon, glass, Stainless steel, titanium, Poly (lactic-co- glycolic acid) (PLGA), Polylactic acid (PLA), Polyglycolic acid (PGA), Polyvinyl alcohol (PVA) | Microelectrochemical systems (MEMS) techniques, deep reactive ion etching of silicon, deep X-ray photolithography, wet chemical etching, an integrated lithographic moulding technique, and microfabrication, in the current era, the 3D printing method | -A high amount of the drug can be delivered -Controlled and accurate release of the loaded drug Easy and economical to manufacture |
-the possibility of needle tip clogging in the tissue and flow resistance due to compressed skin tissue’s density around the needle’s tip -Critical fabrication method and procedure - Uneconomic |
| Dissolving/ biodegradable MNS |
poly (propylene), dextrin, chondroitin sulfate, | solvent casting, droplet-born air blowing, laser machining, hot embossing, |
-The use of biodegradable | -upon long-term use, there is the possibility of |
Table 3: Types of Microneedles systems.
TYPES OF MICRONEEDLES SYSTEM
Microneedle devices are composed of arrays having needles within the micron range that bypass the stratum corneum without stimulating the dermal nerves, hence the holes created by the MNs in the skin are used to deliver the drug from the surface of the skin to the dermal microcirculation. There are 5 main types of MNs which are Solid MNs, Coated MNs, Hollow MNs, Dissolving MNs, and hydrogel-forming MNs.
Solid Microneedles
Solid MNs(without drug coating), poke and patch approach, are known to be applied either in a drug-free form or with a drug coating, Solid MNs without drug coating are used as a tool to create transient microchannel in the SC, skin piercing, by applying them directly to the skin followed by their removal. Such aqueous transient microchannels permeate the passive diffusion of the APIs loaded in multiple dosage forms and external reservoirs, such as cream, gel, transdermal patch, and solution. Besides their advantageous property in skin piercing, Solid MNs can also be coated with suitable yet desired drug formulations, resulting in fast delivery of the desired APIs, such an approach is limited by the therapeutic dose of the API usually less than 1 mg of the API is suitable to be applied at the base as well as the shaft of the MN removal.
Coated Microneedles
The manufacturing process of the coated MNs is mainly focused on first fabricating the solid MN followed by its coating with the desired drug formulation before being applied to the skin, Coated MNs, known for the Coat and poke approach, once inserted in the skin, the drug formulation first starts to dissolve continuously to be released into the skin. The use of this type of MN is limited by the therapeutic dose of the API as a limited amount of the drug can be coated on its surface, therefore limited for use in potent drug. In addition, coated MNs have been used to allow fast delivery of Deoxyribonucleic acid (DNA), proteins, peptides, and Vaccines.
Hollow Microneedles
The main difference between solid MNs and hollow MNs is the presence of internal lumen with a width ranging from 5 μm to 70 μm. Hollow MNs, known for the poke and flow approach, are commonly used for the delivery of vaccines and insulin as they continuously release the loaded drug in certain skin layers. The presence of an internal lumen or bore resulted in the flow of the loaded drug.
(10-100 μl/min) either through passive diffusion or through the application of certain pressure such as using a pump, syringe, or gas. In comparison to the other types of MNs [9], Hollow MNs show several advantages as the following:
• High amount of the drug can be delivered
• Controlled and accurate release of the loaded drug 3- Easy and economical to manufacture
Several interesting techniques concerning hollow MNs were studied as the incorporation of a micro pump or microfluidic chip to the Hollow MNs array resulting in a controlled release of the loaded drug, the integration of the drug reservoir with a heater resulting in either the spreading of the liquid drug formulation or the creation of bubbles to the skin and the application of pressure to the drug’s flexible reservoir resulting in the release of the loaded drug to the skin. Although Hollow MNs have several advantages in comparison to other MNs types, there are certain limitations as the possibility of needle tip clogging in the tissue and flow resistance due to compressed skin tissue’s density around the needle’s tip. Such limitations were overcome using certain strategies and techniques such as the gradual insertion of the hollow MN and the design of an off-centered holes side opening.
Dissolving/biodegradable Microneedles
Dissolving/biodegradable MNs, known for the poke and release approach, are composed of biocompatible polymers or carbohydrates. As shown in [Figure 1], Such soluble matrix is known to control the release of the loaded drug as the release kinetics depend on the dissolution degree of the soluble matrix, which is dissolved after contacting the interstitial fluid resulting in the release of the loaded API. Hence, to control the drug’s release kinetics, the formulator can either modify the manufacturing.
Figure 1: Three generations of Transdermal drug delivery system (TDDS).
Process or adjust the polymer or carbohydrate composition. Several researchers studied degradable MNs, a sub-type of dissolving MNs, to deliver a wide range of drugs with different physicochemical properties such as lidocaine, ibuprofen, caffeine, insulin heparin, and human growth hormone, and erythropoietin. In comparison to the other types of MNs, dissolving MNs show several advantages as the following:
• The use of biodegradable polymers or carbohydrate
• No sharp and bio-contaminated waste
• Economical manufacturing process using either semisynthetic Carbohydrates/polymers or synthetic Carbohydrates/ polymers
The main limitation of the dissolving MNs is that upon long-term use there is the possibility of polymers deposition in the skin
Hydrogel-forming microneedles
In 2010, Hydrogel-forming MNs were first described and designed. Hydrogel-forming MNs are composed of cross-linked polymers micro-extended from an API-loaded solid patch-like base. This type of MNs is fabricated using an aqueous mixture of certain polymers such as ultra-low viscosity carboxymethyl cellulose (CMC), amylopectin, and polymethyl vinyl ether-co-maleic acid (PMVE/ MA). As shown in [Figure 2], Hydrogel-forming microneedles, upon administration at the desired tissue, uptake the interstitial fluid followed by its swelling thus inducing the diffusion of the drug from the MN patch via swollen MNs, resulting in either sustained release or bolus release of the API. After being removed from the skin, Hydrogel-forming MNs leave no polymeric residues [Figure 3]. In addition, Upon modulating the hydrogel matrix’s density, drug delivery can be adjusted. Phase transition MNS, a subtype of the hydrogel- forming MNs, absorb the body’s fluid which results in polymer swelling and release of the API. In comparison to dissolving MNs, Hydrogel-forming MNs show a promising tool for TDDS as they neither dissolve nor degrade in the skin, thus leaving no polymeric residues and as a result, they do not cause harmful side effects, making them suitable for everyday use.
Figure 2: Drug delivery mechanism of the different transdermal drug delivery systems (Hypodermic needle, Transdermal patch, Microneedles, and Nanoparticles loaded microneedles) shows the following: • Hypodermic needles go deep into the dermis layer. • Transdermal patch’s drug should cross the stratum corneum barrier. • Microneedles and nanoparticles loaded Microneedles bypass the stratum corneum barrier, resulting in direct 100% delivery of the drug to the epidermis or the upper dermis layer
Figure 3: Poke and patch approach of the Solid Microneedles system adapted from (154).
Microneedles Loaded With Nanoparticles to Improve Drug Permeation
The combination of nanotechnology with microneedles’ technology presents an innovative and novel promising strategy aiming to merge the advantages of both technologies to allow safe and effective delivery with improved skin permeability of various drugs having different physicochemical properties as well as improved and tuned sustained release effect [Figure 4].
Figure 4: Coat and poke approach of the coated Microneedles system adapted from (154).
Polymeric nanoparticles loaded microneedles
Polymeric nanoparticles, including either polymeric nanocapsules or polymeric nanospheres, have been extensively studied and used as a drug delivery system for multiple body locations, by adjusting their size to be within the nano-size range as well as the surface charge. Polymeric nanoparticles used as TDDS can be categorized into two main groups based on the type of polymer used in the formulation which can be either natural or synthetic. Natural polymers such as chitosan, gelatin, alginate, and albumin; chitosan-based polymeric nanoparticles are commonly used as topical DDS for a wide range of therapeutics including plasmid DNA, oligonucleotides, retinol, and acyclovir. On the other hand, synthetic biodegradable polymers such as Poly (lactic-co-glycolic acid) (PLGA) are the most commonly used for the preparation of TDDS for the delivery of several therapeutics such as ketoprofen, indomethacin. As a transdermal DDS, polymeric nanoparticles are known to accumulate and penetrate the hair follicles rather than the SC [10]. Polymeric nanoparticles-loaded Microneedle (MN) have been reported in various publications [Figure 5]. Prepared Vitamin D3 encapsulated PLGA nanoparticles followed by their coating on stainless steel MN using the dip-coating method. In comparison to a transdermal cream using a Porcine skin cell model, Stainless steel MN coated with Vit D3 PLGA nanoparticles revealed successful and effective release and delivery of the vit D3 at the skin model while maintaining Vit D3 stability and causing no toxicity to the porcine skin cell model. Studied ketoprofenloaded PLA nanoparticles followed by their loading in solid silicon MN, resulting in enhancing the ketoprofen encapsulation efficiency along with extending and maintaining ketoprofen’s stability for 2 months. In an attempt to enhance Transdermal drug delivery, developed PLGA nanoparticles loaded with coumarin 6 and a fluorescent probe R-Phycoerythrin followed by their loading into MN. As shown in [Figure 6], Physicochemical characterization using confocal laser scanning microscopy revealed MN created micro conduits resulting in the delivery of coumarin 6 and R-Phycoerythrin-loaded PLGA nanoparticles to SC. In addition, the quantitative characterization demonstrated that after 48 hours of MN application to the skin, there is a 2-fold increase in the nanoparticles deposition in the SC in comparison to those of control, resulting in enhanced delivery of the desired drug candidates at the SC.
Figure 5: Poke and flow approach of the Hollow Microneedles system adapted from (154).
Figure 6: Poke and release approach of the dissolving Microneedles system adapted from (154).
To increase vaccine immunogenicity, encapsulated the silverspecific antigens in PLGA nanoparticles followed by their loading in dissolving MN, resulting in successful delivery and release of PLGA-loaded silver-specific antigens to the skin resulting in CD4 α and CD8 α activation besides IFN- γ secretion. Poly-caprolactone (PCL), a non-toxic and biodegradable polymer, is used as a drug delivery system for a wide range of therapeutics as it enhances the drug’s permeability across physiological barriers, enhances the drug’s efficiency, and minimizes the possible side effects. To develop anticancer and photothermal therapy, prepared 5-fluorouracil loaded and Indocyanine green-loaded Monomethoxy-poly (ethylene glycol) (MPEG)-PCL nanoparticles to respond to near-infrared rays followed by their loading into hyaluronic acid dissolving MN. The research group examined the efficacy of the designed 5 -fluorouracil loaded and Indocyanine green-loaded MN using A375 Cancer cells, resulting in an improved anti-cancer and photothermal therapy leading to cancer cell proliferation inhibition, improved efficacy of heat transfer, and tunable release of 5-fluorouracil. To extend the antibacterial effect at the site of infection, prepared carvacrol encapsulated PCL formulation followed by their loading into dissolving MN [Figure 7]. In comparison to the control group, Carvacrol loaded MN resulted in a sustained release of the antibacterial caracole with increased skin retention besides in 2-4 fold increase in the antibacterial activity leading to an effective wound healing.
Figure 7: Drug release approach of the Hydrogel forming Microneedles system adapted from (154).
REFERENCES
- Tinkle S, McNeil SE, Mühlebach S, Bawa R, Borchard G, Barenholz YC, et al. Nanomedicines: addressing the scientific and regulatory gap. Ann N Y Acad Sci. 2014; 1313(1): 35–56.
- Pita R, Ehmann F, Papaluca M. Nanomedicines in the EU—Regulatory Overview. AAPS Journal. 2016; 18(6):1576–1582.
- Bleeker EAJ, de Jong WH, Geertsma RE, Groenewold M, Heugens EHW, Koers- Jacquemijns M, et al. Considerations on the EU definition of a nanomaterial: Science to support policy making. Regul Toxicol Pharmacol. 2013; 65(1):119–125.
- European commission recommendation. Commission Recommendation of 18 October 2011 on the definition of nanomaterial Text with EEA relevance.
- European Commission. Directorate General for Health & Consumers.
- Opinion on 4-Nitrophenyl aminoethylurea : COLIPA n° B70. European Commission; 2010; 29.
- Administration D. Guidance for Industry Considering Whether an FDA-Regulated Product Involves the Application of Nanotechnology Contains Nonbinding Recommendations [Internet]. 2014.
- Soares S, Sousa J, Pais A, Vitorino C. Nanomedicine: Principles, properties, and regulatory issues. Front Chem 2018; 6:360.
- Baetke SC, Lammers T, Kiessling F. Applications of nanoparticles for diagnosis and therapy of cancer. Br J Radiol. 2015; 88(1054):2015-2207.
- Zhang J, Xie Z, Zhang N, Zhong J. Nanostructures for Drug Delivery NANOSUSPENSION DRUG DELIVERY SYSTEM: PREPARATION, CHARACTERIZATION, POSTPRODUCTION PROCESSING, DOSAGE FORM, AND APPLICATION. 2017; 413-443
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Amir M (2022) The Application of Nanotechnology in Microneedles for Drug Delivery. J Nanomed Nanotech. 13: 641.
Copyright: ©2022 Amir M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.