Indexed In
- Open J Gate
- Cosmos IF
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
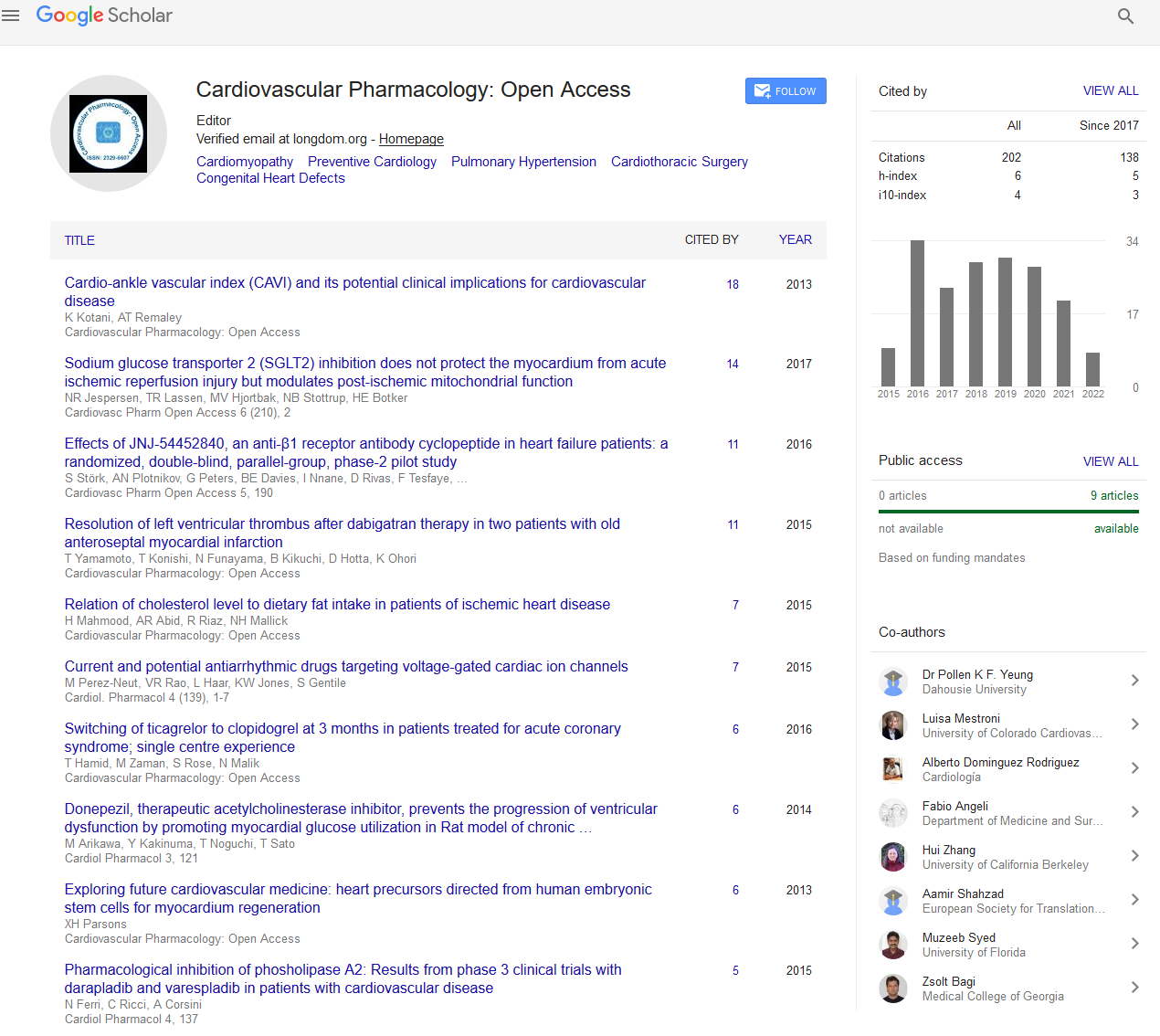
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Commentary - (2022) Volume 11, Issue 6
Strategies in the Management of Acute Type A Aortic Dissection
Guan Bin Jiang*Received: 03-Jun-2022, Manuscript No. CPO-22-17183; Editor assigned: 06-Jun-2022, Pre QC No. CPO-22-17183 (PQ); Reviewed: 20-Jun-2022, QC No. CPO-22-17183; Revised: 27-Jun-2022, Manuscript No. CPO-22-17183 (R); Published: 04-Jul-2022, DOI: 10.35248/2329-6607.22.11.288
Description
Aortic dissection of type A is a fatal condition with a reported frequency of 2.5 to 6 per 100000 patient years. Shekelton is credited with the first known aortic dissection and the notion of true and false lumen in the early 1800s. A patient with an acute type A aortic dissection has a 50 percent to 70% chance of dying within 48 hours if left untreated. As a result, it's critical to go to work right away. False lumen rupture, acute cardiac tamponed, acute high-grade aortic valve insufficiency, and malperfusion syndromes are the most common causes of death in untreated individuals. Despite surgery, the 30-day death rate is still about 20% to 25%, according to the international registry of aortic dissection. The IRAD (International Registry of Aortic Dissection) is a worldwide registry that began recruiting patients in 1996. This initiative has produced up-to-date information on the short- and long-term consequences of acute aortic dissection, as well as potential treatment alternatives [1].
Aortic dissection is described as a rip in the innermost layer of the aortic wall (intima) that causes high-pressure blood flow between the layers of the aorta, resulting in a true and false lumen. Regardless of where the original intimal rip occurs, Type A aortic dissection affects the ascending aorta. Aortic dissection of type A is a surgical emergency, Patients who are affected are at a significant risk of developing life-threatening consequences (eg, cardiac tamponade from hemopericardium, aortic regurgitation, stroke, aortic rupture, myocardial infarction). Without surgery, death rates as high as 1% to 2% per hour following symptom start is possible. The first care of acute type A aortic dissection is discussed, as well as the pros and drawbacks of surgery, as well as the associated morbidity and mortality. The suggestions made are in general in accordance with interdisciplinary cardiovascular guidelines. Type A aortic dissection surgical methods are discussed individually.
Controlling pain and blood pressure in these individuals at the initial assessment is critical to preventing aortic rupture. Morphine and intravenous B-blockers (Labetalol, Esmolol) are used to achieve this. The desired systolic blood pressure and heart rate are fewer than 120 mmHg and 60 beats per minute, respectively. Intravenous B-blockers are beneficial in lowering the force of left ventricular ejection (dP/dt), which would otherwise damage the aortic wall. In some individuals with severe hypertension, a combination of intravenous B-blockers and sodium nitroprusside may be necessary. Intubation and ventilation may be required for patients with substantial hemodynamic instability [2].
Acute management
A "classic" history of acute, stabbing chest and/or back pain, echocardiographic evidence of intimal flap in the ascending aorta, new murmur, symptoms of malperfusion (eg, stroke), or hemodynamic instability are all clinical characteristics of type A aortic dissection. The clinical aspects of acute aortic dissection are discussed individually, as is the differential between type A and type B aortic dissection. If the patient has an acute type A aortic dissection, rapid cardiac surgical consultation is essential, and if expert cardiac surgical services are not available, the patient should be moved for final treatment as soon as possible [3].
Long term management
Long-term consequences are a possibility for patients who survive an acute type A aortic dissection. The three main management principles are continuous anti-impulse therapy in the form of blood pressure lowering to reduce aortic wall shear stress, evaluation for high-risk clinical conditions, and serial imaging to detect signs of dissection progression, re-dissection, or aneurysm formation with reoperation, if necessary [4].
On-going medical treatment
Intravenous beta blocker medication (or other antihypertensive therapy) can be shifted to an oral route after aortic repair if heart rate control is established and the patient tolerates an oral diet. All patients should be treated for the rest of their lives to lower their systemic blood pressure and the pace at which their systolic pressure rises, both of which lessen aortic wall stress. The goal blood pressure is less than 120/80 mmHg, notwithstanding the lack of evidence from controlled trials. Antihypertensive medication treatment in combination is frequently necessary.
Prior to discharge, we usually do a baseline Magnetic Resonance (MR) or Computed Tomographic (CT) angiography. Patients are then subjected to yearly aortic imaging surveillance for the rest of their lives. Because most patients have residual dissection in the distal aorta, it's critical to keep track of them. Residual patent false lumen, greater aortic diameters, many and wide fenestrations, and absence of arch replacement during the first type A dissection repair are all risk factors for aortic expansion of distal segments as well as reoperation after type A repair. Despite the best medical care, at least one-third of patients may need surgery for aortic-related problems within five years of the original dissection, with the risk being greatest in the first few months. Serial imaging is indicated at 1, 3, 6, and 12 months following discharge, as well as annually thereafter, to enable for early detection and surgical correction of late complications of type B dissection, the most prevalent of which is aneurysmal degeneration of a patent false lumen [5].
REFERENCES
- Hagan PG, Nienaber CA, Isselbacher EM, Bruckman D, Karavite DJ, Russman PL, et al. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. Jama. 2000;283(7):897-903.
- Mehta RH, O’Gara PT, Bossone E, Nienaber CA, Myrmel T, Cooper JV, et al. Acute type A aortic dissection in the elderly: clinical characteristics, management, and outcomes in the current era. J Am Coll Cardiol. 2002;40(4):685-92.
- Chiappini B, Schepens M, Tan E, Amore AD, Morshuis W, Dossche K, et al. Early and late outcomes of acute type A aortic dissection: analysis of risk factors in 487 consecutive patients. Eur Heart J. 2005; 26:180.
- Fattouch K, Sampognaro R, Navarra E, Caruso M, Pisano C, Coppola G, et al. Long-term results after repair of type a acute aortic dissection according to false lumen patency. Ann Thorac Surg 2009;88:1244-50.
- Sun L, Qi R, Zhu J, Liu Y, Zheng J. Total arch replacement combined with stented elephant trunk implantation: a new “standard” therapy for type a dissection involving repair of the aortic arch? Circulation. 2011;123:971-978.
Citation: Jiang GB (2022) Strategies in the Management of Acute Type A Aortic Dissection. Cardiovasc Pharm. 11:288.
Copyright: © 2022 Jiang GB. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.