Indexed In
- Open J Gate
- Academic Keys
- ResearchBible
- China National Knowledge Infrastructure (CNKI)
- Centre for Agriculture and Biosciences International (CABI)
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- CABI full text
- Publons
- Geneva Foundation for Medical Education and Research
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research - (2020) Volume 8, Issue 4
Sero Burden of Toxoplasma gondii and Associated Risk Factors among HIV Infected Persons in Armed Forces Referral and Teaching Hospital, Addis Ababa, Ethiopia
Fewzia Mohammed1,2*, Mulusew Alemneh Sinishaw3,4, Negash Nurahmed1, Shemsu Kedir Juhar1 and Kassu Desta52Armed forces Referral and Teaching Hospital, Addis Ababa, Ethiopia
3Clinical Chemistry Department, College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia
4Clinical Chemistry Department, Amhara Public Health Institute, Bahir Dar, Ethiopia
5Department of Medical Laboratory Sciences, School of Allied Health Science, College of Health Sciences, Addis Ababa, Ethiopia
Received: 09-Sep-2019 Published: 24-Jul-2020, DOI: 10.35248/2329-891X.20.8.341
Abstract
Background: Toxoplasmosis is a zoonotic disease, worldwide distribution caused by an obligate intracellular coccidian parasite, known as Toxoplasma gondii. T. gondii can lead to serious diseases in immuno-compromised patients such as HIV/AIDS patients. In most cases, central nervous system involvement can lead to encephalitis, which is one of the most important reasons for death among patients with HIV due to reactivation of tissue cysts that remained latent after the primary infection. This study was conducted to assess the sero burden of Toxoplasma gondii infection and identify associated risk factors among HIV infected individuals in Armed Forces Referral and Teaching Hospital, Addis Ababa, Ethiopia.
Methods: A cross-sectional study was conducted from March to May 2016. After getting an informed consent a pretested questionnaire was used to gather socio-demographic information and data on factors predisposing to T. gondii infection using convenience sampling methods. Serum samples from each volunteered patients were screened for the presence of anti-T. gondii IgG and IgM antibodies by using ELISA test kit (CTKBIOTECH, USA). Data were entered and analyzed using SPSS version 15.0. The chi-square test was used to observe any difference between variables. p-values were determined and taken as a level of significance when they found less than 0.05.
Results: The study recruited a total of 174 HIV infected patients, of whom 99 (56.9%) were males. The study also included different age strata ranging from 18-68 years. Most of the sampled subjects were found in the age group of 31-40 years old. About 154 (88.5%), were seropositive for anti-T. gondii IgG antibody and 3 (1.7%) seropositivity for anti-T. gondii IgM antibodies. None were positive for IgM antibody alone. Of all the variables included in the study, only the presence of the cat depicted an association with sero-burden of anti-Toxoplasma gondii IgG antibody (p=0.038).
Conclusion: This study revealed a high sero burden of chronic toxoplasmosis in HIV/AIDS patients. HIV/AIDS patients having a domestic cat at their home were at higher risk of T. gondii infection. It would be important to increase public awareness about different routes of transmission of T. gondii. Besides, routine screening for Toxoplasma should be undertaken for all HIV-infected patients to minimize complications related to reactivation.
Keywords
HIV/AIDS; Toxoplasma gondii; IgG; IgM
Introduction
Toxoplasma gondii, a member of the phylum Apicomplexa, is an obligate intracellular parasite [1,2]. The life cycle consists of two stages (asexual and sexual); the asexual stage takes place in the intermediate hosts, which are mammals or birds [1]. The sexual stage takes place in the intestine of the definitive host; known definitive hosts are members of the feline family, predominantly domestic cats [3].
The three typical infections transmission routes of peoples are foodborne, animal-to-human and mother-to-child (congenital) [3,4]. Immunocompetent women infected prior to conception virtually never transmit toxoplasmosis to the fetus, although rare exceptions have been reported [5]. There are also rare instances of transmission i.e. via tachyzoites contained in blood products, tissue transplants, or unpasteurized milk, and laboratory workers who handle infected blood can also acquire infection through accidental inoculation [6].
The infection of this parasite leads to an asymptomatic infection in immune-competent persons. However, 10% to 20% of patients with acute infection may develop cervical lymphadenopathy and/or a flu-like illness. The clinical course is benign and self-limited; symptoms usually resolve within a few months to a year [7]. Mortality/Morbidity studies show that immuno-compromised individuals and fetuses are at particularly high risk for severe sequelae and even death [8]. Immunodeficient patients often have central nervous system disease but may have chorioretinitis, or pneumonitis [9]. In patients with AIDS, toxoplasmic encephalitis is the most common cause of intracerebral mass lesions and is thought to be caused by reactivation of chronic infection [10].
When Toxoplasma infection is acquired by a mother during pregnancy, the parasite presents a significant risk of adverse outcomes to the fetus [11]. The risk of transmission from mother to fetus is lower when the maternal infection is acquired in the early stages of pregnancy but the outcome in such cases can be severe or life-threatening to the fetus. Conversely, while maternal infection acquired later in pregnancy confers a higher risk of transmission to the fetus, the clinical outcome is characteristically less severe, or the child may even be born asymptomatic [12]. Latent T. gondii infection may be reactivated in immune-deficient individuals (such as HIV-infected women) and result in the congenital transmission of the parasite [4].
Four clinical signs are thus considered as representative of congenital toxoplasmosis; hydrocephaly or microcephaly, retinochoroiditis, cerebral calcifications, and neurological injury. This clinical spectrum, which represents some of the late sequelae of infection, was later enlarged with a variety of acute signs, hydrops fetalis, erythroblastosis and jaundice with hepatosplenomegaly [13].
However Toxoplasmosis in HIV-infected patients occurs usually due to reactivation of chronic infection, and it usually presents as toxoplasmic encephalitis. In AIDS patients, T. gondii is the most common opportunistic infection that causes focal brain lesions. The initial presentation of toxoplasmic encephalitis in patients with AIDS may be sub-acute. Patients present with altered mental status (62%), headaches (59%), and fever (41%) associated with focal neurologic deficits. Progression of the infection can lead to confusion, drowsiness, seizures, hemiparesis, hemianopsia, aphasia, ataxia, and cranial nerve palsies. Motor weakness and speech disturbance are seen as the disease progresses. If not treated promptly, patients may progress to coma within days to weeks. The eyes and lungs are the most common sites of extracerebral manifestation of toxoplasmosis, and such manifestations may occur with or without concomitant encephalitis. Extra cerebral manifestations occur less frequently than cerebral toxoplasmosis [11].
It is generally assumed that approximately 25% to 30% of the world's human population is infected by Toxoplasma [14]. Actually, the prevalence varies widely between countries (from 10% to 80%) and often within a given country or between different communities in the same region [15]. Low seroprevalences (10% to 30%) have been observed in North America, in South East Asia, in Northern Europe, and in the Sahelian countries of Africa. Moderate prevalence (30% to 50%) has been found in countries of Central and Southern Europe, and high prevalence has been found Latin America and in tropical African countries.
Toxoplasmosis is a major public health concern because the disease is serious in terms of mortality or physical and/or psychological sequellae in patients with HIV disease [15]. In the majority of normal, healthy (immune-competent) subjects, infection is asymptomatic and frequently results in the chronic persistence of cysts within host tissues; the cysts normally lie dormant, probably for life. But, in immune-compromised states such as in HIV infections, subjects are at risk of developing acute toxoplasmosis due to reactivation of the organism if their CD4+ T-cell count decreases below 200 cells/μL [11,12]. Since the pandemic of HIV infection has spread throughout the world, toxoplasmosis has been implicated as one of the most important opportunistic infections in HIV/AIDS patients. Moreover, in up to 10% of HIV infected immune-competent individuals, it causes cervical lymph-adenopathy or ocular disease [16-18].
In developing countries, Toxoplasma-HIV co-infected patients have a risk as high as 30% to 40% of Toxoplasma encephalitis, especially those with significant immuno-suppressant (CD4 cell count<200 cells/μL) [2,4]. Thus, identification of latently infected immunocompromised patients by determining anti- Toxoplasma IgG (immunoglobulin G) antibodies becomes essential [19]. Studies in the USA showed that about 30% of AIDS patients previously exposed to toxoplasma and suffered from a cerebral reactivation [20]. Consequently, it may be calculated that 8% of AIDS patients in South East England will experience a life-threatening episode of cerebral disease following secondary reactivation of toxoplasmosis. In addition to this, 0.5%-1% of these patients may acquire primary toxoplasmosis associated with AIDS each year reflecting the incidence of toxoplasma infection in this group [21].
Among the congenital infections, approximately 10% of congenital toxoplasmosis results in abortion or neonatal death. It is estimated that 10%-13% of the babies will have a visual handicap. Clinical signs of congenital Toxoplasmosis are not apparent at first in most cases but infection acquired after birth is usually asymptomatic. Intrauterine meningoencephalitis could lead to the development of the following: Cerebrospinal Fluid (CSF) abnormalities, hydrocephalus, microcephaly, chorioretinitis, seizures, and deafness. Some of the severely affected infants die in utero or within a few days of birth. Other signs include maculopapular rash, generalized lymphadenopathy, hepatomegaly, splenomegaly, jaundice, and thrombocytopenia [22].
The majority of infections are asymptomatic and patients rarely experience symptoms or complications, which can make detection and control of T. gondii transmission challenges. This is further complicated by the fact that T. gondii leads to significant clinical consequences given their infectious nature, chronicity, and therapeutic difficulties. Hence, the serologic screening will allow early detection of T. gondii infection in asymptomatic carriers and the prevention of adverse sequelae in HIV/AIDS patients [23].
The risk factors associated with seropositivity to toxoplasmosis are raw or undercooked mutton consumption and the presence of cats. Individuals consuming raw or undercooked mutton were found 16.9 times more likely to be positive than those known to consume well-served mutton. Toxoplasmosis is a zoonosis arising from man's close contact with domestic cats (Felis catus). Individuals with a known history of association with cats were 5.3 times more likely to be seropositive than those with no history of such association [24]. Recent studies have identified water as a potential source of infection in both humans and animals [25].
Although toxoplasmosis is a problem throughout the world, its frequency varies from one geographic area to another. Screening for T. gondii is not routinely performed in Ethiopia due to limited health resources and a lack of awareness of the prevalence of the disease and its mode of transmission. Lack of awareness is likely to expose them to increased risk of contracting toxoplasmosis, as they might not take proper precautions. Moreover, data on Seroprevalence of T. gondii and the associated risk factor is limited in some regions of Ethiopia and published reports on magnitude of T. gondii infection in HIV-infected individuals is mainly done with rapid serological test kits which could not reflect the actual burden of Toxoplasmosis in the country. Moreover, our study site is totally different representing Military hospital and the study participants have different risks for Toxoplasmosis. To the best of our knowledge, there was no information concerning burden of T. gondii in Armed Forces Referral and Teaching Hospital. Therefore this study was designed to determine the burden of T. godii infection and associated risk factors among HIV/AIDS infected individuals and try to address the aforementioned gaps and further expand our knowledge of Toxoplasmosis in Ethiopia.
Materials and Methods
A hospital-based cross-sectional study was conducted from March to May 2016 in Armed forces referral and teaching hospital, Addis Ababa, Ethiopia. Armed Force Referral and Teaching Hospital (AFRTH) are located in Ledeta sub-city, Addis Ababa, Ethiopia. It is organized under Health Main Directorate, Ministry of Defense. It provides medical service to members of the Ethiopian defense force and their families. AFRTH has 15 wards with 600 beds. There are 378 health care professionals with different levels and fields of training. Based on the 2014/2015 annual report the hospital provides services for 96,621 outpatients and 3,334 inpatient, 1,223 deliveries as well as 21,200 ART patients. Other than patient diagnosis, AFRTH is also engaged in different activities like health teaching and research. All adult HIV positive patients (aged 18 and above years) who were sent to Armed Forces Referral and Teaching hospital ART clinic for CD-4 cell count and ART monitoring were studied.
The sample size was calculated based on a single population sample size estimation formula taken the prevalence of 87% from the previous study conducted by Bahir Dar [26] considering 95% confidence interval and 5% margin of error. The total calculated sample size was 174 study subjects. Consecutive sampling technique was employed to include study participants who meet the inclusion criteria.
Data collection and specimen transportation
Data were collected by trained medical laboratory technologist and a nurse under the supervision of the principal investigator. A pre-tested structured questionnaire was used to collect sociodemographic information and data on factors predisposing to T. gondii infection from patients through face to face interviews. HIV related Clinical data such as WHO HIV clinical stages, CD4 cell counts and Highly Active Antiretroviral Therapy (HAART) status, of study participants, were taken from patient history cards and documented. The patients were asked to give blood sample and if they were willing then the laboratory technologist collected 4 mL of venous blood sample using serum separated vacutainer tube and the sample was left for 30 minutes to facilitate clotting and then the clotted blood centrifuged to separate the serum from blood. Serum was secondly aliquoted into Nunc tubes and stored at -20°C until use. Repeated freezing and thawing were avoided. All regulation was strictly followed during specimen collection, packaging, and transportation.
Laboratory investigation
The serologic test was employed by using a commercially available ELISA test kit (CTK BIOTECH RecombiLISA Toxo IgM and IgG ELISA Kit USA) as per manufacturer’s instruction. Positive and negative controls were used with each series of anti- T. gondii IgG/IgM test (Human, USA); results were obtained by comparison with a cut-off value measured at 450 nm absorbance.
Interpretation of the ELISA result and quality assurance
We have interpreted the ELISA results according to the instruction provided by the manufacturer presented in the test kit insert. If the Optical Density (OD) ratio is greater or equal to 1.0, it is considered positive if it is below 1.0 it was taken as negative. The Negative result indicates that there is no detectable IgM/IgG anti-T. gondii in the specimen. The quality of test results was maintained using the internal quality control of the test kits for the ELISA method. All reagents that are used for testing checked for their shelf life, being at the appropriate temperature before using them. Test procedures were done according to the manufacturer’s instruction.
Data analysis and interpretation
Data was entered and analyzed using the statistical software SPSS version 16.0. The Seroburden for Toxoplasmosis was expressed in percentages for the entire study group and results obtained were presented in tables, figures, and graphs. The chisquare test was used to determine the association between variables. p-values were determined and taken as a level of significance when finding less than 0.05.
Ethical consideration
Ethical clearance was obtained from the Departmental Ethics and Research Committee of the Department of Medical Laboratory Science, College of Health Sciences and School of Allied Health Science of Addis Ababa University and official permission to collect data was obtained from the Armed Forces Referral and Teaching Hospital administrator. Subjects were recruited after they become informed about the objectives and use of the study and after they gave informed consent. Data and samples taken from each patient were coded and the results obtained were kept confidential.
Results
Socio-demographic status of study participants
Of all the study participants (174), 99 (56.9%) were male, 163 (93.7%) were urban dwellers, 64 (36.8%) were government employees and 64 (36.8%) were with educational level 9 to12. The study also included age strata ranging from 18 to 68 years. Most of the study subjects were found in the age group of 31to 40 years (41.4%) (Table 1).
| Variable with category | Frequency | Percent (%) |
|---|---|---|
| Sex | ||
| Male | 99 | 56.9 |
| Female | 75 | 43.1 |
| Age groups in years | ||
| 21-30 | 19 | 10.9 |
| 31-40 | 72 | 41.4 |
| 41-50 | 61 | 35.1 |
| >50 | 22 | 12.6 |
| Residence | ||
| Urban | 163 | 93.7 |
| Rural | 11 | 6.3 |
| Occupation | ||
| Government | 64 | 36.8 |
| Private | 62 | 35.6 |
| Housewife | 35 | 20.1 |
| Others | 13 | 7.5 |
| Level of education | ||
| Read and write | 12 | 9.2 |
| Primary (1-8) | 47 | 27 |
| Secondary (9-12) | 64 | 36.8 |
| Above grade 12 | 51 | 29.3 |
Table 1: Socio-demographic status of HIV/AIDS patients attending the Armed Forces Referral and Teaching Hospital; Addis Ababa, Ethiopia, March to May 2016.
Clinical and other contributing factors of study subjects
Among the total study participants (174), none had a history of organ transplantation. About 129 (74.1%) had a cat at home and 144 (82.8%) ate raw vegetables and fruit. Only 7 participants (4%) were not on HAART and 15.5% (27) participants had low CD4 T cell count below 200 cell/μl of blood (Table 2).
| Contributing factors | Category | Frequency | Percent (%) |
|---|---|---|---|
| Had cat | No | 45 | 25.9 |
| Yes | 129 | 74.1 | |
| Eat uncooked meat | No | 115 | 66.1 |
| Yes | 59 | 33.9 | |
| Eat raw vegetable and fruit | No | 30 | 17.2 |
| Yes | 144 | 82.8 | |
| Having a history of blood transfusion | No | 136 | 78.2 |
| Yes | 38 | 21.8 | |
| HAART status | with HAART | 167 | 96 |
| without HAART | 7 | 4 | |
| CD4 cell count | <200 | 27 | 15.5 |
| 200-500 | 86 | 49.4 | |
| >500 | 61 | 35.1 | |
| WHO stage | Stage I | 164 | 94.3 |
| Stage II-IV | 10 | 5.7 |
Table 2: Frequency of contributing factors for T. gondii infection among HIV patients attending the Armed Forces Referral and Teaching Hospital; Addis Ababa, Ethiopia, March to May 2016.
The burden of T. gondii infection
From all 174 blood samples that were collected from HIV/AIDS patients and tested for Toxoplasma antibodies, 154 (88.5%) were seropositive for anti-T. gondii IgG antibody and 3 (1.7%) were seropositive for anti-T. gondii IgM antibodies. None was positive for IgM antibody alone (Figure 1).
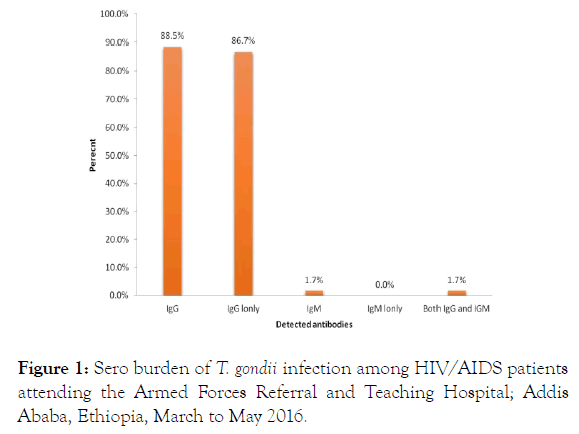
Figure 1. Sero burden of T. gondii infection among HIV/AIDS patients attending the Armed Forces Referral and Teaching Hospital; Addis Ababa, Ethiopia, March to May 2016.
Association of contributing factors with T. gondii infection
Of all the variables included in the study, only the presence of the cat at home was depicted association with sero-burden of anti-T. gondii IgG antibody (p=0.038) as presented on (Table 3) and there was no significant difference in Toxoplasma seropositivity to IgG in relation to HIV/AIDS-related clinical data of the study participant (Table 4).
| Contributing factors X2-test | Category | T. gondii | IgG value | p-Value | |
|---|---|---|---|---|---|
| Positive | Negative | ||||
| Sex | Female | 68 | 7 | ||
| Male | 86 | 13 | 0.605 | 0.437 | |
| Residence | Urban | 144 | 19 | ||
| Rural | 10 | 1 | 0.071 | 0.79 | |
| Educational status | Read and write | 11 | 0 | ||
| Elementary (1-8) | 42 | 5 | 2.057 | 0.725 | |
| Secondary (9-12) | 54 | 10 | |||
| >12 | 47 | 4 | |||
| Occupation | Government employee | 54 | 10 | ||
| Housewife | 32 | 3 | |||
| Private employee | 55 | 7 | 4.475 | 0.215 | |
| Others | 13 | 0 | |||
| Presence of cat | Yes | 118 | 11 | ||
| No | 36 | 9 | 4.317 | 0.038 | |
| Eat uncooked meat | Yes | 54 | 5 | ||
| No | 100 | 15 | 0.8 | 0.371 | |
| Eat raw vegetable and fruit | Yes | 126 | 18 | ||
| No | 28 | 2 | 0.935 | 0.334 | |
| Had a history of blood transfusion | Yes | 34 | 4 | ||
| No | 120 | 16 | 0.046 | 0.831 | |
Table 3: Association of socio-demographic and contributing factors for T. gondii infection among HIV infected individuals attending Armed Forces Referral and Teaching Hospital; Addis Ababa, Ethiopia, March to May 2016.
| Clinical variable | Category | T. gondii IgG | X2-test value |
p-value | |
|---|---|---|---|---|---|
| Positive | Negative | ||||
| HAART status | with HAART | 148 | 19 | ||
| without HAART | 6 | 1 | 0.053 | 0.819 | |
| CD4 cell count | <200 | 23 | 4 | ||
| 200-500 | 80 | 6 | 3.457 | 0.178 | |
| >500 | 51 | 10 | |||
| WHO stage | Stage I | 145 | 19 | ||
| Stage II-IV | 9 | 1 | 1.522 | 0.677 | |
Table 4: Toxoplasma seropositivity (IgG) in relation to clinical variables among HIV infected individuals attending in Armed Forces Referral and Teaching Hospital; Addis Ababa, Ethiopia, March to May 2016.
Discussion
The seroburden of Toxoplasma gondii obtained in this study, 88.5% for anti-T. gondii IgG antibody and 1.7% for anti-T. gondii IgM antibodies were almost concurrent with a cross-sectional study done in Bahir Dar, Northwest Ethiopia, which reported seroprevalence of 87.4% (90/103) of the HIV seropositive individuals [26], and in Arba Minch Hospital, south Ethiopia, in 2013 which reported 88.2% (150/170) seropositivity for anti- T. gondii IgG antibody out of the total that HIV seropositive study Participants [27].
Our finding is lower than the study conducted at St. Paul Hospital, Addis Ababa Ethiopia in 2009 which reported latent Toxoplasma infection prevalence of 93.3% (154/165) among HIV positive patients [28] and Black Lion Hospital, Addis Ababa Ethiopia were 94% (141/150) of the HIV/AIDS patients were seropositive for anti-Toxoplasma gondii IgG antibodies [29]. The possible reason for this difference could be the difference in the study period and the expanded use of HAART which is more practiced today than six years back. However, our finding was higher than studies conducted in Nazareth town, Ethiopia in 2008, which illustrated a 60% (39/65) seropositivity rate for toxoplasma IgG antibody [24]. In Nigeria in 2012 among HIVinfected patients attending hospitals in Makurdi metropolis demonstrated 10.8% (39/360) of the study subjects were seropositive out of the enrolled patients [30], Cameroon in 2010 revealed 52.6% (70/133) were positive [31], at the Port Moresby General Hospital, Papua New Guinea, exhibited 60% (108/181) among HIV-infected participants [32], India from 2011 to 2013 a cross-sectional observational study confirmed 21.3% (141/661) [19], Iran a cross-sectional survey between 2007 and 2008 exemplified 77.4% (48/62) HIV/AIDS serum samples were found positive [33]. In Malaysia in 2002 reported 41.2% (124/301) positive of HIV/AIDS patients [34], Yugoslavia detected in 44.1% (127/288) of AIDS patients [35], and Mexico in 1997 explained that the prevalence were 50.0% (46/92) among HIV/AIDS infected participants [36].
The variation could be due to mainly on time of the study conducted in addition to that of the difference on method of diagnosis used at Nazareth town which was modified direct agglutination test, geographical location and source population, methodology of study employed like the study done in India was observational type and sample size divergence [37].
Toxoplasma infection is short-lived and it is frequently suppressed, The IgM antibody response leads to undetectable levels in the setting of severe immunosuppression [20,35]. Correspondingly, this study revealed lower rates of IgM seropositivity compared to IgG seropositivity which is, 3/174 (1.7%), 154/174 (88.5%) respectively. Lower rate of IgM seropositivity compared to IgG seropositivity in HIV-positive patients has also been similarly reported by other studies from India [19,38,39], Mexico [36] and South Africa [40]. This indicated that the detection of IgM antibodies in HIV-infected individuals gives support to the view that the screening for this antibody in the routine diagnosis of toxoplasmosis in nonpregnant HIV-infected patients may be of limited value [20,35].
Our present study found the only presence of a cat at home depicted association with seroprevalence of anti-T. gondii IgG antibody (p=0.038) of all other variables listed. This was supported by studies conducted in Nazareth town, Ethiopia, in 2008 illustrated that owning of cat were found to have significant association with seroprevalence [24], at the Port Moresby General Hospital, Papua New Guinea, from 2003 to 2005 exhibited the exposure to cats was an independent risk factor but other socio-demographic and disease variables studied such as meat diet, educational levels, and length of HIV infection did not demonstrate any association [32]; Study from Malaysia and Addis Ababa proved that CD4+ T lymphocyte cells count were not statistically associated with Toxoplasmosis [28,34,41].
This finding was inconsistent to that of a study in BahirDar, Nazareth town, and Addis Ababa, Ethiopia reported consuming raw or undercooked mutton and vegetables were independent predictors of T. gondii seropositivity [24,26,28]; and age, gender, and HIV serostatus were found to be significantly associated with seroprevalence of latent toxoplasmosis [41]. This discrepancy could be different in the time of the study and sample size issue.
HIV-related clinical variables such as CD4 cell count, ART status and HIV clinical stage with Toxoplasma seropositivity association may be helpful especially in developing countries to classifying patients who may benefit from Toxoplasma screening or from prophylaxis against toxoplasmosis. In this study, all these HIV-related clinical variables, was not related to Toxoplasma seropositivity, signifying that in our district screening for toxoplasmosis may not be strong predictors for Toxoplasmosis. In agreement with our results, studies from Addis Ababa [29], Mexico [39], and Malaysia [41] have shown no correlation between Toxoplasma seropositivity and CD4 cell count and while another study in Nairobi, Kenya [42], reported no correlation between HIV clinical staging and Toxoplasma seropositivity. In contrast, in France [9] revealed that HIV patients with CD4 cell counts less than 200 cells/μl were more likely to be Toxoplasma seropositive than those with counts greater than 200 cells/μl. Probably the sample size among HIV patients with CD4 cell count below 200 could be low compared to other studies and we could not find a significant association.
Strengths and Limitations of the Study
Strength of the study
Using ELISA test kit for the analysis of T. gondii IgG and IgM antibodies rather than a rapid test kit
Limitation of the study
The study recruited a small sample size limited to Armed forces Referral and Teaching hospital due to lack of enough funds to conduct the study
Conclusion and Recommendation
The current study shows a high burden of latent T. gondii infection among the study participants at Armed Forces Referral and Teaching Hospital in Addis Ababa, Ethiopia, and illustrates the current risk of developing toxoplasmic encephalitis. Thus, it may be appropriate and beneficial to include T. gondii screening as part of routine testing for all HIV/AIDS infected individuals. Moreover, this study shows the presence of cats at home were identified as possible associated risk factors of T. gondii infection among HIV infected patients. Considering the relative high sero-burden of Toxoplasmosis as revealed by this study it would be important to increase public awareness about different routes of transmission of T. gondii. HIV positive individuals should limit themselves contact with cats. Cat owners particularly, HIV infected patients could take necessary preventive measures proper disposal of cat feces and keep hygiene to avoid Toxoplasma infection. Moreover, HIV/AIDS patients should be screened for anti-Toxoplasma antibodies in order to minimize complications related to reactivation and or new infection. Finally, Follow up studies are needed to elucidate the real effect of Toxoplasmosis in HIV/AIDS patients in the study sites and other similar settings.
Conflict of Interest
The authors declare that they have no conflict of interests.Authors’ Contribution
FM and KD conceived and designed the paper. FM, KD, NN, SKJ, and MAS analyzed the data and wrote the paper. All authors participated in the preparation of the manuscript and approved the final manuscript before submission.Acknowledgement
First of all, the principal investigator would like to thank her family especially her brother Mr. Abdu for their financial support. We would like to extend our appreciation to the Department of Medical Laboratory Sciences, College of Health Sciences, and School of Allied Health Science of Addis Ababa University is highly acknowledged for allowing us to do this project. We are most grateful to Mr. Yakob Mohammed for the overall effort he did to start the program and supported us in all issues required for the accomplishment of this manuscript. Finally, we would like to extend our gratitude to the study participants who participated in this study, the Armed Force Referral Teaching Hospital, and the staff members.
REFERENCES
- Dubey JP, Beattie CP. Toxoplasmosis of animal and man. Boca Raton FL. CRC Press Boca Raton. 1988:1-220.
- Dubey JP. Toxoplasma, Neospora, Sarcocystis, and other tissue cyst-forming coccidian of humans and animals. In Parasitic Protozoa, Kreier, J.P. 2nd ed. 1993;6:1-158.
- Dubey JP. Toxoplasmosis a waterborne zoonosis. Vet Parasitol. 2004;126:57-72.
- Rorman E, Zamir CS, Rilkis I, Ben-David H. Congenital toxoplasmosis-prenatal aspects of Toxoplasma gondii infection. Reprod Toxicol. 2006;21:458-472.
- Pons JC, Sigrand C, Grangeot-Keros L, Frydman R, Thulliez P. Congenital toxoplasmosis transmission to the fetus of a pre-pregnancy maternal infection. Presse Med. 1995;24:179-182.
- Petersen E, Dubey JP. Biology of toxoplasmosis. A comprehensive clinical guide. In: Toxoplasmosis, Joynson DHM, Wreghitt TG. Cambridge University, Cambridge UK, 2001:1-42.
- McCabe RE, Brooks RG, Dorfman RF, Remington JS. Clinical spectrum in 107 cases of toxoplasmic lymphadenopathy. Rev Infect Dis. 1987;9:754-774.
- Leblebicioglu H. Toxoplasmosis. Emedicine Pediatrics General Medicine.mht. 2010.
- Belanger F, Derouin F, Grangeot-Keros, Meyer L. Incidence and risk factors of toxoplasmosis in a cohort of human immunodeficiency virus-infected patients: 1988-1995. Clin Infect Dis. 1999;28:575-581.
- Mariuz P, Steigbigel RT. Toxoplasma infection in HIV-infected patients: A comprehensive clinical guide. In: Toxoplasmosis, Joynson DHM, Wreghitt TG. Cambridge University, Cambridge UK, 2001:147-177.
- Remington JS, McLeod R, Thulliez P, Desmonts G. Toxoplasmosis. In infectious disease of the fetus and newborn In. 6th edn, Elsevier Saunders, Philadelphia, 2006:947.
- Health Protection Agency. Investigation of toxoplasma in pregnancy. National Standard Method QSOP. 2010:59.
- Couvreur J. Infection in neonates and infants. In toxoplasmosis, a comprehensive clinical guide, Joynson DHM, Wreghitt TG. 2001:254-276.
- Montoya JG, Liesenfeld O. Toxoplasmosis. Lancet. 2004;363:1965-1976.
- Pappas G, Roussos N, Falagas ME. Toxoplasmosis snapshots: global status of Toxoplasma gondii seroprevalence and implications for pregnancy and congenital toxoplasmosis. Int J Parasitol. 2009;39:1385-1394.
- Elsheikha MH, Azab SM, Abousamra KN, Rahbar HM, Elghannam MD, Raafat D. Seroprevalence of and risk factors for Toxoplasma gondii antibodies among asymptomatic blood donors in Egypt. J Parasitol. 2009;104:1471-1476.
- Martinez E, Mago H, Rocha R, Pacheco M. Epidemiological findings and prevalence of Toxoplasma gondii antibodies in HIV-positive patients in Venezuelan hospital. Valencia Int Conf AIDS. 2002;7:12-14
- Walker M, Zunt JR. Parasitic central nervous system infections in immunocompromised hosts. CID. 2005;40:1005-1015.
- Uppal B, Aggarwal P, Perween N, Sud A. Seroprevalence of toxoplasma among HIV infected and HIV non-infected individuals in North India. Asian Pac J Trop Dis. 2015;5:15-18.
- Navia BA, Petito CK, Gold JW, Cho ES, Jordan BD, Price RW. Cerebral toxoplasmosis complicating the acquired immune deficiency syndrome: clinical and neuropath logical findings in 27 patients. Ann Neurol. 1986;19:224-238.
- Holliman RE. Serological study of the prevalence of toxoplasmosis in asymptomatic patients infected with human immunodeficiency virus. Epidemiol Infect. 1990;105:415-418.
- Uttah E, Ogban E, Okonofua C. Toxoplasmosis: A global infection, so widespread, so neglected. Int J Sci Res Publ. 2013;3:2250-3153.
- Hany ME, Manar SA, Nashwa KA, Mohammad HR, Doaa ME, Douaa R. Seroprevalence and risk factors for Toxoplasma gondii antibodies among asymptomatic blood donors in Egypt. Parasitol Res. 2009;104:1471-1476.
- Negash T, Tilahun G, Medhin G. Seroprevalence of Toxoplasma gondii in Nazaret town, Ethiopia. E Afri J PH. 2008;5:211-214.
- Lin YL, Liao YS, Liao LR, Chen FN, Kuo HM, He S. Seroprevalence and sources of Toxoplasma infection among indigenous and immigrant pregnant women in Taiwan. Parasitol Res. 2008;8:4-8.
- Walle F, Kebede N, Tsegaye A, Kassa T. Seroprevalence and risk factors for Toxoplasmosis in HIV infected and non-infected individuals in Bahir Dar, Northwest Ethiopia. Parasites Vectors. 2013;6:15.
- Yohanes T, Debalke S, Zemene E. Latent Toxoplasma gondii infection and associated risk factors among Hiv-infected individuals at Arba Minch Hospital, South Ethiopia. AIDS Res Treat. 2014:1-6.
- Shimelis T, Tebeje M, Tadesse E, Tegbaru B, Terefe A. Sero-prevalence of latent Toxoplasma gondii infection among HIV-infected and HIV-uninfected people in Addis Ababa, Ethiopia. BMC Res Notes. 2009;2:213.
- Aleme H, Getachew Tilahun, D fekada, Berhe N, Medhine G. Sereoprevalence of Immunoglobulin-G and of Immunoglobulin-M Anti-Toxoplasma gondii antibodies in human immunodeficiency virus infection/acquired immunodeficiency syndrome patients at Tikur Anbessa. Infect Dis Ther. 2013;1:1-5.
- Amuta EU, Amali O, Jacob SE, Houmsou RS. Toxoplasma gondii IgG antibodies in HIV/AIDS patients attending hospitals in Makurdi metropolis, Benue state, Nigeria. Int J Med Biomed Res. 2012;1:186-192.
- Okwuzu JO, Odunukwe NN, Ezechi OC, Gbajabiamila TA, Musa AZ, Ezeobi PM, et al. Toxoplasma gondii infection in HIV/AIDS: prevalence and risk factors. Afr J Clin Exp Microbiol. 2014;15:97-102.
- John W, Mcbride H, Base C. Seroprevalence of anti-Toxoplasma gondii antibodies in HIV/AIDS patients and healthy blood donors at the Port Moresby General Hospital, Papua New Guinea. PNG Med J. 2012;55:88-93.
- Daryani A, Sharif M, Meigouni M. Seroprevalence of IgG and IgM anti-Toxoplasma antibodies in HIV/AIDS patients, northern Iran. Asian Pac J Trop Med. 2011;4:271-274.
- Nissapatorn V, Lee CKC, Cho SM, Rohela M, Anuar AK, Quek KF, et al. Toxoplasmosis in HIV/AIDS patients in Malaysia. Southeast Asian J Trop Med Public Health. 2003;34:80-85.
- Djurkovic-djakovic O, Bobic B. Risk for Toxoplasmic encephalitis in AIDS patients in Yugoslavia. Int J Infect Dis. 1997;2:74-78.
- Galván Ramírez ML, Valdez Alvarado V, Vargas Gutierrez G, Jiménez González O, García Cosio C, Vielma Sandoval M. Prevalence of IgG and IgM anti-Toxoplasma antibodies in patients with HIV and Acquired Immunodeficiency Syndrome (AIDS). Rev Soc Bras Med Trop. 1997;30:465-467.
- Sukthana Y. Toxoplasmosis beyond animals to humans. Trends in Parasitology. 2006;22:137-142.
- Meisher YV, Mehta S, Petel U. A prospective study of sero-prevalence of toxoplasmosis in general population and in HIV/AIDS patients in Bombay India. J Postgrad Med. 1997;43:93-97.
- Gongora-Biach RA, Gonzalez-Martinez P, Castro-Sansones C, Alvarez-Moquel R, Pavia-Ruz N. Antibodies against Toxoplasma gondii in patients with HIV in Yucatan. Rev Invest Clin. 1998;50:419-222.
- Hari KR, Modi MR, Ochan AH, Modi G. Reduced risk of toxoplasma encephalitis in HIV Infected patients-a prospective study from Gauteng, South Africa. Int J STD AIDS. 2007;18:555-558.
- Nissapatorn V, Kamaru I, Zaman A, Init L, Tan LH, Rohela M, et al. Seroepidemiology of toxoplasmosis among HIV infected patients and healthy blood donors. Med J Malaysia. 2002;57:304-310.
- Brindle R, Holliman R, Gilles C, Wayaki P .Toxoplasma antibodies in HIV positive patients from Nairobi. Trans R Soc Trop Med Hyg. 1991;85:750-751.
Citation: Mohammed F, Sinishaw MA, Nurahmed N, Juhar SK, Desta K (2019) Sero Burden of Toxoplasma gondii and Associated Risk Factors among HIV Infected Persons in Armed Forces Referral and Teaching Hospital, Addis Ababa, Ethiopia. J Trop Dis 8:341. doi: 10.35248/2329-891X. 19.8.341
Copyright: © 2019 Mohammed F, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.

