Indexed In
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
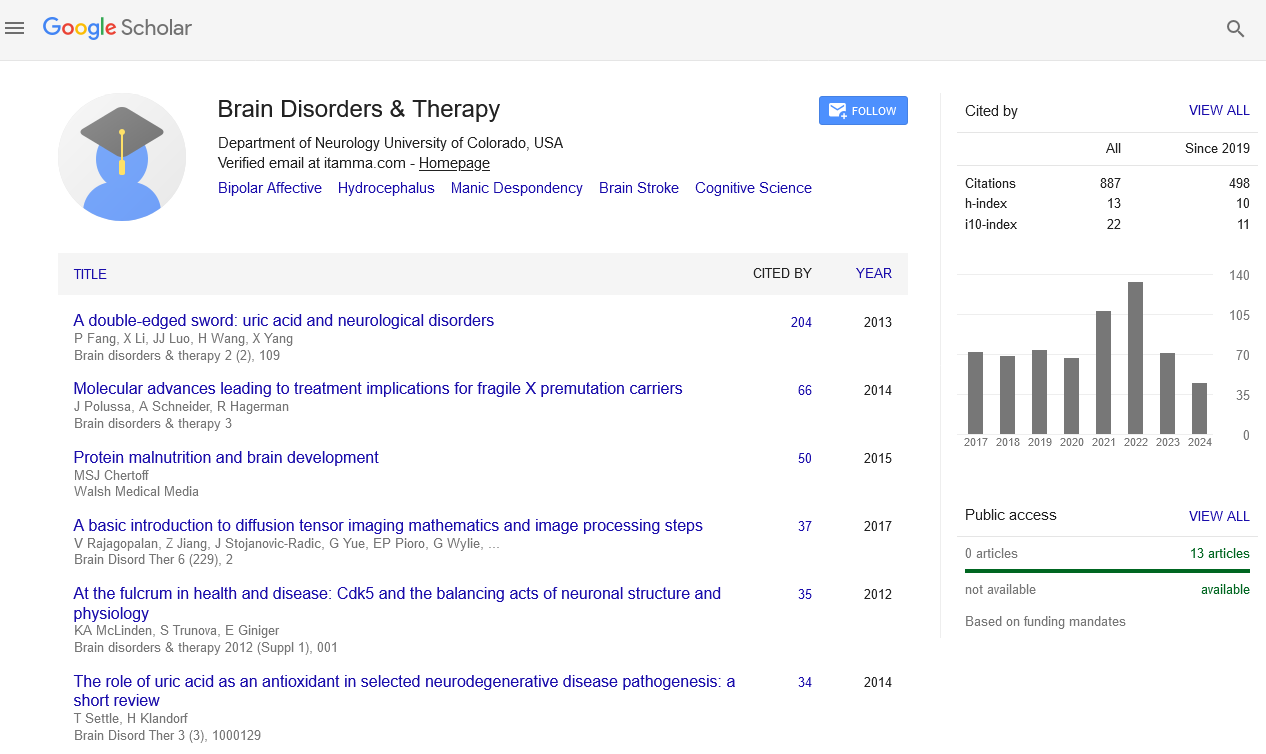
- Publons
- Geneva Foundation for Medical Education and Research
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Commentary - (2024) Volume 13, Issue 2
Role of Pressure Reactivity Index in Modern Traumatic Brain Injury Treatment
Caine Sutherland*Received: 28-May-2024, Manuscript No. BDT-24-26018; Editor assigned: 31-May-2024, Pre QC No. BDT-24-26018 (PQ); Reviewed: 14-Jun-2024, QC No. BDT-24-26018; Revised: 21-Jun-2024, Manuscript No. BDT-24-26018 (R); Published: 28-Jun-2024, DOI: 10.35248/2168-975X.24.13.260
Description
Traumatic Brain Injury (TBI) is a critical medical condition that necessitates immediate and effective management to prevent long-term neurological damage or death. Cerebral autoregulation, the brain's ability to maintain stable blood flow despite changes in systemic blood pressure, plays a pivotal role in TBI management. The Pressure Reactivity Index (PRx) is a dynamic marker used to assess cerebral autoregulation, offering valuable insights into the condition of patients with TBI. This article delves into the significance of Pressure Reactivity Index, its methodology, and its application in managing TBI.
Understanding cerebral autoregulation
Cerebral autoregulation ensures consistent Cerebral Blood Flow (CBF) by adjusting the diameter of cerebral blood vessels in response to fluctuating blood pressures. This mechanism is crucial for preventing ischemia or hyperperfusion, which can lead to further brain damage. Impaired autoregulation is often observed in TBI patients, making it a critical factor to monitor.
The pressure reactivity index
The pressure reactivity index is a calculated parameter that reflects the relationship between Intracranial Pressure (ICP) and Arterial Blood Pressure (ABP). It is obtained by computing the moving correlation coefficient between slow waves of ICP and ABP. A positive pressure reactivity index indicates impaired autoregulation, where an increase in ABP leads to an increase in ICP, while a negative pressure reactivity index suggests intact autoregulation.
Pressure reactivity index measurement
To measure pressure reactivity index, continuous monitoring of ICP and ABP is required. Typically, this involves invasive techniques such as intraparenchymal probes or external ventricular drains for ICP monitoring, and arterial lines for ABP measurement. The data are collected and analyzed using specialized software that calculates the pressure reactivity index over time, providing a real-time assessment of cerebral autoregulation.
Clinical relevance of pressure reactivity index in TBI management
Predicting outcomes: Pressure reactivity index has been shown to correlate with patient outcomes. Higher pressure reactivity Index values, indicating impaired autoregulation, are associated with worse outcomes, including higher mortality rates and poor neurological recovery. This makes pressure reactivity index a valuable prognostic tool in TBI management.
Guiding therapeutic interventions: Monitoring pressure reactivity index can guide therapeutic decisions. For example, optimizing Cerebral Perfusion Pressure (CPP) based on pressure reactivity index values can help maintain adequate CBF while avoiding secondary brain injury. Clinicians can adjust interventions such as fluid management, vasopressor use, and ventilatory support to maintain optimal CPP.
Individualized patient care: The continuous assessment of pressure reactivity index allows for tailored treatment strategies for each patient. This personalized approach can enhance the effectiveness of interventions and improve overall patient outcomes.
Despite its advantages, the use of pressure reactivity index is not without challenges. Invasive monitoring techniques pose risks such as infection and bleeding. Additionally, the interpretation of pressure reactivity index requires expertise and understanding of its dynamic nature. Variability in pressure reactivity index values can occur due to factors like sedation, temperature changes, and patient movement, necessitating careful analysis and contextual understanding. Advancements in non-invasive monitoring techniques could potentially mitigate the risks associated with invasive methods. Technologies such as Near-Infrared Spectroscopy (NIRS) and Transcranial Doppler Ultrasound (TCD) are being explored for their ability to provide real-time assessments of cerebral autoregulation. Further research is needed to validate these methods and integrate them into clinical practice.
The pressure reactivity index is a valuable tool in the management of traumatic brain injury, offering insights into cerebral autoregulation and guiding therapeutic interventions. By providing real-time data on the status of cerebral blood flow regulation, pressure reactivity index aids in predicting patient outcomes, tailoring treatments, and potentially improving recovery rates. Despite the challenges associated with its use, ongoing advancements in monitoring technologies hold potential for enhancing the applicability and accuracy of pressure reactivity index in clinical settings. As research progresses, the integration of pressure reactivity index in to standard TBI management protocols could lead to better-informed clinical decisions and improved patient care.
Citation: Sutherland C (2024) Role of Pressure Reactivity Index in Modern Traumatic Brain Injury Treatment. Brain Disord The. 13:260.
Copyright: © 2024 Sutherland C. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.