Indexed In
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2021) Volume 5, Issue 5
Subtenon Block with 1% Ropivacaine and 0.75% Bupivacaine for Cataract Surgery: A Randomized, Double-Blind Clinical Trial
Diego Campos da Rocha David1, Denismar Borges de Miranda2*, Marco Aurelio Soares Amorim1, Adriana de Oliveira Cordeiro1, Jose Fernando Bastos Folgosi1, Larissa Goveia Moreira3 and Catia Sousa Goveia32Municipal Health Department of Goiania, Goias Federal University, Goias, Brazil
3Department of Anesthesiology, University of Brasília, Brasília, Federal District, Brazil
Received: 16-Sep-2021 Published: 07-Oct-2021, DOI: 10.35248/2684-1606.21.5.156
Abstract
Background: Cataract surgery is the most frequent operation performed in Ophthalmology, and the subtenon block is one of the executed modalities of regional anesthesia. This study aims to compare the quality of anesthesia between ropivacaine and racemic bupivacaine in the subtenon block for cataract surgeries with phacoemulsification technique.
Methods: Clinical trial, randomized and double-masked, comparing the quality of anesthesia of 1% ropivacaine (GR) and 0.75% racemic bupivacaine with epinephrine (GB) under subtenon block for cataract surgery. Sample with 64 patients, 32 randomly assigned to GR and 32 in GB. All blockages were performed with 5 mL solution added with 40 IU/mL hyalurunidase. Motor akinesia, intraocular pressure, ocular perfusion pressure, analgesia, sedation level and anthropometric characteristics were evaluated. Student’s t tests, chi-square (χ2) and Mann-Whitney U were applied to evaluate differences between the groups, with 5% significance level.
Results: No difference was found in the demographic and clinical baseline characteristics between the groups. Early satisfactory motor block (5 minutes) was observed in GR (p=0.035). Within 10 minutes, akinesia was found to be adequate in 84.3% of GR and only in 62.5% of GB (p=0.048). The GR showed lower latency and better motor akinesia compared to GB. Secondary outcomes with no difference between groups.
Conclusion: The subtenon block is effective for cataract surgery. 1% ropivacaine presented satisfactory motor akinesia in 10 minutes and lower latency when compared to bupivacaine 0.75%.
Keywords
Su btenon block; Ropivacaine; Bupivacaine; Cataract surgery; Clinical trial
Abbreviations
GB: Bupivacaine Group; GR: Ropivacaine Group; IOP: Intraocular Pressure; MBP: Mean Blood Pressure; OCR: Oculocardiac Reflex; OPP: Ocular Perfusion Pressure; SD: Standard Deviation; VAS: Visual Analog Scale.
Introduction
One of the most frequently performed operations in ophthalmology is facectomy by phacoemulsification and intraocular lens implantation. Several anesthetic techniques are described for this operation. The loco-regional blocks [intraconal, extraconal and subtenon) are widely performed because they provide excellent sensory block and ocular akinesia [1,2].
The subtenon block was described by Turnbull in 1884 and popularized by Stevens in 1992, after demonstrating its effectiveness as a single anesthetic technique. It is also known as either parabulbar or episcleral block. It has been used more frequently due to its effective akinesia and intraoperative analgesia comparing to other regional anesthesia techniques. The blockade consists in the local anesthetic administration in the episcleral space, under the Tenon’s capsule, with atraumatic cannulae or needles [3-6].
When the local anesthetic is injected into the episcleral space, it diffuses into the retrobulbar space, the optic nerve sheath and the ciliary nerves, leading to rapid analgesia. As there is continuity between the eyeball fascial sheath and the rectus sheaths, the anesthetic diffuses up to the terminal motor nerves, and produces excellent eye akinesia. It was demonstrated by computed tomography that 4 mL of local anesthetic are sufficient to involve the whole globe and produce akinesia after a single injection. However, other authors have demonstrated a better quality of blockade and postoperative analgesia for vitrectomies with the use of 10 mL of local anesthetic after double injection, compared to 5 mL single injection [7].
Local anesthetics promote motor block in different degrees and latencies according to the concentrations and volumes used. It is also important to evaluate akinesia and Intraocular Pressure (IOP), as they vary according to the anesthetic. Racemic bupivacaine is still widely used in cataract surgery, although its cardiotoxicity is scientifically established. Therefore, anesthetics with a lower degree of cardiac toxicity, such as ropivacaine, must be encouraged. In subtenon block, the local anesthetic with the best performance and the least potential for adverse effects wasn’t still determined in the scientific literature. Thus, this study aims to compare the quality of subtenon anesthesia between racemic bupivacaine and ropivacaine in cataract surgery [8].
Methodology
This is a randomized, double-masked clinical trial. Cataract patients were admitted to a referenced hospital in ophthalmology in Goiania, Goias, Brazil, to undergo cataract surgery by phacoemulsification with intraocular lens implantation. They were previously invited to participate in the study. The study was carried out from September to December 2016. The research was approved by the Ethics Committee under the protocol of approval n° 58192716.7.0000.0035, according to Resolution n° 466 of the Ministry of Health; all patients signed the Informed Consent Form and are in line with the Declaration of Helsinki.
It was estimated that the study should have 80% power to test the hypothesis at a significance level of 5% and success rate of 34% (bupivacaine compared to ropivacaine), as already identified in a previous study that compared the same medications in a regional block. The calculated sample consisted of 52 patients randomly assigned in two groups (1% ropivacaine group-GR and 0.75% racemic bupivacaine group-GB) using the four block randomization technique. The masked allocation was maintained by means of a sealed brown envelope [9].
Participants were considered eligible if attended the following criteria: age between 18 and 75 years; physical state I, II or III according to the American Society of Anesthesiologist’s criteria; and candidates to cataract surgery under Subtenon block. Participants were excluded if they exhibited allergy to local anesthetic, glaucoma, abnormal eye movement, chronic cough, anticoagulant therapy, orbital abnormalities, and inability to understand the study or block failure.
In this study, the primary endpoint was the quality of motor blockade (degree of akinesia), evaluated by Nicoll’s score in three moments (T0-beginning, T5-5 minutes and T10-10 minutes) after subtenon block. The intensity of akinesia was assesed by eye movement in four hypothetical quadrants, ranging from 0 to 8. It was considered proper akinesia if the score >6 [10].
The secondary endpoints considered were: sedation level (Ramsay Sedation Scale), IOP-evaluated by a manual applanation tonometer, Ocular Perfusion Pressure (OPP)-calculated by the difference between Mean Blood Pressure (MBP) and IOP, postoperative analgesia-assessed by visual analog scale (VAS) 30 minutes after the end of the surgery and 24 hours after the blockade (presence of pain if VAS ≥ 1), and adverse effects such as bradycardia (decreased heart rate above 20% of pre- blocking values), hypotension (defined as mean arterial pressure decrease higher than 20% of pre-blocking values) and hypoxia (SpO2 <90%) during operation. These outcomes were compared between the groups [11-14].
After peripheral venous puncture with 22 G catheter, nasal catheter was installed for oxygen administration with a flow rate of 2 L/minute. IOP, ocular motility, heart rate, noninvasive blood pressure and pulse oximetry were measured during T0. Sedation was performed intravenously with propofol (0.4 mg/kg) and fentanyl (20-30 micrograms) before subtenon block.
Subtenon block was administered according to a standard technique with a 20 G needle in the medial canthus. For GR, 5 mL of 1% ropivacaine was administered, for GB, 5 mL of 0.75% bupivacaine with epinephrine 1:200.000. In both groups, hyalorunidase was added 40 IU per milliliter of anesthetic solution.
The researcher DCDR was responsible for performing all subtenon blocks. AOC, a different and veiled researcher, was responsible for assessing the patients during the pre, intra and postoperative periods. All patients were unaware of their allocation group.
Statistical analysis was performed using a commercially available statistical software package (SPSS for Mac, V.22.0, IBM-SPSS, Chicago, Illinois, USA). Mean and Standard Deviation (SD) were calculated. The test of normal distribution of variables was calculated by the Kolmogorov-Smirnov test. Differences between the groups were assessed by Student’s t test, chi-square test (χ2) and Mann-Whitney U test. Statistical significance was considered as p<0.05.
Results
Sixty-seven patients were considered eligible and agreed to participate. Two patients undergoing anticoagulant therapy and one who failed sensory blockade (later supplemented with peribulbar anesthesia) were excluded. Sixty-four patients were evaluated and submitted to subtenon block as anesthetic technique for cataract surgery Figure 1. The demographic and clinical characteristics of the patients were similar in both groups (Table 1), except for the IOP value before the procedure. However, the difference in this data has no clinical significance, since the values remained within normal limits. The most common clinical comorbidities were hypertension and diabetes mellitus. Other comorbidities were chronic obstructive pulmonary disease, osteoporosis, osteoarthrosis, and acquired immunodeficiency syndrome.
| Features | Groups | p value | ||
|---|---|---|---|---|
| Ropivacaine (n=32) | Bupivacaine (n=32) | |||
| Demographic | ||||
| Sex | 0.453* | |||
| Male | 14 (43.75%) | 17 (53.12%) | ||
| Female | 18 (56.25%) | 15 (46.88%) | ||
| Age (years) | 65.94 ± 8.73 | 65.63 ± 9.76 | 0.893† | |
| Weight (Kg) | 67.91 ± 13.89 | 66.59 ± 10.69 | 0.673† | |
| Height (cm) | 161 ± 10.53 | 162 ± 8.81 | 0.617† | |
| Clinical | ||||
| Comorbities | 0.168* | |||
| No | 3 (9.38%) | 7 (21.88%) | ||
| Yes | 29 (90.62%) | 25 (78.12%) | ||
| Arterial Hypertension | 22 (68.75%) | 18 (56.25%) | 0.302* | |
| Diabetes mellitus | 6 (18.75%) | 5 (15.62%) | 0.740* | |
| Others | 5 (15.62%) | 6 (18.75%) | 0.740* | |
| Physical State (ASA) | 0.143* | |||
| 1 | 3 (9.38%) | 8 (25.00%) | ||
| 2 | 21 (65.62%) | 14 (43.75%) | ||
| 3 | 8 (25.00%) | 10 (31.25%) | ||
| IOP (mmHg) | 12.66 ± 1.45 | 13.94 ± 1.76 | 0.002† | |
| OPP (mmHg) | 83.17 ± 10.57 | 85.60 ± 10.70 | 0.367† | |
| SBP (mmHg) | 132.63 ± 14.38 | 135.78 ± 15.32 | 0.399† | |
| DBP (mmHg) | 77.44 ± 9.21 | 81.41 ± 9.52 | 0.095† | |
| MAP (mmHg) | 95.83 ± 9.94 | 99.53 ± 10.37 | 0.150† | |
| HR (bpm) | 72.41 ± 10.99 | 69.03 ± 13.79 | 0.283† | |
| SpO2 (%) | 97.0 ± 2.06 | 97.1 ± 1.95 | 0.852† | |
| Ramsay | 2 (1-2) | 2 (1-2) | 0.691‡ | |
Data are presented in absolute and relative frequency (%), mean ± standard deviation and median (minimum-maximum), when applicable. *Statistical analysis performed using the χ2 test; † Statistical analysis performed with the Student t test; ‡ Statistical analysis performed with the Mann-Whitney U test; ASA, physical state according to criteria of the American Society of Anesthesiologists; IOP- Intraocular Pressure; OPP-Ocular Perfusion Pressure; SBP-Systolic Blood Pressure; DBP-Diastolic Blood Pressure; MAP- Mean Arterial Pressure; HR- Heart Rate; SpO2-Oxygen Saturation in the Blood.
Table 1: Baseline characteristics of patients submitted to subtenon block with 1% ropivacaine and 0.75% bupivacaine.
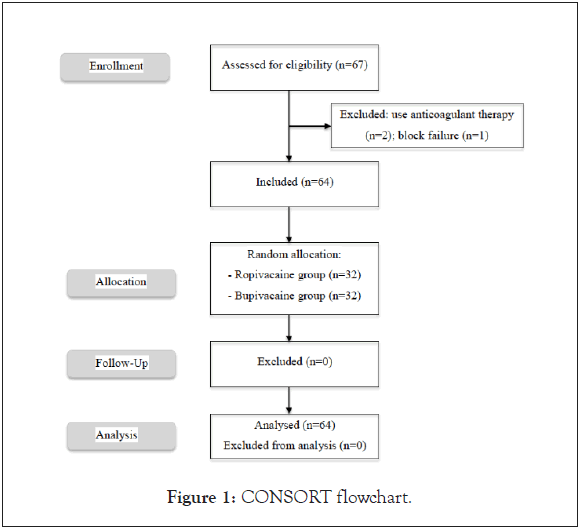
Figure 1: CONSORT flowchart.
The primary and secondary endpoints are shown in Table 2. In ocular akinesia evaluation, a higher frequency of early adequate motor block (T5) was observed in GR compared with GB (p=0.035). At T10, 84.38% of GR had adequate akinesia compared to 62.50% of GB (p=0.048). In both groups, it was observed an increase in IOP compared to the basal value (T0), for T5 (difference in GR=3.28 ± 0.85 vs. GB=1.31 ± 0.89, p=0.000) and T10 (difference in GR=2.78 ± 1.01 vs. GB=0.66 ± 0.93, p=0.000), higher in GR, with statistical significance. Statistically significant differences between the groups were also observed in IOP evaluation at T10 (GR=15.44 ± 1.52 vs. GB=14.59 ± 1.79, p=0.047) and SpO2 in T5 (GR=96.69 ± 1.84 vs. GB=97.63 ± 1.52, p=0.030). However, such differences have no clinical repercussions. The other clinical characteristics had no difference between the groups.
| Clinical characteristics | Groups | p-value | |
|---|---|---|---|
| Ropivacaine (n=32) | Bupivacaine (n=32) | ||
| Akinesia | |||
| T5 | 0.035* | ||
| Inappropriate | 17 (53.12%) | 25 (78.12%) | |
| Appropriate | 15 (46.88%) | 7 (21.88%) | |
| T10 | 0.048* | ||
| Inappropriate | 5 (15.62%) | 12 (37.50%) | |
| Appropriate | 27 (84.38%) | 20 (62.50%) | |
| IOP (mmHg) | |||
| T0 | 12.66 ± 1.45 | 13.94 ± 1.76 | 0.002† |
| T5 | 15.94 ± 1.68 | 15.25 ± 1.85 | 0.125† |
| T10 | 15.44 ± 1.52 | 14.59 ± 1.79 | 0.047† |
| T5-T0 | 3.28 ± 0.85 | 1.31 ± 0.89 | 0.000† |
| T10-T0 | 2.78 ± 1.01 | 0.66 ± 0.93 | 0.000† |
| OPP (mmHg) | |||
| T0 | 83.17 ± 10.57 | 85.60 ± 10.70 | 0.367† |
| T5 | 78.02 ± 10.96 | 81.48 ± 13.69 | 0.269† |
| T10 | 79.39 ± 8.99 | 80.17 ± 12.59 | 0.770† |
| T5-T0 | -5.16 ± 9.09 | -4.11 ± 12.35 | 0.702† |
| T10-T0 | -3.78 ± 6.90 | -5.43 ± 9.18 | 0.421† |
| SBP (mmHg) | |||
| T5 | 130.06 ± 13.20 | 134.00 ± 18.96 | 0.339† |
| T10 | 130.06 ± 11.55 | 131.97 ± 18.93 | 0.629† |
| DBP (mmHg) | |||
| T5 | 75.91 ± 10.55 | 78.09 ± 11.68 | 0.435† |
| T10 | 77.22 ± 8.62 | 76.16 ± 10.54 | 0.661† |
| MAP (mmHg) | |||
| T5 | 93.96 ± 10.50 | 96.73 ± 13.25 | 0.357† |
| T10 | 94.83 ± 8.71 | 94.76 ± 12.00 | 0.978† |
| HR (bpm) | |||
| T5 | 72.25 ± 11.45 | 70.97 ± 13.69 | 0.686† |
| T10 | 71.22 ± 10.98 | 70.16 ± 12.40 | 0.718† |
| SpO2 (%) | |||
| T5 | 96.69 ± 1.84 | 97.63 ± 1.52 | 0.030† |
| T10 | 97.28 ± 1.63 | 97.19 ± 1.45 | 0.809† |
| Ramsay | |||
| T5 | 3 (2-4) | 4 (3-5) | 0.199‡ |
| T10 | 2 (2-3) | 2 (2-3) | 0.317‡ |
| Pain | |||
| 10 min | 1.000* | ||
| No | 31 (96.88%) | 31 (96.88%) | |
| Yes | 1 (3.12%) | 1 (3.12%) | |
| 24 h | 0.152* | ||
| No | 24 (75.00%) | 19 (59.38%) | |
| Yes | 6 (25.00%) | 11 (34.38%) | |
Data are presented in absolute and relative frequency (%); mean ± standard deviation and median (minimum-maximum), when applicable. *Statistical analysis performed using the χ2 test; † Statistical analysis performed with the Student t test; ‡Statistical analysis performed with the Mann-Whitney U test; T0, baseline evaluation; T5, five minutes after the block; T10, ten minutes after the block; IOP- Intraocular Pressure; OPP- Ocular Perfusion Pressure; SBP- Systolic Blood Pressure; DBP- Diastolic Blood Pressure; MAP- Mean Arterial Pressure; HR- Heart Rate; SpO2-Oxygen Saturation in the Blood.
Table 2: Clinical characteristics among patients submitted to subtenon block with 1% ropivacaine and 0.75% and bupivacaine.
There was no difference regarding the occurrence of adverse events between the groups (Table 3). However, there was a higher rate of bradycardia in GB when compared to GR (p=0.030), regardless of the presence of preexisting comorbidities (Table 4).
| Adverse events | Groups | No | P value |
|---|---|---|---|
| No | 22 (68.7% 5) | 16 (50.00 %) | 0.127 |
| Yes | 10 (31.25 %) | 16 (50.00 %) | |
| Bradycardia | 3 (8 9.3%) | 10 (31.25%) | 0.03 |
| Chemosis | 5 (15.6 2 %) | 1 (3.1 2%) | 0.086 |
| Arterial hypertension | 1 (3.1 2%) | 2 (6.2 5 %) | 0.554 |
| Arterial hypotension | 0 (0.001 %) | 2 (6.2 5 %) | 0.151 |
| Periorbital hyperemia | 0 (0.00 %) | 1 (3.1 2%) | 0.313 |
| Hypoxia | 1 (3.1 2%) | 0 (0.00 %) | 0.313 |
The data is presented in absolute and relative frequency (%). Statistical analysis performed using the χ2 test.
Table 3: Adverse events among patients submitted to subtenon block with 1% ropivacaine and 0.75% bupivacaine.
| Previous comorbities | Bradycardia | P-value | |
|---|---|---|---|
| No (n=51) | Yes (n=13) | ||
| Hypertension | 0.229 | ||
| No | 21 (41.18%) | 3 (23.08%) | |
| Yes | 30 (58.82%) | 10 (76.92%) | |
| Diabetes mellitus | 0.847 | ||
| No | 42 (82.35%) | 11 (84.62%) | |
| Yes | 9 (17.65%) | 2 (15.38%) | |
| Others | 0.528 | ||
| No | 43 (84.31%) | 10 (76.92%) | |
| Yes | 8 (15.69%) | 3 (23.08%) | |
The data are presented in absolute and relative frequency (%). Statistical analysis performed using the χ2 test.
Table 4: Confounding factors for bradycardia among patients submitted to subtenon block with 1% ropivacaine vs. 0.75% bupivacaine.
Discussion
In this study, the subtenon block provided anesthesia with excellent quality for cataract surgery. It demonstrated to be an efficient and safe technique in ophthalmic surgery without the potential complications of either peribulbar or retrobulbar anesthesia [15,16].
The demand for drugs with lower latency and toxicity, and better pharmacokinetic profile has been an important issue for researchers. Comparative studies between ropivacaine and bupivacaine in supraclavicular blocks and labor analgesia did not show differences in the quality of sensory and motor blocks. In the peribulbar block it was evidenced the same degree of motor block and variation in IOP. In a study comparing levobupivacaine and ropivacaine in peribulbar anesthesia for cataract surgery, there was better akinesia with levobupivacaine, but with no clinical significance. In our study, ropivacaine showed better motor akinesia and lower latency compared to bupivacaine in subtenon anesthesia, in agreement with another study about peribulbar block [12,17-20].
The volume of 5 ml of anesthetic caused no significant variation of IOP in the groups, since it remained within normal limits. As presented in other studies, there was an expected initial increase (T5) followed by a reduction (T10) of IOP, in both groups 12, 20, 21. This IOP reduction is explained by three reasons: vasoconstriction provided by anesthetics, relaxation of extraocular muscles and reduction in aqueous humor production by ciliary ganglion blockade. Ropivacaine resulted in higher IOP values. It is known that the local anesthetics lipid solubility alters the calcium channels and produces a vasoconstrictor effect. The addition of adrenaline to bupivacaine may have intensified the vasoconstriction and contributed to the greater IPO decrease in this group. However, these differences do not mean clinical repercussion, since variation remained in a short range.
Another factor that may have contributed to the decrease in IOP is the level of sedation. Opioids and hypnotics, such as fentanyl and propofol, reduce aqueous humor production, depress the central nervous system, decrease arterial and venous pressures of the eyeglobe, and promote extraocular muscle relaxation. This was probably not a determining factor for the difference in IOP between groups, as there was no difference in sedation level between the groups [21].
Bradycardia may occur due to Oculocardiac Reflex (OCR), the vagal stimulation in response to globe compression or stretching of the extraocular and conjunctival musculature. Also, local anesthetics may also depress atrial contractility and cardiac excitability, leading to bradycardia or even cardiopulmonary arrest with difficult resuscitation. It’s known that the subtenon anesthesia does not reduce the incidence of OCR in strabismus surgery. This study showed bradycardia as the most common adverse event in both groups, especially with bupivacaine. The presence of previous comorbidities did not influence this data, suggesting that bupivacaine has a higher cardiac toxicity than ropivacaine. The observed bradycardia may not be related to the typical vagal response of OCR, mainly because the subtenonian technique does not determine a significant increase of IOP [22-25].
The study could have added adrenaline to both groups, avoiding a biased analysis of IOP. More studies are needed to evidence the effective volume and concentration of local anesthetics in subtenon block.
Conclusion
It has been shown that subtenon block is effective for cataract surgeries, providing excellent anesthesia and rare complications. Among anesthetics, 1% ropivacaine has better motor akinesia and lower latency when compared to 0.75% racemic bupivacaine. Bradycardia is more common in patients exposed to bupivacaine, confirming its higher cardiac toxicity.
Contributions
DCRD, MASA and AOC collected the patient’s information drafted this manuscript and made contribution to supervision and final approval, and DBM and CSG analyzed and interpreted the patient data, and final approval. All authors read and approved the final manuscript.
Acknowledgements
The Goias Eye Bank Foundation Hospital.
REFERENCES
- Malik A, Fletcher EC, Chong V, Jay, D. Local anesthesia for cataract surgery. J Cataract Refract Surg. 2010; 36: 133-152.
- El-Hindy N, Johnston RL, Jaycock P, Eke T, Braga AJ, Tole DM, et al. The cataract national dataset electronic multi-centre audit of 55,567 operations: anaesthetic techniques and complications. Eye. 2009; 23: 50-55.
- Stevens JD. A new local anesthesia technique for cataract extraction by one quadrant sub-Tenon’s infiltration. Br J Ophthalmol. 1992; 76: 670-674.
- Greenbaum S. Parabulbar anesthesia. Am J Ophthalmol. 1992; 114: 776.
- Ripart J, Metge L, Prat-Pradal D, Lopez FM, Eledjam. Medial canthus single-injection episcleral (sub-tenon anesthesia): computed tomography imaging. Anesth Analg. 1998; 87: 42-45.
- Kumar CM, Eid H, Dodds C. Sub-Tenon’s anaesthesia: Complications and their prevention. Eye. 2011; 25: 694-703.
- Gill VS, Presland AH, Lord JA, Bunce C, Xing W, Charteris DG. Two-quadrant high-volume sub-Tenon’s anaesthesia for vitrectomy: a randomised controlled trial. Br J Ophthalmol. 2012; 96: 189-192.
- Foster RH, Markham A. Levobupivacaine: A review of its pharmacology and use as a local anaesthetic. Drugs. 2000; 59(3): 551-579.
- Ogun CO, Kirgiz EN, Duman A, Okesli S, Akyurek C. Comparison of intrathecal isobaric bupivacaine-morphine and ropivacaine-morphine for caesarean delivery. Br J Anaesth. 2003; 90(5): 659-664.
- Nicoll JM, Treuren B, Acharya PA, Ahlen K, James M. Retrobulbar anesthesia: The role of hyaluronidase. Anesth Analg. 1986; 65(12): 1324-1328.
- Consales G, Chelazzi C, Rinaldi S, De Gaudio AR. Bispectral index compared to Ramsay score for sedation monitoring in intensive care units. Minerva Anestesiol. 2006; 72(5): 329-336.
- Magalhaes E, Goveia CS, Oliveira KB. Racemic bupivacaine, levobupi vacaine and ropivacaine in regional anesthesia for ophthalmology - a comparative study. Rev Assoc Med Bras. 2004; 50(2):195-198.
- Hayreh SS. Blood flow in the optic nerve head and factors that may influence it. Prog Retin Eye Res. 2001; 20(5): 595-624.
- Yazbeck-Karam VG, Siddik-Sayyid SM, Abi Nader EL, Barakat DE, Karam HS, Cherfane GM, et al. Supplementation of retrobulbar block with clonidine in vitreoretinal surgery: Effect on postoperative pain. J Clin Anesth. 2011; 23(5): 393-397.
- Amin S, Minihan M, Lesnik-Oberstein S. A new technique for delivering sub-tenon’s anaesthesia in ophthalmic surgery. Br J Ophthalmol. 2002; 86(1): 119-120.
- Guise PA. Sub-tenon anesthesia: A prospective study of 6,000 blocks. Anesthesiology. 2003; 98: 964-968.
- Venkatesh RR. A Randomized controlled study of 0.5% bupivacaine, 0.5% ropivacaine and 0.75% ropivacaine for supraclavicular rrachial plexus block. J Clin Diagnostic Res. 2016; 10: 90-93.
- Dresner M, Freeman J, Calow C, Quinn A, Bamber J. Ropivacaine 0.2% versus bupivacaine 0.1% with fentanyl: a double blind comparison for analgesia during labour. Br J Anaesth. 2000; 85(6): 826-829.
- Borazan M, Karalezli A, Akova YA, Algan C, Oto S. Comparative clinical trial of topical anaesthetic agents for cataract surgery with phacoemulsification: lidocaine 2% drops, levobupivacaine 0.75% drops, and ropivacaine 1% drops. Eye (Lond). 2008; 22(3): 425-429.
- Serzedo PSM, Nociti JR, Zuccolotto EB, Cagnolati CA, Nunes AMM. Ropivacaína em bloqueio peribulbar: estudo comparativo com bupivacaína. Rev Bras Anestesiol. 1998; 48(4): 258-263.
- Govêia CS, Magalhãe E. Anestesia peribulbar com ropivacaína: estudo da ação vasoconstritora. Rev Bras Anestesiol. 2010; 60(5): 495-512.
- Bhattacharjee A, Rajaram P, Khatua A. Two Episodes of trigeminocardiac reflex during a pan facial fracture surgery, a rare phenomenon - case report and review of literature. J Clin Diagn Res. 2017; 11: 1-3.
- Bardsley H, Gristwood R, Baker H, Watson N, Nimmo W. A comparison of the cardiovascular effects of levobupivacaine and rac-bupivacaine following intravenous administration to healthy volunteers. Br J Clin Pharmacol. 1998; 46(3): 245-249.
- Tuzcu K, Coskun M, Tuzcu EA. Effectiveness of sub-tenon’s block in pediatric strabismus surgery. Rev Bras Anestesiol. 2015; 65: 349-352.
- Mather CM. Comparison of i.v. cannula and Stevens’ cannula for sub-tenon’s block. Br J Anaesth. 2007; 99: 421-424.
Citation: David DCDR, Miranda DBD, Amorim MAS, Cordeiro ADO, Folgosi JFB, Moreira LG, et al. (2021) Subtenon Block with 1% Ropivacaine and 0.75% Bupivacaine for Cataract Surgery: A Randomized, Double-Blind Clinical Trial. J Surg Anesth. 5:156.
Copyright: © 2021 David DCDR, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
