Indexed In
- Genamics JournalSeek
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2020) Volume 9, Issue 1
Safety Culture in the Neonatal Intensive Care Unit: Comparing the Pediatric Postgraduates and Nurses Using the Safety Attitude Questionnaire
Pooja Kunde, Kavitha Sreekumar* and Silveira MPReceived: 08-Nov-2019 Published: 13-Feb-2020, DOI: 10.35248/2167-0897.20.9.272
Abstract
Background: Evidence shows that neonates in the Neonatal Intensive Care Unit (NICUs) experience a significantly higher potential for medication errors and adverse events rate than do patients in other wards of the hospital. This necessitates the assessment of the safety culture in the (NICU) which can help to identify areas that can lead to errors in the unit.
Methods: This was cross sectional study done in the Neonatal unit, where the pediatric postgraduates resident doctors (PGs) and nurses were surveyed regarding the safety practices. The Safety Attitude Questionnaire (SAQ) which is validated and has good psychometric properties was used. Mean and Standard deviations for the six domains (job satisfaction, safety climate, teamwork climate, working conditions, perception of management and stress recognition) was analysed and unpaired t test was used to compare the means.
Results: Total of 31 responses was obtained (12 PGs and 19 nurses). Overall mean scores for the SAQ were 70.2 for PGs and 63.8 for nurses, suggesting an overall negative response. Mean scores for PGs ranged from 63 (working condition) to 82.8 (stress recognition) and for nurses 48.6 (working conditions) to 82.8 (job satisfaction). There was statistically significant difference between the PGs and nurses in the domain of job satisfaction with p value of 0.03. Rest of the domains showed no significant difference.
Conclusion: The scores suggest an overall negative response regarding safety culture in NICU. The variations among the Postgraduates and nurses suggest that we need customise the policies for both groups when we attempt to improve the safety culture in the unit while focussing on promoting teamwork.
Keywords
Safety culture; Safety attitude questionnaire; Neonatal intensive care unit
Introduction
Patient safety is aimed at preventing medical errors before they cause mortality or morbidity. Medical errors affect 1 in 10 patients globally and their implications may include death, short term or long term harm, financial loss, and psychosocial harm to the patient and caregiver [1]. A NICU is a high risk scenario for serious medical errors. Preterm infants are fragile, often very ill, and exposed to complex and prolonged intensive health care interventions. This makes the working environment vulnerable to lapses in teamwork and patient safety [2]. Healthcare workers in the NICU setting may particularly struggle to balance work and personal lives while trying to deliver optimal care to the sickest neonate resulting in a high and sustained level of stress that causes physical and emotional burnout. Eventually burnout can have adverse effects on the quality of patient care and potentially tragic consequences for patients [3]. Safety culture was defined by the Health and Safety Commission as “the product of individual and group values, attitudes, perceptions, competencies, and patterns of behaviour that determine the commitment to, and the style and proficiency of, an organization's health and safety management” [4]. A strong safety culture in health care organizations contributes to the promotion of an environment that enables the provision of safe care [5] and therefore, reduces the number of errors. In order to transform culture it is important to first understand and confront it. Generally in our set up, adverse events are individually discussed as and when they occur and changes are advised to prevent similar events in the future. So we rationalised that assessing and improving the overall safety culture in the NICU would help to prevent errors in a better way. So this study was conducted to evaluate the safety culture among the postgraduates and nurses working in the NICU using the Safety Attitude Questionnaire. The Safety Attitudes Questionnaire (SAQ) that was developed by Sexton and colleagues [6] at the University of Texas Houston and has been widely used to assess the safety climate across many intensive care settings. It has good psychometric properties, and is responsive to interventions [6].
Research Methodology
The study used a cross-sectional design. Data was collected between April and July 2019. The study population consisted of all the Paediatric Postgraduates (n=15) who have undergone neonatal posting and nurses (n=30) working in the neonatal unit for at least 3 months. SAQ was administered to the study population using the Google forms application. The survey was adapted for PGs and nurses. The SAQ consisted of 30 items grouped in six domains: teamwork climate, safety climate, job satisfaction, perceptions of management, working conditions, and stress recognition. Each item was answered using a 5-points Like scale (1=disagree strongly, 2=disagree slightly, 3=neutral, 4=agree slightly, 5=agree strongly). These scores were later converted to a 100-points scale during analysis to facilitate interpretation of the results (1=0, 2=25, 3=50, 4=75 and 5=100). Each domain score equals the mean score of its component survey items. The scores of the two negatively worded survey items were reversed [6]. A positive score is defined as 75 or more on 100-points scale [6]. The mean for the scale was calculated by dividing the composite score by the number of items. Finally, the percentages of positive responses for the survey scales and items were calculated. Positive responses in positively worded survey items were ‘agree/strongly agree’ and in negatively worded items were ‘disagree/strongly disagree’. Descriptive statistics including percentages, means and standard deviations were used for all survey items and domains. The scores were compared using the unpaired t-test. P value of less than 0.05 was considered significant.
Results
Total of 31(12 PGs and 19 nurses) responses were obtained with a response rate of 67%. Among the PGs, 6 were in the first year, 5 from the second year and 1 was in the 3rd year of the course. Among the nurses, all of them had completed more than one year in the NICU.
Table 1 shows the respondents' ratings of the SAQ items and scales as well as the percentages of positive responses along with the p value for each item. Overall mean scores for the SAQ were 70.2 for PGs and 63.8 for nurses, both of which are below 75 suggesting an overall negative response. Mean scores for PGs ranged from 63 (working condition) to 82.8 (stress recognition) and for nurses 48.6 (working conditions) to 82.8 (job satisfaction). There was statistically significant difference between the PGs and nurses in the domain of stress recognition with p value of 0.04. Rest of the domains showed no significant difference.
| SAQ items | Postgraduates (n=12) | Nurses (n=19) | P-values | |||||
|---|---|---|---|---|---|---|---|---|
| Item | Mean | SD | % positives | Mean | SD | % positives | - | |
| Job Satisfaction | 71.246 | 26.39 | 68.33 | 82.36 | 22.03 | 77.89 | 0.03 | |
| 1 | I like my job | 70.83 | 25.7 | 58.33 | 88.1 | 17.4 | 89.47 | 0.0554 |
| 2 | Working in this hospital is like being part of a large family | 66.66 | 26.8 | 66.66 | 82.8 | 22.1 | 84.21 | 0.0948 |
| 3 | This hospital is a good place to work | 68.75 | 26.35 | 75 | 88.15 | 19.3 | 84.21 | 0.0405 |
| 4 | I am proud to work at this hospital | 79.16 | 17.9 | 83.33 | 84.21 | 23.8 | 78.94 | 0.5089 |
| 5 | Morale in this NICU is high | 70.83 | 35 | 58.33 | 68.42 | 27.4 | 52.63 | 0.8418 |
| Safety Climate | 66.96 | 26.62 | 69.044 | 63.1 | 26.1 | 57.3 | 0.56 | |
| 1 | I would feel safe being treated here as a patient | 81.25 | 28.4 | 83.33 | 61.8 | 32.6 | 47.3 | 0.0927 |
| 2 | Medical errors are handled appropriately at this NICU | 79.16 | 27.8 | 91.66 | 64.4 | 29.2 | 52.6 | 0.1733 |
| 3 | I receive appropriate feedback about my performance | 70.83 | 14.4 | 75 | 52.63 | 24.8 | 42.1 | 0.3985 |
| 4 | In this NICU, it is difficult to discuss errors* | 66.6 | 34.2 | 75 | 43.4 | 32 | 36.8 | 0.2345 |
| 5 | I am encouraged by my colleagues to report any patient safety concerns I may have | 47.91 | 27 | 41.66 | 72.3 | 24.8 | 73.6 | 0.6789 |
| 6 | The culture in this NICU makes it easy to learn from the errors of others | 60.41 | 27 | 50 | 82.8 | 16 | 89.4 | 0.2298 |
| 7 | I know the proper channels to direct questions regarding patient safety in this NICU | 62.5 | 27.1 | 66.66 | 64.4 | 26.7 | 57.8 | 0.0326 |
| Teamwork Climate | 73.26 | 27.39 | 74.99 | 66.8 | 28.9 | 66.6 | 0.319 | |
| 1 | Personnel input about patient care is well received in this NICU | 66.6 | 26.8 | 58.33 | 73.68 | 28.2 | 73.68 | 0.4935 |
| 2 | In this NICU, it is difficult to speak up if I perceive a problem with patient care* | 62.5 | 31 | 66.66 | 48.68 | 29.4 | 31.57 | 0.2312 |
| 3 | Disagreements in this NICU are appropriately resolved (i.e., not who is right, but what is best for the patient) | 75 | 26.1 | 83.33 | 61.84 | 34.7 | 68.42 | 0.2403 |
| 4 | I have the support I need from other personnel to care for patients | 79.16 | 23.4 | 83.33 | 61.84 | 34.7 | 68.42 | 0.1082 |
| 5 | It is easy for personnel in this NICU to ask questions when there is something that they do not understand | 77.08 | 27 | 83.33 | 86.84 | 19.3 | 84.21 | 0.2918 |
| 6 | The physicians and nurses here work together as a well-coordinated team | 79.16 | 29.8 | 75 | 68.42 | 27.4 | 73.68 | 0.3247 |
| Working Conditions | 63.017 | 28.11 | 64.577 | 48.68 | 29.52 | 39.46 | 0.149 | |
| 1 | This hospital does a good job of training new personnel | 68.75 | 21.6 | 66.66 | 23.68 | 28.2 | 15.78 | 0.0706 |
| 2 | All the necessary information for diagnostic and therapeutic decisions is routinely available to me | 60.41 | 27 | 58.33 | 60.52 | 31.5 | 47.36 | 0.3967 |
| 3 | This hospital deals constructively with problem personnel | 56.25 | 32.2 | 58.33 | 55.26 | 24.4 | 42.1 | 0.97 |
| 4 | Trainees in my discipline are adequately supervised | 75 | 26.1 | 91.66 | 55.26 | 33.9 | 52.63 | 0.0793 |
| Perception of Management | 59.9 | 27.8 | 58.3 | 49.5 | 20.8 | 35.5 | 0.4049 | |
| 1 | Hospital administration supports my daily efforts | 54.16 | 33.4 | 50 | 55.26 | 21.3 | 31.57 | 0.92 |
| 2 | Hospital management does not knowingly compromise the safety of patients | 81.25 | 18.8 | 83.33 | 61.84 | 19.3 | 52.63 | 0.0107 |
| 3 | The levels of staffing in this NICU are sufficient to handle the number of patients | 47.9 | 27.1 | 41.8 | 23.1 | 20.5 | 15.7 | 0.07 |
| 4 | I am provided with adequate, timely information about events in this hospital that might affect my work | 56.25 | 32.2 | 58.33 | 57.89 | 22.1 | 42.1 | 0.8591 |
| Stress Recognition | 82.8 | 20.42 | 81.245 | 61.83 | 30.92 | 61.84 | 0.0725 | |
| 1 | When my workload becomes excessive, my performance is impaired | 91.66 | 12.3 | 100 | 72.36 | 27.5 | 73.68 | 0.0128 |
| 2 | I am less effective at work when fatigued | 87.5 | 16.8 | 91.66 | 67.1 | 27.7 | 68.42 | 0.0163 |
| 3 | I am more likely to make errors in hostile or tense situations | 79.16 | 23.4 | 66.66 | 69.73 | 31.8 | 68.42 | 0.3514 |
| 4 | Fatigue impairs my performance during emergency situations | 72.91 | 29.1 | 66.66 | 38.15 | 36.6 | 36.84 | 0.0068 |
*Scores were reversed
Table 1: SAQ items, scales' mean scores, standard deviations and percentages of positive responses.
When the two statement responses for burnout were evaluated, 42% of nurses said they felt burned out and 58% of PGs reported burn out [7].
Discussion
Promoting a culture of safety has become one of the pillars of the patient safety movement. Professional and organizational cultures in health care must undergo a change with an aim to promote safer patient care.
Measurement of safety culture in the NICU setting may be particularly needed as preterm infants are fragile, often very ill, and exposed to complex and prolonged intensive health care interventions. These circumstances make preterm infants vulnerable to lapses in patient safety [2]. In our study, overall there was a negative response in all the domains except stress recognition in the PGs group and job satisfaction among the Nurses group. In most studies the nurses show a lower score than physicians but it is not consistent [5,8] and varies with individual domains as is seen in our study.
Job satisfaction
In this domain, the nurses showed a positive response compared to the PGs (82.36 vs. 71.2) even though they had negative response in other related domains like working conditions and perception of management. This was the only domain where the difference between the two groups was found to be statistically significant (pvalue 0.03). This finding is similar to the results found in another study done by Mcdonald et al. who showed that Neonatal nurses were satisfied with their jobs and the work environment in the NICU [9]. There is a significant difference between the two groups for the item “this hospital is a good place to work” with PGs giving a negative response. This could be related to the workload and stress associated with the job which might be leading to burnout and hence a negative response to the work environment. A study done is related to career choice regret [10]. The use of instruments that evaluate burnout among health care professionals can help us identify early signs and take measures to alleviate stress and work related anxiety among them.
Safety climate
Safety climate is one of the critical dimensions of patientsafety that mainly focuses on reporting and learning fromevents that occur. Both the group of participants gave a negative score to safety climate. Both groups pointed out that it is difficult to discuss errors in the NICU and there were no proper channels to direct questions regarding patient safety. This finding is similar to studies done by Abu et al. and Hamden et al. [5,8]. This type of an attitude arises from the fact that the current tendency to react to errors is the “blame and shame” culture which prevents healthcare personnel to readily acknowledge and report an error and therefore obstructs any possibility of learning from it. Safety improvement requires that systems have ready availability of information that supports learning from experience which will promote a system that prevents errors and lessen the impact of errors that occur [11]. Haerkens et al. [12] argued that the typical culture in the ICU doesn't allow junior staff to question the decisions made by senior staff which adds to the challenge. Evidence showed that complete unit-based safety programs that provided an outline for looking into patient safety culture issues can improve work force sensitivities and therefore improve safety culture [12].
Teamwork climate
In a study of voluntarily reported errors in the NICU setting, poor teamwork and poor communication contributed to errors in 9% and 22%, respectively [2].
Team performance is especially important in emergent situations where a rescue team must assemble quickly, communicate clearly and collaborate effectively to avoid needless morbidity or mortality [13]. In our study, the teamwork climate domain had mean scores of 73.26 and 66.8 for PGs and nurses respectively (Figure 1). But one of the items in this domain (In this NICU, it is difficult to speak up if I perceive a problem with patient care) had only a 31.5% positive responses from the nurses. This could point out that there is an element of moral distress among the nurses. In a study done by Prentice et al. the primary causes of moral distress were perceived disproportionate care, which is not in a patient’s best interests and a perceived inability on the part of the nursing staff to protect the child. Moral distress can have negative impact on the quality, quantity, and cost of patient care and can lead to job dissatisfaction and burnout [14]. Better communication with the nursing personnel and involving them in management decisions as well as taking feedback regarding patient condition would help them to express concerns regarding possible adverse effects of an intervention. In a study done by Ciccone et al. [15], introduction of “care managers” in management of patients helped to improve the communication between the physicians, nurses and the patients which led to better adherence to treatment and good lifestyle changes which had a significant impact on the cardiovascular parameters. Having a similar concept in the neonatal intensive care setup, where the care managers are specialised trained nurses, would help to improve communication not only between the doctors and the parents of the babies admitted in the NICU but also act as a communication bridge between the doctors and the nurses. It could also help to empower nurses in the NICU to express their opinions and work towards reducing moral distress.
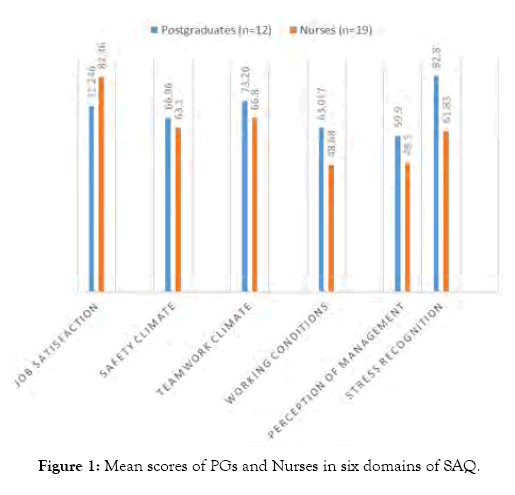
Figure 1: Mean scores of PGs and Nurses in six domains of SAQ.
Working conditions
Even though not statistically significant, the nurses had a much lower mean score in this domain compared to the PGs (48.6 vs. 63.0). Of note was the item, ‘This hospital does a good job of training new personnel’, which had a mere 15% positive response from the nurses. This is different from the findings of other studies which used the SAQ where the participants gave a positive score for this item [2,5,8]. This difference points to an existing lack of an orientation and training program for the new nurses recruited in the NICU in our set up. Unlike the doctors who are oriented before the posting in the NICU and also get an opportunity to attend training sessions pertaining to neonatal care as part of their Postgraduate curriculum, nurses employed in the NICU do not have any such orientation or continuous learning opportunity, Interventions that may improve working conditions may include dealing positively with staff difficulties, providing training support, and make information routinely available to staff to perform their duties [5].
Perception of management
The scores on this domain were below 75 for both groups which was similar to findings of other studies done in NICU. The item which scored the lowest was in regard to adequate staffing. This was seen in other studies as well. Such shortage of staff may affect the safety of provided care and may lead to an increase in the number of errors. Open communication, support of team work, rewards for reporting, allocation of appropriate resources and senior executive walk rounds to demonstrate senior leadership commitment to patient safety are all means to improve ‘perception of management’ and thereby the safety culture [16].
Stress recognition
This domain showed that the PGs have a positive attitude towards stress recognition compared to the nurses (82.8 vs. 61.3). In NICUs, nurses and doctors provide specialized care to patients who are critically ill and have unstable vital functions along with a high mortality rate. This can lead to high levels of stress that can impair the quality of work. Our finding in this domain is different from other studies done, which show that both doctors and nurses have low stress recognition scores. So unlike in other set ups, nurses in our unit responded that excess workload does not impact their work output except in emergency situations.
This study provides a very useful insight as to what are the safety attitudes among the health care professionals who are directly caring for the sick newborn. It highlights the most important factors that need to be worked upon to improve safety culture and in turn reduce errors in the NICU. The study also brings out the point that the perceptions of the PGs and nurses towards the safety culture are quite varied; hence when we plan interventions, we should customize them according to the professional roles and not apply the same interventions to the whole healthcare group catering to the neonates.
Strengths and Limitations
The strength of the study is that we used a validated instrument which covered all aspects of safety cultures. The limitations are the response rates is 73%. The less than optimal response rate could be that nurses do not freely express their views in the NICU which is also reflected in the study. Many of the responses were given as neutral, which could again be an indication of the above observation or it could be that the question was not very well understood by the respondent.
Conclusion
This study revealed a predominantly negative response of safety attitudes in all the SAQ subscales and identified opportunities for improving the patient safety culture in NICUs. Shortage of staff, increased workload and absence of standard protocols for reporting errors and getting feedback were the items that had the poorest positive response. Hence there is an urgent need to plan and implement programs and policies mainly in the domains of safety climate, working conditions and perception of management to improve safety culture in the NICU. There is a variation in attitudes towards safety among the PGs and nurses which should be kept in mind while planning a safety improvement strategy, but at the same time focussing on team work to create an error free healthcare system for the neonates.
Acknowledgement
All the Pediatric postgraduates and Nurses working in the NICU.
REFERENCES
- Samra HA, McGrath JM, Rollins W. Patient safety in the NICU: a comprehensive review. J Perinat Neonatal Nurs. 2011;25:123-32.
- Profit J, Etchegaray J, Petersen LA, Sexton JB, Hysong SJ, Mei M, et al. The Safety Attitudes Questionnaire as a tool for benchmarking safety culture in the NICU. Arch Dis Child Fetal Neonatal Ed. 2012;97:127-132.
- Profit J, Sharek PJ, Amspoker AB, Kowalkowski MA, Nisbet CC, Thomas EJ, et al. Burnout in the NICU setting and its relation to safety culture. BMJ Qual Saf. 2014;23:806-13.
- Health and Safety Commission. Organising for safety: third report of the human factors study group of ACSNI (Advisory Committee on the Safety of Nuclear Installations).
- Hamdan M, Saleem AA. Assessment of patient safety culture in Palestinian public hospitals. Int J Qual Health Care. 2013;25:167-75.
- Sexton JB, Helmreich RL, Neilands TB, Rowan K, Vella K, Boyden J, et al. The Safety Attitudes Questionnaire: psychometric properties, benchmarking data, and emerging research. BMC Health Serv Res. 2006;6:44.
- West CP, Dyrbye LN, Satele DV, Sloan JA, Shanafelt TD. Concurrent validity of single-itemmeasures of emotional exhaustion anddepersonalization in burnout assessment. J Gen Intern Med. 2012;27:1445-1452.
- Abu-El-Noor NI, Hamdan MA, Abu-El-Noor MK, Radwan AK, Alshaer AA. Safety Culture in Neonatal Intensive Care Units in the Gaza Strip, Palestine: A Need for Policy Change. J Pediatr Nurs. 2017;33:76-82.
- McDonald K, Rubarth LB, Miers LJ. Job satisfaction of neonatal intensive care nurses. Adv Neonat Care. 2012;12:1-8.
- Dyrbye LN, Burke SE, Hardeman RR, Herrin J, Wittlin NM, Yeazel M, et al. Association of clinical specialty with symptoms of burnout and career choice regret among US resident physicians. Jama. 2018 Sep 18;320(11):1114-30.
- Reason J. Organizational accidents: the management of human and organizational factors in hazardous technologies. England: Cambridge University Press, Cambridge. 1997.
- Haerkens MH, Jenkins DH, van der Hoeven JG. Crew resource management in the ICU: the need for culture change. Ann Intensive Care2012;2:39.
- Clarke SP, Aiken LH. Failure to rescue. Am J Nurs. 2003;103:42-7.
- Prentice T, Janvier A, Gillam L, Davis PG. Moral distress within neonatal and paediatric intensive care units: a systematic review. Arch Dis Child. 2016;101:701-8.
- Ciccone MM, Aquilino A, Cortese F, Scicchitano P, Sassara M, Mola E, et al. Feasibility and effectiveness of a disease and care management model in the primary health care system for patients with heart failure and diabetes (Project Leonardo). Vasc Health Risk Manag. 2010;6:297.
- Frankel A, Grillo SP, Pittman M, Thomas EJ, Horowitz L, Page M, et al. Revealing and resolving patient safety defects: the impact of leadership Walk Rounds on frontline caregiver assessments of patient safety. Health Serv Res. 2008;43:2050-2066.
Citation: Sreekumar K, Kunde P, Silveira MP (2020) Safety Culture in the Neonatal Intensive Care Unit: Comparing the Pediatric Postgraduates and Nurses Using the Safety Attitude Questionnaire. J Neonatal Biol 9:272. doi: 10.35248/2167-0897.20.9.272
Copyright: © 2020 Sreekumar K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

