Indexed In
- Open J Gate
- Cosmos IF
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
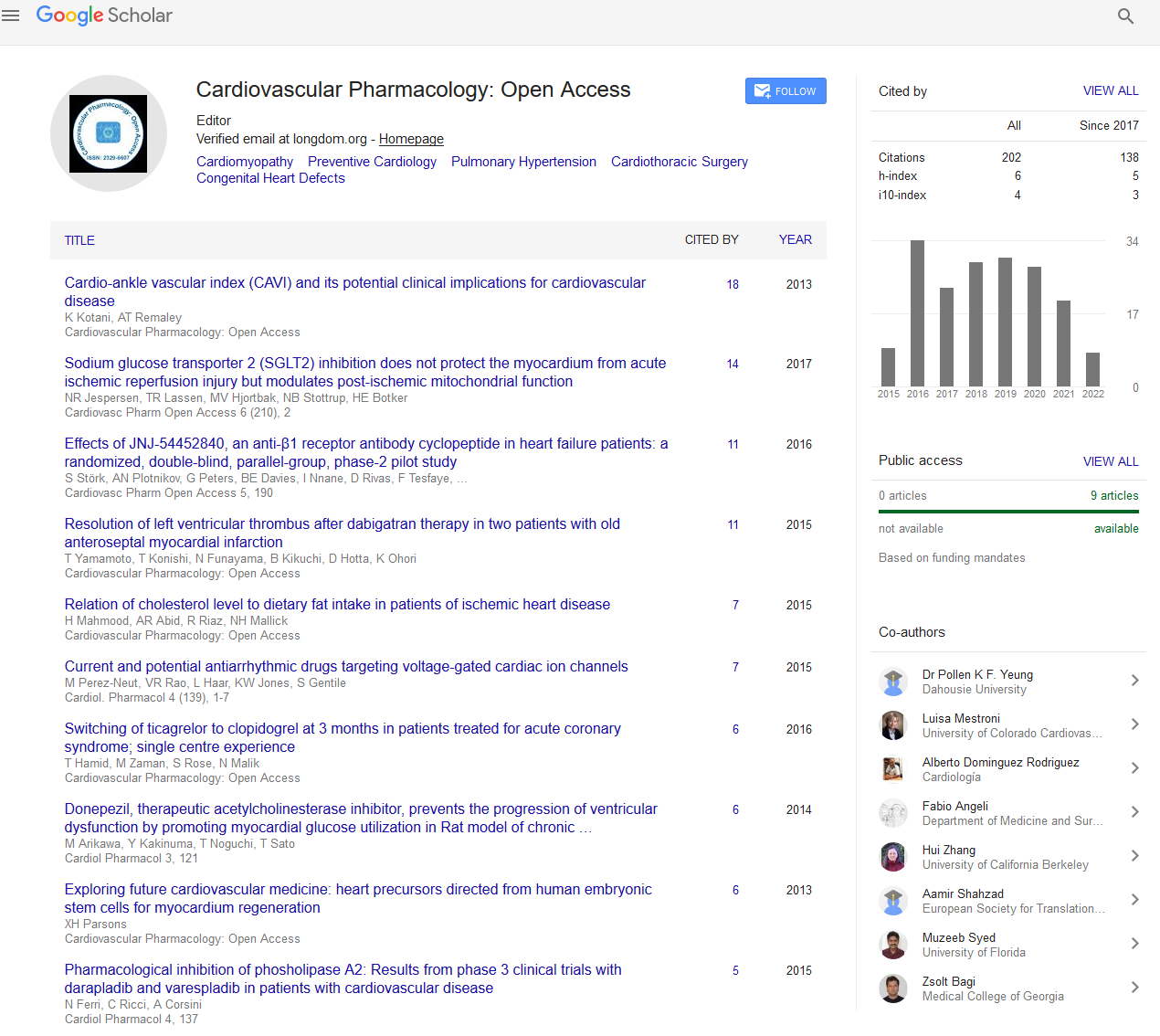
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Opinion Article - (2022) Volume 11, Issue 10
Relevance of Immunity and Inflammation in Cardiovascular Disease and Atherosclerosis
Robert Lazzerini*Received: 03-Oct-2022, Manuscript No. CPO-22-18610; Editor assigned: 06-Oct-2022, Pre QC No. CPO-22-18610 (PQ); Reviewed: 20-Oct-2022, QC No. CPO-22-18610; Revised: 27-Oct-2022, Manuscript No. CPO-22-18610 (R); Published: 03-Nov-2022, DOI: 10.35248/2329-6607.22.11.311
Description
Many cardiovascular disorders originate and worsen as a result of innate and adaptive immune responses. It is generally acknowledged that atherosclerosis, the main factor in coronary artery disease, stroke, and peripheral vascular disease, is a chronic inflammatory disease. The pathogenesis of atrial fibrillation, the most prevalent heart arrhythmia, also includes inflammation. Alterations in immunological responses can result in cardiac remodelling following myocardial infarction, and defects in the resolution of inflammation encourage the development of susceptible plaque in atherosclerosis. The immune system has a variety of roles in the development of Atherosclerotic Cardiovascular Disease (ASCVD). However, little is known about the dysregulation of immune cells that causes ASCVD. We examined whether arterial calcifications contribute to the link between innate and adaptive immune system components and ASCVD across time.
Heart disease and vasculopathies are only two examples of the pathologies where innate immunity and inflammation play important roles. Current theories contend that "damage" rather than "foreignness" is what actually sets off the immune system, which has drastically altered how we often think about the etiopathology of the majority of cardiac diseases. It is exciting to consider the possible role that some anti-inflammatory medicinal approaches may have in the treatment of cardiac disease. The Janus face of immunity and inflammation cannot be overstated, though, since improper manipulation of these systems might be harmful or at the very least ineffective. Undoubtedly, knowing the functional properties of certain immune mediators is a key topic, but the key to selecting prospective drug targets for the future lies in a thorough comprehension of the many biological activities of these molecules as well as their context-specific roles.
Toll-Like Receptors (TLRs) are traditional Pattern Recognition Receptors (PRRs), gene-encoded proteins that the innate immune system uses to identify mostly invariant pathogen associated molecular patterns (PAMPs) that are shared by pathogen groups but at the same time not present in the host. Lipopolysaccharides produced by bacteria and double-stranded RNA produced by various viruses are two examples of PAMPs. An extracellular leucine-rich repeat domain and a cytoplasmic toll/interleukin-1 receptor homology domain are features of TLRs. The TLR family of transmembrane proteins now consists of thirteen different members, each of which has a number of distinct ligands that, upon binding, cause the proper hostdefense genes to be activated and transcripted. TLRs are expressed by nearly all cardiac cells. Cardiomyocytes can easily identify TLR-2 to TLR-4 and TLR-6, but the endotheliocytes, smooth muscle cells, and macrophages of the vasculature can only detect TLR-1 to TLR-6. TLRs can trigger a full immune response that includes both innate immune activity through activated macrophages that can fight invading pathogens by producing pro-inflammatory cytokines and antimicrobial molecules (such as nitric oxide) as well as an adaptive immune response by activating dendritic cells, which can promote T-cell expansion and differentiation. TLRs can also keep this adaptive immune response going by supplying the required co-stimulatory chemicals. A cell- and pathogen-specific immune response can be triggered by the TLR family. Immune and parenchymal cells express TLR system components differently, and many TLRs are triggered by more than one class of PAMPs.
The pathophysiology of some of the most prevalent cardiovascular disorders is characterised by inflammation. Recent advances in genetically altered rodent models, such as transgenic and knockout mice, have made it possible to identify certain signalling pathways causing heart disease and assess potential clinical treatment possibilities. Understanding tissuespecific mechanisms that may either enhance or reduce inflammatory cells and mediators is crucial for developing therapeutic methods for inflammatory processes in any organ. It is crucial to understand that the inflammatory response will likely vary depending on the organ in question in terms of its amplification and/or dampening, and that the matrix and mediators released by specialised cells will regulate the overall inflammatory response in addition to the organ's primary cellular makeup. Due to the fact that conventional cardiovascular medications appear to have little to no effect on the total cytokine network, Immunomodulatory therapy has become a potential new therapeutic option for CHF (Cardiac Heart Failure). Future research will probably focus on selective gene targeting to determine which PRRs play a crucial function in the heart consequent to damage.
Citation: Lazzerini R (2022) Relevance of Immunity and Inflammation in Cardiovascular Disease and Atherosclerosis. Cardiovasc Pharm. 11:311
Copyright: © 2022 Lazzerini R. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.