Indexed In
- Open J Gate
- Genamics JournalSeek
- CiteFactor
- Cosmos IF
- Scimago
- Ulrich's Periodicals Directory
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- Directory of Abstract Indexing for Journals
- OCLC- WorldCat
- Proquest Summons
- Scholarsteer
- ROAD
- Virtual Library of Biology (vifabio)
- Publons
- Geneva Foundation for Medical Education and Research
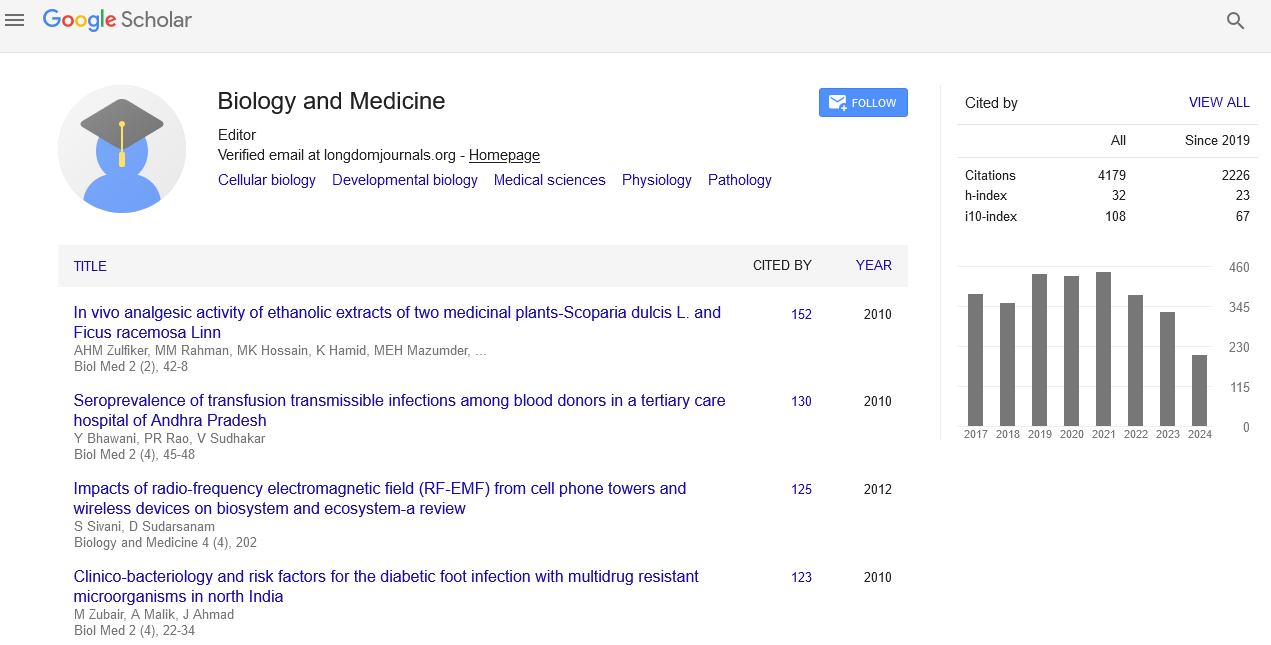
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2024) Volume 16, Issue 4
Risk of Alzheimer's Disease in People with Diabetes Mellitus
Muhammad Umer Zaheer Khan1, Abdul Raheem Tunio2, Shafaque Batool3, Kausar Abbas Saldera4, Rizwan Lakho5, Ufaque Batool K. Samo4* and Jehan Zaib Arshad62Department of General Medicine, Mohterma Shaheed Benazir Bhutto Hospital, Quetta, Pakistan
3Department of Physiology, Gambat Institute of Medical Sciences (GIMS), Gambat, Pakistan
4Department of Physiology, Basic Medical Sciences Institute(BMSI), Jinnah Postgraduate Medical Centre, Karachi, Pakistan
5Department of Urology, Teaching Hospital SMBBMU (Shaheed Mohtarma Bhutto Benazir Medical University), Larkana, Pakistan
6Department of Clinical Pathology, Jinnah Post Graduate Medical Centre, Karachi, Pakistan
Received: 20-Mar-2024, Manuscript No. BLM-24-25196; Editor assigned: 22-Mar-2024, Pre QC No. BLM-24-25196 (PQ); Reviewed: 05-Apr-2024, QC No. BLM-24-25196; Revised: 12-Apr-2024, Manuscript No. BLM-24-25196 (R); Published: 19-Apr-2024, DOI: 10.35248/0974-8369.23.15.671
Abstract
Background: Diabetes Mellitus (DM) may increase the risk of Alzheimer’s disease (AD) in a number of biologically conceivable ways, although how DM and the development of AD are related is still unclear.
Objective: To assess the risk of AD in subjects with and without DM.
Design: Prospective community-based cohort study.
Participants: Framingham Research Participants (n=2210; 1325 women; mean age, 70 years) who were part of the first cohort, did not have dementia and did not participate in the biennial test.
Results: Relative risk of incident Alzheimer’s disease within the overall group and within subgroups defined by plasma homocysteine levels and apolipoprotein E genotype (based on criteria from the National Institute of Neurological and Communicative Diseases and Stroke/Association for Alzheimer’s Disease and Related Disorders); models were adjusted for age, sex, and cardiovascular risk factors. At baseline, 202 people (9.1%) had DM. During the follow-up period (mean, 12.7 years; range, 1-20 years), the risk of developing AD was 1.15 (95% confidence interval, 0.65-2.05) in 17 of 202 people with diabetes (8.1%) and 220 of 2008 people without diabetes (11.0%). Among the 684 participants, 44 (6.4%) did not have elevated plasma homocysteine levels or an apolipoprotein E4 allele; the relative risk of AD was 2.98 (95% confidence interval, 1.06-8.39; P=.03) in patients with diabetes compared to those without diabetes. The effect was greatest among individuals 75 years of age or older, with a relative risk of 4.77 (95% confidence interval, 1.28–17.72; P=.02).
Conclusion: Overall, Diabetes Mellitus did not increase the incidence of incident AD in the Framingham cohort; however, in the absence of other major risk factors for AD, Diabetes Mellitus may be a risk factor for AD.
Keywords
Diabetes Mellitus (DM); Alzheimer Disease (AD); Brain; Ageing
Introduction
Diabetes Mellitus (DM) has been associated with morphological measures of brain ageing, hippocampus and whole-brain shrinkage, cognitive impairment, an increased risk of stroke, and Vascular Dementia (VaD). It is unclear how DM and Alzheimer Disease (AD) are related; some previous research has detected a link, but others have not. These various results could be a result of differences in age, ethnicity, sex, and risk factor profiles; study designs; definitions of DM, dementia, VAD, and AD; and follow-up periods. In earlier studies linking DM to the risk of AD, the follow-up time was either quite brief (less than 6 years) or large. We previously noted that younger, APOE4 negative participants-those with the lowest a priori risk of developing dementia-had the highest probability of developing dementia after stroke. Furthermore, only those people who lacked APOE4 had a greater chance of developing AD due to insulin resistance. We therefore reasoned that the best way to show the connection between DM and AD would be to perform a long-term follow-up of participants who did not have the two primary recognized risk factors for AD (elevated plasma homocysteine (tHcy) level and the APOE4 genotype).
Materials and Methods
Birmingham the original cohort participants (n=2611) were enrolled in a dementia-free cohort between 2000 and 2022 based on their data from a standard battery of neuropsychological tests and subsequent biennial Mini-Mental State Testing and, in the case of individuals suspected of having cognitive problems, further evaluations by a neurologist. Our study sample consisted of 2210 patients (1325 women; mean age 70 years) from this cohort who were still free of dementia at the biannual examination (2000-2022). Informed consent was obtained from each participant after providing consent from the Institutional Review Board [1-3].
Diagnosis of incident dementia, AD, and VaD
Previous descriptions of dementia screening and follow-up procedures have been made. The Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition criteria were met by the participants who were classified as having dementia. Additionally, they had a clinically evident case of dementia (a score of 1 on the CDR scale) for a minimum of six months [4]. Participants with ADs met the criteria for definite or probable ADs set forth by the Alzheimer Disease Diagnostic and Treatment Centre, while those with VaD met the criteria for probable VaD established by the National Institute of Neurological and Communicative Diseases and Stroke. Only 32 individuals with multiple dementia-related causes were included in the study of all dementias.
Diagnosis of DM
DM was defined as follows: A documented history of using insulin, oral hypoglycemic medication, or a casual (nonfasting) plasma glucose level of more than or equal to 200 mg/dL (11.1 mol/L), as measured at the biannual assessment or at an earlier examination.
Definition of variables
Only 1139 people (51%) had available APOE genetic information since the remaining participants either passed away before they could decline to provide consent or had their DNA taken for genotyping. Two groups of participants were created: Those who lacked the APOE4 allele and those who did. The majority of participants were able to view information on all other covariates, such as systolic blood pressure, body mass index, baseline cardiovascular disease, stroke, current cigarette smoking, alcohol intake (0, <2 or >2 drinks per day), educational level (dichotomized at high school graduation), and plasma tHcy levels (dichotomized as within or below the top age and sex quartile).
Statistical analysis
The presence or absence of DM at the biennial assessment served as the exposure variable, and we used Cox proportional hazards regression models (age and sex-adjusted, multivariable models) to relate the presence or absence of DM to the development of all-cause dementia, AD, and VaD (until December 2033). VaD and Alzheimer's disease are viewed as conflicting hazards. We further corrected for APOE4 status in participants for whom APOE genotype data were available. By integrating the relevant interaction terms into the analysis, we examined how age, sex, baseline blood pressure, diabetes treatment, a priori risk status, and the accessibility of the APOE4 genotype affected the effect modification. We assessed the chances of having dementia and AD in subgroups of people who were a priori less likely to develop dementia and AD. Diabetes was modeled as a time-dependent covariate for secondary analysis. SAS software was used for all the statistical analyses.
Results
At baseline, of the 2210 trial participants, 202 (9.1%) had diabetes at the beginning of the study, 98 (4.4%) had a confirmed blood glucose level higher than 198 mg/dL (11 mmol/L), and 176 (8%) were using insulin or an oral hypoglycemic medication. Table 1 compares the demographic and baseline characteristics of the participants with and without diabetes. A total of 319 of the 2210 patients developed dementia throughout the course of the 20-year follow-up period (range, 1-20 years; mean, 12.7 years; 237 had definite or probable AD; 32 had probable VaD). In comparison to all the subjects, the Relative Risk (RR) for Alzheimer's Disease (AD) was 0.32 (95% confidence interval, 0.23-0.47; P<.001) for low-risk individuals without the APOE4 gene or a plasma tHcy level in the top quartile and 0.24 (95% confidence interval, 0.15-0.39; P<.001) for very low-risk individuals who were also under 75 years old. Using both conventional and time-dependent Cox models, we discovered that, generally, DM did not increase the risk of AD or all-cause dementia; however, the subgroup of participants who were considered low risk and very low risk according to the standard Cox models did have an increased risk. Throughout the follow-up period, this difference in risk persisted (Figures 1 and 2). Age and a priori risk status were found to be effect modifiers (greater risk in younger patients; P.05); in contrast, APOE genotyping availability, baseline blood pressure, diabetes therapy, and sex were not. We do not have enough data to draw any firm conclusions on the likelihood of developing VaD.
| Characteristics of Study Sample at Baseline (16th Biennial) Examination* | |||
|---|---|---|---|
| Characteristic | Without diabetes (n=2008) | With diabetes (n=202) | P-value |
| Sex, % males | 39 | 51 | 0.002 |
| Age, yr | 70.4 ± 6.9 | 71.5 ± 7.0 | 0.045 |
| Education, high school graduate, % | 64 | 53 | 0.002 |
| Systolic blood pressure, mm Hg | 139 ± 20 | 146 ± 19 | <.001 |
| Body mass index† | 26.5 ± 4.3 | 28.5 ± 5.2 | <.001 |
| Apolipoprotein E genotype, % | |||
| Â2/ε2 or ε2/ε3 | 11 | 9 | 0.88 |
| ε3/ε3 | 67 | 67 | |
| ε2/ε4, ε3/ε4, or ε4/ε4 | 22 | 24 | |
| Plasma homocysteine level, μmol/L | 12.5 ± 7.5 | 12.2 ± 4.3 | 0.42 |
| Casual blood glucose level, mg/dL | 89 ± 19 | 156 ± 89 | <.001 |
| Diabetes medications | |||
| Insulin, % | 0 | 18 | <.001 |
| Oral hypoglycemic, % | 0 | 44 | <.001 |
| Alcohol | |||
| 0 drinks/d | 38 | 52 | |
| <2 drinks/d | 44 | 35 | <.001 |
| >2 drinks/d | 18 | 14 | |
| Current smoker, % | 16 | 15 | 0.7 |
| Baseline cardiovascular disease | |||
| Stroke, % | 3 | 8 | 0.002 |
| Other cardiovascular disease, % | 20 | 39 | <.001 |
Table 1: SI conversion factors-To convert glucose to millimoles per liter, multiply by 0.05551. Note: *: Values are given as the mean ± SD unless otherwise noted, †: Calculated as weight in kilograms divided by the square of height in meters.

Figure 1: Cumulative incidence of Alzheimer disease in entire
sample: comparison of groups with and without Diabetes
Mellitus (DM), adjusted for age and sex. Note: ( ) No DM,
(
) No DM,
( ) DM.
) DM.

Figure 2: Cumulative incidence of Alzheimer disease in lowrisk
group: Comparison of persons with and without Diabetes
Mellitus (DM), adjusted for age and sex. Note: ( ) No DM,
(
) No DM,
( ) DM.
) DM.
Discussion
According to the entire Framingham Study sample, Diabetes Mellitus increased the risk of AD by three to five times in patients who had a relatively lower initial risk of the disease (those who were APOE4 negative and did not have plasma tHcy levels in the highest age and sex-specific quartile). However, Diabetes Mellitus was not an independent risk factor for AD. The population-attributable risk factor for DM was 25% in younger patients (<75 years of age), where the RR was highest. Our results imply that DM may affect AD risk in study population subpopulations in which there is no proof of an overall relationship between these features [5]. The strengths of our investigation include its prospective study design, direct confirmation of exposure and outcome status, and communitybased population. By enrolling the population well in advance of diabetes or dementia development and by closely monitoring survival and cognitive health throughout time, selection bias was reduced. The likelihood of an ascertainment bias was reduced by the continual determination of diabetes status at each biennial examination, beginning long before the development of dementia. Finally, subjects underwent up to one year of observation [6-8]. The study population's predominance of white people is a significant restriction. Additionally, because we used casual (nonfasting) blood glucose levels rather than fasting blood glucose levels, we might have mistakenly classified patients with impaired glucose tolerance as nondiabetic patients. The null hypothesis would benefit from this bias in the overall and subgroup analyses, but it would not explain our observations of higher risk in certain subgroups [9-11]. Our results are consistent with a number of previous and, which neither did not show a link between DM and the risk of developing AD nor did they only occur in certain subgroups (men, people whose systolic blood pressure was less than 180 mm Hg, or people who had the genotype), and These findings are not consistent with the results of a few sizable population-based studies that did establish a general association [12]. The prevalence and definition of Diabetes Mellitus (DM) varied among the studies, which may be one explanation for this discrepancy. We discovered that participants lacking the three established AD risk factors-those with a tHcy level in the top quartile, an APOE4 gene, or age 75 or older-had the highest probability of developing AD, which may be attributed to DM. The risk in this particular category has not been studied previously; however, subjects younger than 75 years of age have been shown to have a higher risk of AD associated with DM than subjects older than 85 years [13-16]. The Kungsholmen project revealed no correlation between the APOE4 genotype and diabetes incidence, despite the findings of the Honolulu-Asia Aging study revealing a greater RR among patients with this genotype. These discrepancies may be the result of chance, racial, or sex disparities in the population or both. Our epidemiological findings may have a biological basis; as prior research has revealed that AD patients lacking the APOE4 gene may be more vulnerable to the harmful consequences of hyperinsulinemia. Numerous biologically conceivable, nonvascular mechanisms could be used to mediate the link between DM and AD. Advanced glycation end products, inflammation, and neurofibrillary tangle development are all encouraged by Diabetes Mellitus [17,18]. The risk of AD appears to be increased by insulin resistance and subsequent hyperinsulinemia. Similar genetic mechanisms may play a role in the development of AD and DM. For example, mutations in the insulin-degrading enzyme that result in DM41 also impact the degradation of amyloid protein [19,20].
Conflicts of Interest
None
References
- Arvanitakis Z, Wilson RS, Bienias JL, Evans DA, Bennett DA. Diabetes Mellitus and risk of Alzheimer disease and decline in cognitive function. Arch Neurol. 2004;61(5):661-666.
[Crossref] [Google Scholar] [PubMed]
- den Heijer T, Vermeer SE, Van Dijk EJ, Prins ND, Koudstaal PJ, Hofman A, et al. Type 2 diabetes and atrophy of medial temporal lobe structures on brain MRI. Diabetologia. 2003;46:1604-1610.
[Google Scholar] [PubMed]
- Elias MF, Elias PK, Sullivan LM, Wolf PA, D Agostino RB. Obesity, diabetes and cognitive deficit: The Framingham Heart Study. Neurobiol Aging. 2005;26(1):11-16.
[Crossref] [Google Scholar] [PubMed]
- Farris W, Mansourian S, Leissring MA, Eckman EA, Bertram L, Eckman CB, et al. Partial loss-of-function mutations in insulin-degrading enzyme that induce diabetes also impair degradation of Beta amyloid-protein. Am J Pathol. 2004;164(4):1425-1434.
[Crossref] [Google Scholar] [PubMed]
- Fishel MA, Watson GS, Montine TJ, Wang Q, Green PS, Kulstad JJ, et al. Hyperinsulinemia provokes synchronous increases in central inflammation and Beta-amyloid in normal adults. Arch Neurol. 2005;62:1539-1544.
[Crossref] [Google Scholar] [PubMed]
- Fontbonne A, Berr C, Ducimetière P, Alpérovitch A. Changes in cognitive abilities over a 4-year period are unfavorably affected in elderly diabetic subjects: Results of the Epidemiology of Vascular Aging Study. Diabetes care. 2001;24(2):366-370.
[Google Scholar] [PubMed]
- Haan MN, Mungas DM, Gonzalez HM, Ortiz TA, Acharya A, Jagust WJ. Prevalence of dementia in older latinos: The influence of type 2 Diabetes Mellitus, stroke and genetic factors. J Am Geriatr Soc. 2003;51(2):169-177.
[Google Scholar] [PubMed]
- Hassing LB, Johansson B, Nilsson SE, Berg S, Pedersen NL, Gatz M, et al. Diabetesmellitusis risk factor for vascular dementia, but not for Alzheimer’s disease: A population-based study of the oldest old. Int Psychogeriatr. 2002;14(3):239-248.
- Ivan CS, Seshadri S, Beiser A, Au R, Kase CS, Kelly-Hayes M. Dementia after stroke: The Framingham Study. Stroke. 2004;35(6):1264-1268.
- Karamohamed S, Demissie S, Volcjak J, Liu C, Heard-Costa N, Liu J, et al. Polymorphisms in the insulin-degrading enzyme-encoding gene are associated with type 2 diabetes in men from the NHLBI Framingham Heart Study. Diabetes. 2003; 52(6):1562-1567.
[Google Scholar] [PubMed]
- Logroscino G, Kang JH, Grodstein F. Prospective study of type 2 diabetes and cognitive decline in women aged 70-81 years. BMJ. 2004;328(7439):548.
[Google Scholar] [PubMed]
- Luchsinger JA, Reitz C, Honig LS, Tang MX, Shea S, Mayeux R, et al. Aggregation of vascular risk factors and risk of incident Alzheimer disease. Neurol. 2005;65(4):545-551.
[Google Scholar] [PubMed]
- Luchsinger JA, Tang MX, Shea S, Mayeux R. Hyperinsulinemia and risk of Alzheimer disease. Neurol. 2004;63(7):1187-1192.
- Luchsinger JA, Tang MX, Stern Y, Shea S, Mayeux R. Diabetes Mellitus and risk of Alzheimer’s disease and dementia with stroke in a multiethnic cohort. Am J Epidemiol. 2001;154(7):635-641.
[Google Scholar] [PubMed]
- MacKnight C, Rockwood K, Awalt E, McDowell I. Diabetes Mellitus and the risk of dementia, Alzheimer’s disease and vascular cognitive impairment in the Canadian Study of Health and Aging. Dement Geriatr Cogn Disord. 2002;14:77-83.
- Peila R, Rodriguez BL, Launer L. Type 2 diabetes, APOE gene, and the risk for dementia and related pathologies: The Honolulu-Asia Aging Study. Diabetes. 2002;51(4):1256-1262.
- Schmidt R, Launer LJ, Nilsson LG, Pajak A, Sans S, Berger K, et al. Magnetic resonance imaging of the brain in diabetes: The Cardiovascular Determinants of Dementia (CASCADE) Study. Diabetes. 2004;53(3):687-692.
[Google Scholar] [PubMed]
- Schnaider Beeri, Goldbourt U, Silverman JM, Noy S. Diabetes Mellitus in midlife and the risk of dementia three decades later. Neurol. 2004;63(10):1902-1907.
- Xu WL, Qiu CX, Wahlin A, Winblad B, Fratiglioni L. Diabetes Mellitus and risk of dementia in the Kungsholmen project: A 6-year follow-up study. Neurol. 2004;63(7):1181-1186.
[Crossref] [Google Scholar] [PubMed]
- Yaffe K, Blackwell T, Kanaya AM, Davidowitz N, Barrett-Connor E, Krueger KD. Diabetes, impaired fasting glucose, and development of cognitive impairment in older women. Neurol. 2004;63(4):658-663.
Citation: Tunio AR, Batool S, Khan MUZ, Smo UBK, Abbas K, Lakho R, et al. (2024) Risk of Alzheimer's Disease in People with Diabetes Mellitus. Bio Med. 15:671.
Copyright: © 2024 Tunio AR, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.