PMC/PubMed Indexed Articles
Indexed In
- Academic Journals Database
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Ulrich's Periodicals Directory
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2019) Volume 10, Issue 1
Recurrent Cutaneous Bullous Lesions: Think of Fixed Drug Eruption!
Salma Salim1*, Mariame Meziane1, Nadia Ismaili1, Laila Benzekri1, Karima Senouci1, Kaoutar Znati2, Amina Tebaa3 and Badredine Hassam12Department of Histopathology, Ibn Sina University Hospital, Rabat, Morocco
3Poison Control and Pharmacovigilance Center of Morocco, Rabat, Morocco
Received: 29-Jan-2019 Published: 26-Feb-2019
Abstract
Fixed drug eruption is the only pathognomonic clinical form of cutaneous drug reaction. It is an eruption made of one or few centimetric lesions, relapsing in the same area and leaving residual pigmentation. The bullous forms of fixed pigmented erythema are rare but can be serious in case of generalized forms. The management of this situation is based on the immediate interruption of the suspected drug, the notification to pharmacovigilance, and the hospitalization in case of extended forms with symptomatic treatment. The prevention consists in the identification and total eviction of the responsible drug. We report a rare and original case of bullous fixed drug eruption in an adult, and we discuss its diagnosis, management and prognosis.
Keywords
Bullous fixed drug eruption; Lyell-like eruption; Notification to pharmacovigilance; Eviction of responsible drug
Introduction
Fixed Drug Eruption (FDE) is a cutaneous drug reaction made of one or few centimetric lesions, relapsing in the same area and leaving residual pigmentation [1]. Bullous Forms (BFDE) are rare but can be serious in case of generalized forms
Case Report
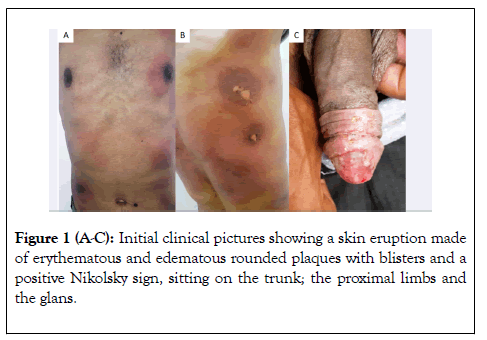
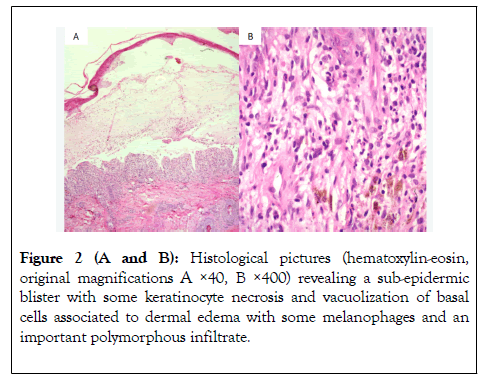
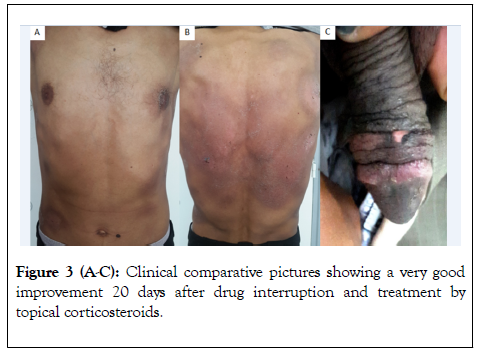
We report a case of a 50-year-old man without significant past medical history. He consulted in the emergency department for a skin eruption that occurred 12 hours after taking a Trimethoprim-Sulfamethoxazol (TS) tablet of 400 mg for an episode of diarrhea. The patient reported similar eruption two years ago after a drug intake too. Dermatological examination revealed a bullous eruption sitting on an erythematous base in the trunk, the proximal limbs and the glans. Nikolsky sign was positive and the peeled surface area was estimated at 7% (Figures 1A-1C). BFDE was strongly suspected and drug intake stopped. Declaration to Poison Control and Pharmacovigilance Centre was made and incriminated the TS. Cutaneous biopsy was made and objectived a sub-epidermal blister with some keratinocyte necrosis and vacuolization of basal cells, associated to dermal edema with some melanophages and an important polymorphous infiltrate (Figures 2A and 2B). A treatment based on topical corticosteroids and antihistamine drugs was instituted with good clinical improvement(Figures 3A-3C). A certificate indicating the responsibility of TS has been given to the patient prohibiting any further taking of the latter and all similar drugs of the same family.
Figure 1(A-C): Initial clinical pictures showing a skin eruption made of erythematous and edematous rounded plaques with blisters and a positive Nikolsky sign, sitting on the trunk; the proximal limbs and the glans.
Figure 2 (A and B): Histological pictures (hematoxylin-eosin, original magnifications A ×40, B ×400) revealing a sub-epidermic blister with some keratinocyte necrosis and vacuolization of basal cells associated to dermal edema with some melanophages and an important polymorphous infiltrate.
Figure 3 (A-C): Clinical comparative pictures showing a very good improvement 20 days after drug interruption and treatment by topical corticosteroids.
Discussion
FDE is a recurrent eruption leaving residual pigmentation. It is the only pathognomonic clinical form of cutaneous drug reaction [1]. This is a model of delayed hypersensitivity to drug reaction mediated by CD8 T cells [2,3]. The prevalence of the FDE varies considerably from one country to another, from less than 1% of drug reactions in Switzerland to 70% in West Africa [1,4]. The onset is rapid made of itch and localized burns followed by the appearance of one or few erythematous or brown and edematous plaques, rounded or oval, centimetric, occurring 1 to 4 days after the first dose, and few hours after readministration.
The improvement is good in few days with residual pigmentation [1]. Bullous forms are rare and can be localized or generalized as pseudo-Lyell type. Histological examination shows vacuolization of basal cells, sometimes with keratinocyte necrosis, sub-epidermic blister, dermal edema and perivascular lympho-histiocytic infiltrate. Patch tests could be especially interesting if several drugs are suspected. However, they are not necessary to make the diagnosis and their sensibility is not very important and varies from one series to another [3,5]. Declaration of pharmacovigilance is mandatory. The most implicated drugs are phenazone, barbiturates, carbamazepine, non-steroidal anti-inflammatory drugs, cyclins and sulfonamides, as in our patient [1,4]. Differential diagnosis between BFDE and Stevens-Johnson syndrome or Lyell syndrome could be made according to chronological, clinical and histological criteria in addition to bibliographic data provided by pharmacovigilance centre [1,6]. There is no specific treatment of the disease and the management remains symptomatic. The use of topical and sometimes systemic corticosteroids may reduce the inflammation. In case of generalized BFDE, severity is related to the importance of the peeled or peelable surface. When it is greater than 10%, the patient should be hospitalized and symptomatic treatment established joining that of Lyell syndrome [1,7]. Prevention is based on the identification and definitive eviction of the responsible drug and all similar drugs of the same family. The prognosis is close to that of Lyell syndrome with an equal affected cutaneous surface [7].
Conclusion
FDE is most often a benign type of cutaneous drug reaction. Bullous forms are rare but could be severe in case of generalized form.
REFERENCES
- Valeyrie-Allanore L, Lebrun-Vignes B, Bensaid B, Sassolas B, Barbaub A, sous l’égide du groupe toxidermie de la Société française de dermatologie (FISARD). Fixed pigmented erythema: Epidemiology, physiopathology, clinical features, differential diagnosis and therapeutic management. Ann Dermatol Venereol. 2015;142(11): 701-706.
- Mizukawa Y, Shiohara T. Fixed drug eruption: a prototypic disorder mediated by effector memory T cells. Curr Allergy Asthma Rep. 2009;9(1): 71-77.
- Shiohara T. Fixed drug eruption: pathogenesis and diagnostic tests. Curr Opin Allergy Clin Immunol. 2009;9(4): 316-321.
- Lebrun-Vignes B, Jean-Pastor MJ. Étude des 307 cas d’érythème pigmenté fixe enregistrés dans la base nationale de pharmacovigilance. Ann Dermatol Venereol. 2008;135: A97-A98.
- Andrade P, Brinca A, Goncalo M. Patch testing in fixed drug eruptions--a 20-year review. Contact Dermatitis. 2011;65(4): 195-201.
- Zaouk A, Chaabani M, Ben Salem F, Ben Jannet S, Hammami H, Kastalli S. Erythème pigmenté fixe bulleux: une série hospitalière. Revue française d’allergologie. 2018;58(3): 240-249.
- Lipowicz S, Sekula P, Ingen-Housz-Oro S, Liss Y, Sassolas B, Dunant A, et al. Prognosis of generalized bullous fixed drug eruption: comparison with Stevens-Johnson syndrome and toxic epidermal necrolysis. Br J Dermatol. 2013;168(4): 726-732.
Citation: Salim S, Meziane M, Ismaili N, Benzekri L, Senouci K, Znati K, et al. (2019) Recurrent Cutaneous Bullous Lesions: Think of Fixed Drug Eruption! J Allergy Ther 10:1
Copyright: © 2019 Salim S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.