Indexed In
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Access to Global Online Research in Agriculture (AGORA)
- Centre for Agriculture and Biosciences International (CABI)
- RefSeek
- Directory of Research Journal Indexing (DRJI)
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Scholarsteer
- SWB online catalog
- Publons
- Euro Pub
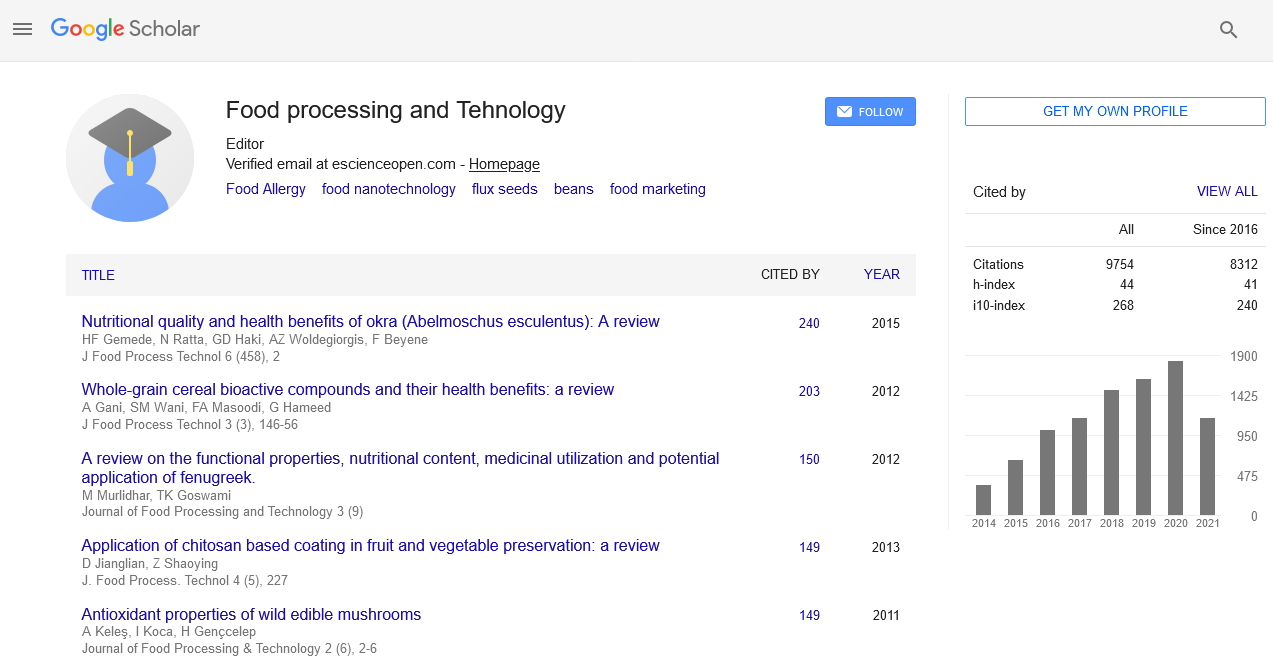
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Commentary - (2024) Volume 15, Issue 5
Role of Gut Microbiota in the Development and Management of Food Allergies
Heleny Joe*Received: 30-Sep-2024, Manuscript No. JFPT-24-26887; Editor assigned: 03-Oct-2024, Pre QC No. JFPT-24-26887 (PQ); Reviewed: 17-Oct-2024, QC No. JFPT-24-26887; Revised: 24-Oct-2024, Manuscript No. JFPT-24-26887 (R); Published: 31-Oct-2024, DOI: 10.35248/2157-7110.24.15.1124
Description
Food allergies have become a major public health concern, impacting millions of people throughout all of history. The immune system's abnormal response to typically harmless food proteins can lead to a range of symptoms, from mild discomfort to severe anaphylactic reactions. Recently it has begun to uncover the intricate relationship between the gut microbiota and food allergies, offering new perspectives on both the development and management of these conditions. The human gut microbiota comprises trillions of microorganisms, including bacteria, viruses, fungi and protozoa, residing primarily in the intestines. This complex community plays a critical role in various physiological processes, including digestion, metabolism and immune function. The balance of these microorganisms is essential for maintaining overall health and preventing disease. The gut microbiota is pivotal in shaping the immune system. During early life, exposure to diverse microbial communities helps to educate the immune system, promoting tolerance to harmless antigens and defense against pathogenic invaders. This educational process involves the development of regulatory T cells, which play a critical role in maintaining immune tolerance and preventing excessive immune responses.
Food allergies: An immune system dysfunction
Food allergies occur when the immune system mistakenly identifies a food protein as a threat, leading to an inappropriate immune response. This reaction is often mediated by Immunoglobulin E (IgE) antibodies, which trigger the release of histamines and other inflammatory mediators. The resulting symptoms can range from mild gastrointestinal discomfort to severe anaphylaxis.
Microbiota diversity and composition: A diverse and balanced gut microbiota is associated with a lower risk of developing allergies. For instance, reduced microbial diversity in the gut has been linked to an increased risk of allergies, including food allergies. Certain beneficial bacteria, such as Lactobacillus and Bifidobacterium, are known to promote immune tolerance and may help prevent allergic responses.
Gut barrier function: The gut microbiota helps maintain the integrity of the intestinal barrier, which is essential for preventing the entry of allergens into the bloodstream. A healthy gut barrier restricts the passage of undigested food particles and harmful substances, reducing the likelihood of systemic immune responses. Dysbiosis, an imbalance in the gut microbiota, can lead to a compromised gut barrier and increased permeability, known as "leaky gut," which may contribute to the development of food allergies.
Immune system modulation: Gut microbiota influences the immune system through the production of metabolites and signaling molecules. Regulation T cell activity is improved and immunological tolerance is promoted by Short-Chain Fatty Acids (SCFAs), which are generated when gut bacteria ferment dietary fibers. Additionally, certain gut bacteria can produce antimicrobial peptides that support a balanced immune response and prevent the overgrowth of pathogenic microorganisms.
The early life environment plays an essential role in shaping the gut microbiota and, consequently, immune system development. Factors such as mode of delivery (vaginal birth versus cesarean section), antibiotic use and dietary practices (e.g., breastfeeding versus formula feeding) can significantly impact the establishment of the gut microbiota. For example, breastfeeding promotes the growth of beneficial bacteria, such as Bifidobacterium, which are associated with a lower risk of developing allergies.
Managing food allergies through gut microbiota
Potential management and possibly preventive treatments for food allergies become available with an understanding of the involvement of gut bacteria in these conditions:
Prebiotics against probiotics: The gut microbiota can be improved or restored by taking probiotics, which are live beneficial bacteria. Some studies suggest that probiotic supplementation may reduce the incidence of allergies in high-risk infants. Prebiotics, which are non-digestible fibers that promote the growth of beneficial bacteria in supporting a healthy gut microbiota and potentially reducing allergy symptoms.
Dietary interventions: Diet plays a significant role in shaping the gut microbiota. A diet rich in diverse, fiber-containing foods supports microbial diversity and health. Conversely, a diet high in processed foods and low in fiber can negatively impact gut microbiota composition and function. Individuals with food allergies might benefit from dietary adjustments that promote a balanced microbiota and support immune health.
Fecal microbiota transplantation: Fecal Microbiota Transplan- tation (FMT), the process of transferring fecal material from a healthy donor to a recipient, has shown potential in restoring a balanced gut microbiota. While primarily used for treating conditions like Clostridium edificial infection, FMT is being explored as a potential therapy for various allergic conditions, including food allergies. However, more research is needed to establish its safety and efficacy for this purpose.
Further elucidate the complex interactions between gut microbiota, immune system development and food allergies. Large-scale clinical trials and longitudinal studies are needed to confirm the effectiveness of microbiota-based interventions and to identify the most beneficial strains of probiotics or prebiotics. Additionally, personalized approaches, considering individual variations in gut microbiota composition, may lead to more effective management strategies for food allergies. Advances in genomic and microbiome study for developing targeted therapies that could transform the treatment landscape for food allergies. The gut microbiota plays an important role in the development and management of food allergies. By influencing immune system development, gut barrier function and immune modulation, a balanced microbiota can help prevent and manage allergic responses. As research continues to uncover the intricate connections between gut health and food allergies, new therapeutic strategies may emerge, offering hope for better management and potentially even prevention of these challenging conditions.
Citation: Joe H (2024). Role of Gut Microbiota in the Development and Management of Food Allergies. J Food Process Technol. 15:1124.
Copyright: © 2024 Joe H. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.