Indexed In
- Genamics JournalSeek
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2020) Volume 9, Issue 2
Short Term and Long term Outcome of Single-Stage Trans-anal Pull Through for Hirschsprung’s Disease in Neonates and Infants
Sajad Ahmad Wani*, Gowhar Nazir Mufti, Kumar Abdul Rashid, Nisar Ahmad Bhat and Aejaz Ahsan BabaReceived: 09-Nov-2019 Published: 03-Aug-2020, DOI: 10.35248/2167-0897.20.9.277
Abstract
Purpose: Hirschsprungs disease is common cause of intestinal obstruction in neonate and trans-anal pull through has drastically changed the treatment of Hirschsprungs disease. The aim of this study was to evaluate the short and long-term outcome of single-stage trans-anal pull through in neonates and infants.
Material and methods: It was a prospective study of new-born’s and young infants with features of Hirschsprungs disease. Patients with weight more than 3 kg, transition zone at recto sigmoid and distal sigmoid region were included in the study. Patients with more dilated proximal colon, bowel obstruction not responding to washes and long segment Hirschsprungs disease were excluded from the study. Single-stage trans-anal pull through was done in all cases and short term variables include wound infection, leak, peri-anal excoriation and long term outcome variables included continence, constipation, stricture, enterocolitis and need of redo pull-through procedure were evaluated.
Results: 24 patients were included in the study. There were 15 males and 9 females. Age of the patients ranged from 26 days to 4.5 months with mean age of 1.3 months. Weight of the patients ranged from 3 kg to 5.3 kg with mean weight of 4.8 kg. Wound infection and perianal excoriation was seen in 8.3% and 45.8% respectively. Enterocolitis, stricture, constipation and minor soiling were seen in 12.5%, 4.2%, 8.3% and 12.5% respectively. Follow-up period ranged from 10 to 120 months.
Conclusion: Trans-anal pull through is feasible and safe option with excellent results in neonates and infants with short segment Hirschsprungs disease.
Keywords
Hirschsprungs disease; New-born’s and young infants; Transanal Endorectal Pull-Through (TEPT); Outcome
Introduction
Hirschsprungs disease is relatively common surgical disease in neonates and children with an incidence of 1 in 5000 live births, characterized by absence of ganglion cells in the sub mucosal and myenteric plexuses of the distal bowel [1,2]. This aganglionosis leads to functional obstruction presenting with delayed passage of meconium in the neonatal period, chronic constipation with abdominal distension and failure to thrive in older children. Unusually, it may presents with perforation peritonitis with sepsis. Barium enema is usually diagnostic but transition zone may not be obvious in the first three months of life [2,3]. Absence of ganglion cells and presence of hypertrophied nerve fibres on rectal biopsy confirms the diagnosis.
Traditionally Hirschsprungs disease has been managed by staged procedure, which consisted of a proximal defunctioning colostomy with multiple colonic biopsies, a definitive pull-through procedure and finally colostomy closure [4]. Over the past few decades, many paediatric surgeons abandoned the use of colostomy and favour single-stage pull-through procedure [5-7]. Over the years, increasing numbers of authors described a single-stage trans-anal pull-through in suitable cases and obviates the need for multiple surgeries, no pelvic structure damage, no scars, associated with less postoperative pain, shorter hospital stay and there is a high degree of parental acceptance of the procedure as it avoids the need to care for a baby with a colostomy. The most commonly used technique for the trans-anal pull-through is endorectal dissection which leaves a muscular cuff, which is usually split posteriorly [8,9]. Return of bowel function is earlier in the postoperative period and permits early initiation of oral feeds.
The aim of this study was to evaluate the short term and long- term outcome of single-stage trans-anal pull-through procedure for the management of Hirschsprungs disease in neonates and infants.
Material and Methods
This study was conducted over a period of 8 years from January 2009 to February 2017 in the Department of Paediatric and Neonatal Surgery Sher-I-Kashmir Institute of Medical Sciences, which is the only tertiary care and high volume centre in the state. It was a prospective study. Newbern’s and young infants with features of Hirschsprungs disease were included in the study. The inclusion criteria’s were weight more than 3 kg, transition zone at recto sigmoid and distal sigmoid region, absence of enterocolitis and sepsis. Patients with more dilated proximal colon, bowel obstruction not responding to washes and long segment Hirschsprungs disease were excluded from the study. The diagnosis was based on the history of delayed passage of meconium, abdominal distension and vomiting. Barium enema was done in all cases and transition zone was taken as an indicator of the level of aganglionosis. Initially patients were decompressed with rectal washes. Preoperative bowel preparation was given in most of the cases. Parents were explained in detail about the procedure and confirmation of ganglionic and aganglionic segment with intraoperative frozen section. Written informed consent was taken from the parents. Single-stage trans-anal pull through procedure was done in all patients. Intraoperative frozen section was done in all cases to confirm the level of aganglionosis (transition zone) and normal ganglionic segment above the transition zone.
Outcome variables were short term and long term. Short term variables include wound infection, leak, peri-anal excoriation and time of initiation of oral feeds. Long term outcome variables included continence, constipation, stricture; enterocolitis and need of redo pull-through procedure.
In our patients, we used the descriptive Krickenbeck score (Table 1) to grade the fecal incontinence (soiling) and constipation. Constipation and soiling were given a score 0 (normal) to 3.
| Parameters | Grade | ||
|---|---|---|---|
| Soiling /Fecal incontinence | Grade-1 | Grade-2 | Grade-3 |
| Occasionally (once or twice per week) | Every day | Constant | |
| Constipation | Manageable with diet | Requires laxatives | Resistant to diet and laxatives |
Table 1: Krickenbeck score for postoperative results.
Surgical Technique
After induction of general anaesthesia with caudal block supplementation, Foleys was introduced. Lithotomy position was given and gentle anal dilatation was done. Everting sutures using 3/0 silk were placed to expose the anal mucosa, picking up skin 2 inches from the anus and the anal canal just distal to the dentate line (Figure 1). Dissection begins circumferential just 0.5 cm above the dentate line and dissected mucosa is held by stay sutures (Figure 2). Proximal circumferential dissection of the sub mucosa from underlying muscularis was done for about 2cm and then converted to full thickness of the rectal wall. The rectum and sigmoid colon was then mobilized out of the anus by working on the surface using electro cautery and leaving a muscular cuff of 1-2 cm (Figure 3).
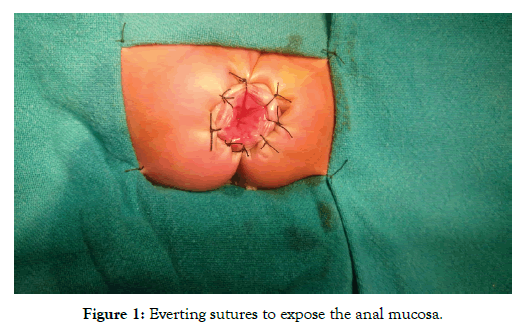
Figure 1: Everting sutures to expose the anal mucosa.
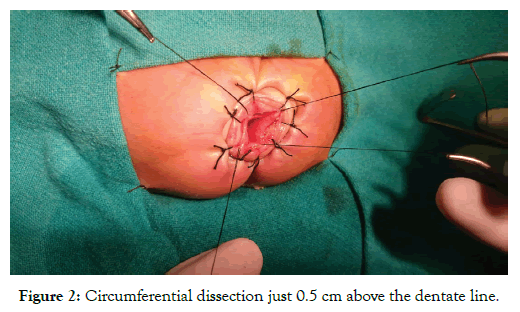
Figure 2: Circumferential dissection just 0.5 cm above the dentate line.
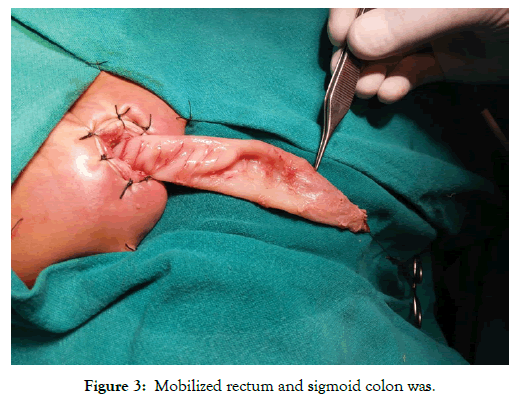
Figure 3: Mobilized rectum and sigmoid colon was.
Figure 4 is showing peristaltic wave stopping at the transition zone. Dissection was done up to the clear visualization of transition zone and proximal dilated bowel. Frozen section was taken 3-4 cm from transition zone and after confirmation of presence of ganglion cells, aganglionic segment was resected and colo-anal anastomosis was completed (Figure 5). Paraffin soaked gauge was kept in as anal pack and everting sutures were removed. Postoperatively patient was kept nil per orally for 2-3 days depending upon the recovery of bowel function and feeding was started slowly. Urinary catheter was removed on third postoperative day. Gentle rectal examination was done 2 weeks after the surgery and patient was put on anal dilatations once a day for 3 weeks then twice a week for 3 weeks and then once a week for 4 weeks. Initially patient were followed twice weekly for 2 months then once a monthly for 3 months and then 3-4 monthly thereafter.
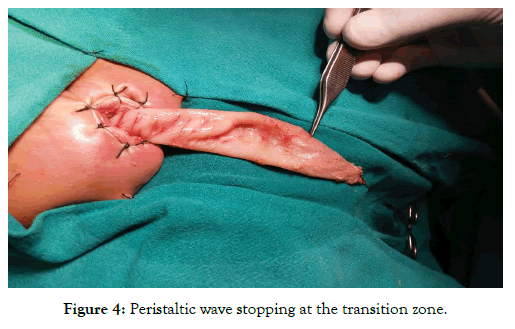
Figure 4: Peristaltic wave stopping at the transition zone.

Figure 5: Colo-anal anastomosis completed.
Results
Single-stage trans-anal pull through was done in 24 cases over a period of 8 years. There were 15 males and 9 females. Age of the patients ranged from 26 days to 4.5 months with mean age of 1.3 months. Weight of the patients ranged from 3 kg to 5.3 kg with mean weight of 4.8 kg. Most common clinical presentation in our patients was delayed passage of meconium (87.5%) followed by abdominal distension (70.8%) (Table 2). Site of the transition zone is shown in Table 3. Operative time ranged from 56 minutes to 125 minutes with mean of 85 minutes. None of the patients required blood transfusion.
| Clinical features | Â Frequency (No.) | Percentage (%) |
|---|---|---|
| Delayed passage of meconium | 21 | 87.5 |
| Abdominal distension | 17 | 70.8 |
| Vomiting | 8 | 33.3 |
Table 2: Clinical presentation.
| Site | Â Frequency (No.) | Percentage (%) |
|---|---|---|
| Recto sigmoid | 15 | 62.5 |
| Mid/Distal sigmoid | 6 | 25 |
| Rectum | 3 | 12.5 |
| Total | 24 | 100 |
Table 3: Site of transitional zone.
Short term outcome and long term outcome are shown in Table 4 and Table 5 respectively. Follow-up period ranged from 10 months to 120 months.
| Variables | Â Frequency (No.) | Percentage (%) |
|---|---|---|
| Perianal excoriation | 11 | 45.8 |
| Wound infection | 2 | 8.3 |
| Leak | 0 | - |
| Average time to full feeds (hours) | 24-48 | - |
| Duration of hospital stay (days) | 7-Mar | - |
Table 4: Short term outcome.
| Outcome variable/Complication | Â Frequency (No.) | Percentage (%) |
|---|---|---|
| Enterocolitis | 3 | 12.5 |
| Constipation | 2 | 8.3 |
| Stricture | 1 | 4.2 |
| Minor soiling | 3 | 12.5 |
Table 5: Long term outcomes.
Discussion
Hirschsprungs disease is one of the common surgical diseases in the paediatric age group. It is a congenital condition characterized by arrest in descend/degeneration of ganglion cells resulting in the absence of ganglion cells in the sub mucosal (Meissner’s) and myenteric (Auerbach’s) plexuses of the distal bowel. Majority of the patients have the classical disease with short aganglionic segment extending up to the recto sigmoid region. Unusually aganglionosis extend up to the whole of the colon and rarely the small bowel. Most of the patients with Hirschsprungs disease present with delayed passage of meconium in the newnorn period or chronic constipation with failure to thrive in older children. 95% of term neonates pass meconium within 24 hours of birth and only 10% of patients with Hirschsprungs disease pass meconium within 24 hours of birth [10]. In our study, 87.5% patients have delayed passage of meconium.
Radiographic transition zone correlates accurately with pathological transition zone in 90% of cases of Hirschsprungs disease [11]. Almond et al. has reported correlation of radiographic transition zone with the pathological transition zone in 28 (84.8%) patients. In our patients, radiographic transition zone has accurately correlated with the pathological transition zone in 22 (91.7%) patients. In 2 (8.3%) patients there was not clear cut transition zone on contrast enema. The loss of transition zone in these 2 patients could be due to the use of rectal washes. In most of our patients, rectal biopsy was not done because preoperative rectal biopsy makes the dissection difficult due to fibrosis and scarring and can affect the functional outcome [12]. However in 2 patients in which radiographic transition zone was not clear, rectal biopsy was sent for frozen section for confirmation of the diagnosis before the surgical procedure and transition zone was assessed by visual and palpatory examination of the mobilized bowel and confirmed by frozen section. In our patients, combination of history, contrast enema findings and intra-operative frozen section biopsy was 100% accurate for the diagnosis.
Trans-anal pull through procedure leaves a long aganglionic rectal muscular sleeve that can cause postoperative obstructive symptoms, constipation, enterocolitis and cuff stricture [13,14]. To avoid these problems of seromuscular cuff, many authors have recommended shorter mucosectomy and leaving short aganglionic seromuscular cuff measuring only 1-2cm above the dentate line [15,16]. We used the similar technique in our patients.
Perianal excoriation is a troublesome problem associated with trans-anal endorectal pull-through which probably occurs due to overstretching of the anal sphincters and subsequent increased stool frequency. In our series, 45.8% of patients had perianal excoriation, which lasted for a period varying from 2 weeks to 5 months. Hadidi reported increased stool frequency in all cases lasting up to 6 weeks [17]. Rintala reported perianal skin rash in 14 out of 26 (54%) patients [8]. Rakesh and Harjai reported perianal excoriation in 11 out of 14 (78.5%) patients lasting from 3 weeks to 6 months [18,19].
In our study, none of the patients had anastomotic leak, which may be related to good vascularity, good surgical technique and preoperative bowel preparation. [20-23] have reported 0% anastomotic leak.
Enterocolitis has been considered one of the main complications in patients with Hirschsprung’s disease and can occur both before and after definite treatment. In our patients, postoperative enterocolitis has occurred in 3 (12.5%) of patients, which were treated by nil per orally, intravenous fluids, intravenous antibiotics and rectal washes. Pradeep et al. [24], Ali [25], Hassan [26], Weidner et al. [21], Mahjan et al. [9] and Khalaf [19], Rakesh and Harjai [18] have reported postoperative enterocolitis in 20%, 14.3%,11.9%, 13%, 11.7%, 9.09%, 7.1% respectively.
Almost all studies have reported coloanal anastomosis stricture in patients who underwent trana-anal pull through procedure. This may be the result of ischemia of the mobilized colon, anastomotic leak, technical complication, narrow muscular cuff, wound infection and failure to adhere to dilation program. In our study, coloanal anastomotic stricture occurred in 1 (4.2%) patient, which was managed by dilatations. Swande et al. [27], Khalaf [19], Mahjan et al. [9], Gao et al. [20], Ali [25], Hassan [26] have reported stricture formation in 3.03%, 3.03%, 11.7%, 3.03%, 7.1% and 4.8% respectively.
There is no international consensus on any scoring system to describe bowel function after HD surgery. Furthermore, different authors use various definitions of constipation, soiling and fecal incontinence. In our patients, we used Krickenbeck score (Table 1), which was defined for anorectal malformations. Since HD patients suffer from many of the same problems as patients with anorectal malformations, and Krickenbeck score is the most novel system developed by international consensus for functional results after anorectal surgery in children. Hence, we too apply this score to describe postoperative results in our patients.
Constipation is common complaint following surgery, which may result from incomplete resection, stricture formation, fecaloma, sphincter achalasia, neuropathic ganglionic bowel, acquired Aganglionosis or may be functional. The reported incidence of constipation after trans-anal pull through is ranging from 0% to 8.6% [17,28-30]. In our study, 2(8.3%) patient had constipation problem, which was managed with laxatives.
Fecal soiling has the greatest negative impact on the quality of life in children with Hirschsprung’s disease. Soiling is physically, emotionally and psychologically disabling. Soiling after pull through can be due to the abnormal sphincter function, abnormal sensation or pseudo-incontinence related to abnormal rectal function or obstipation. Different authors have reported incontinence ranging from 0% to 17% [12,17,28-31]. In our patients, complete continence was achieved 14 (87.5%) patients. 3 (12.5%) patients had minor soiling (grade-1) which improved over time. A comparison of various studies of single-stage trans-anal pull through is shown in Table 6.
| Study | No. of patients | Frozen section | Leak % | Enterocolitis % | Peri-anal excoriation% | Stricture% | Soiling% |
|---|---|---|---|---|---|---|---|
| Weider et al. [21] | 15 | Yes | None | 13 | NA | NA | NA |
| Mahajan et al. [9] | 17 | Yes | None | 11.7 | NA | 11.7 | NA |
| Khalaf [19] | 33 | No | None | 9.09 | 6.1 | 3.03 | 9.09 |
| Handa and Harjai [18] | 14 | No | NA | 7,1 | 78.5 | NA | 21.4 |
| Aslan et al. [28] | 22 | Yes | 4.5 | 9 | NA | NA | None |
| Elhalaby et al. [30] | 149 | Yes | 0.7 | 17.4 | 20.1 | 4.7 | 4.7 |
| Hadidi [17] | 68 | Yes | 2.9 | 4.4 | NA | NA | None |
| Present study | 24 | Yes | None | 12.5 | 45.8 | 4.2 | 12.5 |
Table 6: Comparison of various studies.
Conclusion
Single-stage trans-anal pull through is easily learned and is associated with excellent clinical results. It is safe and effective in neonates and young infants with Hirschsprungs disease provided we follow proper selection criteria. It avoids multiple abdominal operations, injury to the surrounding structures, no scars, less pain, shorter hospital stay and early initiation of oral feeds and high degree of parental acceptance.
Conflict of Interest
The authors declare that they have no conflict of interest. This article does not contain any studies with animals performed by any of the authors.
Funding
No source of funding.
REFERENCES
- Badner JA, Sieber WK, Garver KL, Chakravarti, AR. A genetic study of Hirschsprung disease. American Journal of Human Genetics. 1990;46:568.
- Madonna MB, Luck SR, Reynolds M, Schwarz DK, Arensman RM. Swenson procedure for the treatment of Hirschsprung's disease. In: Seminars in Pediatric Surgery. 1998;7:85-88.
- Lanfranchi GA, Bazzocchi G, Federici S, Brignola C, Campieri M, Rossi F, et al. Anorectal manometry in the diagnosis of Hirschsprung's disease--comparison with clinical and radiological criteria. American Journal of Gastroenterology. 1984;79:270-75.
- Harjai MM. Hirschsprung’s disease: Revisited. J Postgrad Med. 2000;46:52-54.
- Langer JC, Fitzgerald PG, Winthrop AL, Srinathan SK, Foglia RP, Skinner MA, et al. One-stage versus two-stage Soave pull-through for Hirschsprung's disease in the first year of life. J Pediatr Surg. 1996;31:33-37.
- Pierro A, Fasoli L, Kiely EM, Drake D, Spiz L. Staged pull-through for rectosigmoid Hirschsprung's disease is not safer than primary pull-through. J Pediatr Surg. 1997;32:505-509.
- Langer JC, Durrant AC, De La Torre L, Teitelbaum DH, Minkes RK, Caty MG, et al. One-stage transanal Soave pull through for Hirschsprung disease: A multicenter experience with 141 children. Annals of Surgery. 2003;238:569.
- Rintala RJ. Transanal coloanal pull-through with a short muscular cuff for classic Hirschsprung's disease. European J Pediatr Surg. 2003;13:181-186.
- Mahajan JK, Rathod KK, Bawa M, Narasimhan KL. Transanal Swenson's operation for Recto-sigmoid Hirschsprung's disease. African Journal of Paediatric Surgery. 2011;8:301.
- Dasgupta R, Langer JC. Transanal pull-through for Hirschsprung disease. In: Seminars in Pediatric Surgery. 2005;14:64-71.
- Proctor ML, Traubici J, Langer JC, Gibbs DL, Ein SH, Daneman A, et al. Correlation between radiographic transition zone and level of aganglionosis in Hirschsprung's disease: Implications for surgical approach. J Pediatr Surg. 2003;38:775-778.
- Pratap A, Shakya VC, Biswas BK, Sinha A, Tiwari A, Agrawal CS, et al. Single-stage transanal endorectal pull-through for Hirschsprung's disease: perspective from a developing country. J Pediatr Surg. 2007;42:532-535.
- Tariq GM, Brereton RJ, Wright VM. Complications of endorectal pull through for Hirschsprung’s disease. J Pediatr Surg. l991;26:1202-1206.
- Joseph VT, Sim CK. Problems and pitfalls in the management of Hirschsprung’s disease. J Pediatr Surg. 1988;23:398-02.
- Ahmed N, Langer JC. Evolution of technique in the transanal pullthrough for Hirschsprung’s disease: Effect on outcome. J Pediatr Surg. 2007;42:36-40.
- Wester T, Rintala RJ. Early outcome of transanal endorectal pullthrough with a short muscle cuff during the neonatal period. J Pediatr Surg. 2004;39:157-60.
- Hadidi A. Transanal endorectal pull-through for Hirschsprung’s disease: a comparison with the open technique. Eur J Pediatr Surg. 2003;13:176-80.
- Handa R, Harjai MM. Single Stage Transanal Endorectal Pull-Through for Management of Hirschprung’s Disease. Journal of paediatric surgical specialities. 2015;9:1–52.
- Khalaf AA. Transanal Endorectal Swenson Pullthrough: A single center experience. 2014;13:356-63.
- Gao Y, Li G, Zhang X, Xu Q, Guo Z, Zheng B, et al. Primary transanal rectosigmoidectomy for Hirschsprung's disease: Preliminary results in the initial 33 cases. J Pediatr Surg. 2001;36:1816-1819.
- Weidner BC, Waldhausen JH. Swenson revisited: a one-stage, transanal pull-through procedure for Hirschsprung’s disease. J Pediatr Surg. 2003; 38:1208-1211.
- Xu ZL, Zheng Z, Long W, Qun AN, Tao WF. A new modification of transanal Swenson pull-through procedure for Hirschsprung's disease. Chinese Medical Journal. 2008;121:2420-2423.
- Sookpotarom P, Vejchapipat P. Primary transanal Swenson pull-through operation for Hirschsprung’s disease. Pediatric Surgery International. 2009;25:767-773.
- Bhatiav P, Joshi SR., Ramji J, Bachani M, Uttarwar A. Single Stage Transanal Pull-Through for Hirschsprung’s Disease in Neonates: Our Early Experience. Journal of Neonatal Surgery. 2013;2:39.
- Ali KAE. Transanal endorectal pull-through for Hirschsprung’s disease during the first month of life. Ann Pediatr Surg. 2010;6:81-88.
- Hassan HS. One stage tranasnal endorectal pull through procedure for Hirschsprung’s disease in neonates. Ann Pediatr Surg. 2009;5:21-26.
- Sowande and Adejuyigbe: Swenson’s Pull-through in Nigerian Children. Ten-year experience with the Swenson procedure in Nigerian children with Hirschsprung’s disease. African Journal of Paediatric Surgery. 2011;8.
- Aslan MK, Karaman I, Karaman A, Erdogan D, Cavusoglu YH, Çakmak Ö. Our experience with transanal endorectal pull-through in Hirschsprung's disease. European J Pediatr Surg. 2007;17:335-339.
- Zhang SC, Bai YZ, Wang W, Wang WL. Clinical outcome in children after transanal 1-stage endorectal pull-through operation for Hirschsprung disease. J Pediatr Surg. 2005;40:1307-1311.
- Elhalaby EA, Hashish A, Elbarbary M, Soliman HA, Wishahy MK, Elkholy A, et al. Transanal one-stage endorectal pull-through for Hirschsprung’s disease: a multicenter study. J Pediatr Surg. 2004;39:345-351.
- Hakgüder G, Kart Y, Olguner M, Akgür FM. The effect of dilated ganglionic segment on anorectal and urinary functions during 1-stage transanal endorectal pull through for Hirschsprung's disease. J Pediatr Surg. 2007;42:1271-1275.
Citation: Ahmad Wani S, Nazir Mufti G, Abdul Rashid K, Ahmad Bhat N, Ahsan Baba A (2020) Short Term and Long term Outcome of Single-Stage Trans-anal Pull Through for Hirschsprung’s Disease in Neonates and Infants. J Neonatal Biol 9:277. doi: 10.35248/2167-0897.20.9.277
Copyright: © 2020 Wani SA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

