Indexed In
- Open J Gate
- Genamics JournalSeek
- CiteFactor
- Cosmos IF
- Scimago
- Ulrich's Periodicals Directory
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- Directory of Abstract Indexing for Journals
- OCLC- WorldCat
- Proquest Summons
- Scholarsteer
- ROAD
- Virtual Library of Biology (vifabio)
- Publons
- Geneva Foundation for Medical Education and Research
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research - (2021) Volume 13, Issue 11
Recurrence of Tuberculosis and Associated factors Among Treated Patients
Meskerem Abebe*Received: 04-Nov-2021 Published: 25-Nov-2021, DOI: 10.35248/0974-8369.21.13.455
Abstract
Introduction: Tuberculosis is the disease with the second highest incidence rate and causes the highest mortality rate among communicable diseases in Ethiopia. Recurrent disease is an essential issue in survival analysis: where the same event is observed on the same subject (patient) more than once. Recurrence of TB is still a major problem in high burden countries, where there is lack of resources and no special attention is being given to this issue. The rate of recurrence is highly variable and has been estimated to range from 4.9% to 47%.
Methods: The data for this study was extracted from 338 Tuberculosis patients’ during monthly follow-up period (2010-2016). Descriptive statistics such as frequency table was used to summarize the data. Log-Normal frailty model were used in determining the risk factors associated with time to recurrence of Tuberculosis disease.
Results: Recurrence of tuberculosis was highest (21.3%) among patients in the age group 26-40 years. Out of 338 subjects, 62.2% of tuberculosis human immune deficiency virus Positive and 78.4% of the patients were alcohol drinker. The results of shared log-normal frailty indicate that initial body weight (P ≤ 0.05, CI = (1.02, 1.05), past medical history (P ≤ 0.05, CI (1.60-4.44), TB category (P ≤ 0.05, CI:(1.36 - 3.76), residence(P ≤ 0.05, CI: (1.37-2.90), HIV status (P ≤ 0.05, CI: (0.48-0.96), alcohol use (P ≤ 0.05, CI: (0.32-0.76), localization of TB (P ≤ 0.05, CI: (0.44- 1.01) were the most prognostic factors for the recurrence of tuberculosis.
Conclusion: The author concludes that Patients with risky behaviours, such as alcohol consumption and risky clinical factors, such as positive HIV status or previous family history, have a higher recurrence. Therefore, considerable attention should be given to those significant explanatory variables in order to reduce recurrence of Tuberculosis.
Keywords
Recurrent event; Tuberculosis; Shared lognormal frailty model; Ethiopia
Abbreviations
DOTS = Directly Observed Treatment, Short-course
FMOH = Federal Ministry of Health
HIV = Human Immunodeficiency Virus
IP = Intensive Phase LOWESS = Locally Weighted Polynomial Regression
MDR = Multi-Drug Resistant
NTLCP = National Tuberculosis and Leprosy Control Program
TB=Tuberculosis
WHO=World Health Organization,
AFB=Acid Fast Bacilli
AIC=Akaikie in formation criterion,
AG=Andersen-Gill
PWP=Prentic-Williams-Peterson
REH=Rifampicin Ethambutol Hisoniazid
EH=Ethambutol Hisoniazid
RH=Rifampicin Hisoniazid
CPT=Co-trimoxazole Preventive Therapy
HSDP=Health Sector Development Program
NTLCP=National Tuberculosis Leprosy Control Program
LCV= Likelihood Cross-Validation.
Introduction
Tuberculosis is an infectious disease caused by Mycobacterium tuberculosis. Tuberculosis is a contagious airborne disease that commonly attacks the lungs; but it affects any part of the body, from the bloodstream to the brain. The disease has become rare in high-income countries, but still a major public health problem in low-and middle-income countries. Tuberculosis causes ill-health in millions of people each year, and in 2015 was one of the top 10 causes of death worldwide, ranking above HIV/AIDS as one of the leading causes of death from an infectious disease. This is despite the fact that with a timely diagnosis and correct treatment, most people who develop TB can be cured [1].
TB can affect any tissue or organ but most commonly it affects the lungs. As a result, TB has diverse clinical manifestations. Transmission is broadly classified into pulmonary TB (85% of the cases) and extra-pulmonary tuberculosis that accounts for the remaining 15%. Pulmonary tuberculosis is classified into smearpositive pulmonary tuberculosis that accounts for 75-80% of all pulmonary tuberculosis and smear-negative pulmonary tuberculosis that accounts for about 20-25% of all pulmonary tuberculosis cases. Detection of the bacterium by a direct microscope from sputum has been the main way for the diagnosis of tuberculosis. However, smear-positive synonyms (ordered by estimated frequency) of noun rate among HIV-positive tuberculosis affected roles have markedly decreased and thus the most expensive and time taking gene expert technique is used for the diagnosis of tuberculosis [2]. Recurrence of TB is still a major problem in high burden countries, where there is lack of resources and no special attention is being given to this issue. The rate of recurrence is highly variable and has been estimated to range from 4.9% to 47%
In 2010, recurrence TB contributes 3.1% of the total notification TB cases. From 1995 up to 2010, a TB-infected patient in Ethiopia has increased from 343 to 4,898 cases. In this interval the estimated proportion of new and recurrence cases that have MDR-TB were 1.6% and 12% respectively [3]. Surveillance data suggest that the recurrence regime is successful in about 70% of the patients but the retrospective study that has evaluated the regimen’s efficacy showed variable discussion responses with success rates ranging from 26% to 92%. Rapid diagnosis of mycobacterium infections is essential to provide appropriate antimicrobial therapy and in the case of Mycobacterium tuberculosis, to implement effective infection control or hospital interference. Tuberculosis was the disease with the second highest incidence rate and caused the highest mortality rate among communicable diseases in Ethiopia [4-10]. Therefore, the study was conducted on recurrence of TB patients and to identify related factors.
Methods
Study area description
The investigation was conducted in Robe Hospital, Bale Zone, Oromia Region, Ethiopia. According to the 2015 census, the population is 49,398. Data from this study were extracted from a total of 338 TB patients. Each patient was identified by a unique medical registration card code, and the information needed for our study was extracted from follow-up history at Robe Hospital. All patients diagnosed with tuberculosis at Bale Robe Hospital were administered DOT in accordance with the guidelines of the national tuberculosis and leprosy management program (NTLCP).
Data Collection Method
Data collection procedure
In this study, the authors used secondary data from the TB registration book of the hospital. The book contained basic information such as patient’s age, sex, residence, weight, category of TB, HIV status, educational level, alcohol used, smoking habits, localization of TB, family history of TB, past medical history, history of previous treatment, marital status, treatment started date, treatment stopped date and treatment outcome.
Data extraction was conducted by nurse’s workings at the TB clinic of the hospital. One day grooming was given for all data collectors about how to fill the structured data collecting sheet. The hospital’s register was used to retrieve data on tuberculosis disease and patient's initial date of entry to follow-up. During the sample distribution process, the hospital’s record logbook also was used in parliamentary procedure to select the patients. Data ingathering was carried out during November 15, 2017 to March 28, 2017.
Data Structure for Modeling Recurrence of TB Disease
The sample carefully checked the data of three tuberculosis patients and confirmed the time to recurrence of the first, second, and second times in tuberculosis patients. The duration of each subject in the study was defined as the time from enrolment to the end of the study or the time until subject supplementation was lost or withdrawn. No tuberculosis recurrence must be before or after the tuberculosis-free period, except at the end of the study period in case of deviation.
Subjects with multiple events are counted as multiple entities for analysis purposes. For example, subjects 3, 3 times were considered. The first row starts the follow-up at time 0 and ends at 9 months. According to the fact that the subject has been at risk for 9 months. The second line shows the patient's risk of another event of interest resumed at 26 months after the previous event postponed entry at 35 months and ended at 42 months.
The third line shows that the risk that the previous event of interest was postpone into the 70th month and ended in the 76th month restarted in the 28th month after the same analysis in themes one and two. Shows the data structure representation of the time to relapse model by the follow-up history and calendar time scale for three patients.
Data Analysis
The collected data input to Excel and analysed with Statistical software R version 3.5. In this study, an extension of the original Cox model provided for analysis of recurrence event data, and the researchers make the following assumptions: In the case of data that cut off in the middle of the right. The lognormal frailty model at the 5% significance level determines the relationship and intensity between the explanatory and outcome variables.
Shared Lognormal Frailty Model
The popularity of the log-regular flail model stems primarily from its link with the hybrid model. The standard assumption here is that the random effect is normally distributed. The use of lognormal distributions in the flail model stems from the link with generalized mixed models with the standard assumption that the random effect wj follows a normal distribution with mean zero variance σ2. The corresponding log-normative flail model given by the equation:
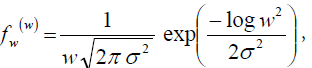
Where: E(w) = exp (α2 / 2)
var (w)= exp (σ2 ) (exp (σ )−1)
Therefore, this model indicates that σ2 represents the variance of the random effect w = ln(Z). Also, the expectation of the Frailty variable is usually no 1, even though the lognormal model random effect w has an expectation of zero.
Results
Descriptive statistics results Descriptive statistics presented, out of 338 patients, 56.8% experienced recurrence and the remaining 43.2% discontinued. In this study, recurrence of tuberculosis started at 0, and the maximum was 3 times. The results show that the rate of recurrence is greater in male patients, 23.7% and 19.5% than that in females. Of all subjects included in this study, 62.2% found to be HIVpositive, while 37.8% of patients with tuberculosis were negative. The highest 30.5% of recurrence was 12.7% in HIV-positive tuberculosis patients than in HIV-negative tuberculosis patients. Based on the total subjects incorporated into this study, 78.4% of patients were drinkers, whereas 21.6% were non-drinkers. The recurrence of the disease was higher among drinkers and 36.4% than those who did not drink (6.8%). The sample data also made it clear that 84.9% were smokers and 15.1% were non-smokers. The recurrence in non-smokers was 7.4%, less than in smokers 35.8%.
Analysis of Log-Normal Frailty Model
A Semi parametric random effect frailty model suitable to adequately explain the dependency between un observed heterogeneity with the patient. In this model, we assumed that the time to recurrence of TB follows the Cox proportional hazards model with the condition of some unobserved senility random variables. Multiple recurrences in each individual share a common senility random variable to explain within their individual correlations.
Shared Lognormal Frailty Model Results
Performs univariate analysis based on the shared log-normal Frailty Model. Except covariate gender, all confirmed as factors, noting that they affected the time to relapse of tuberculosis at a 0.25% significance level. In addition, all covariates were included in multiple covariate analyses to display the effects of Tb relapse factors collectively. The results obtained in Table 1 show that the variance of the senile term sigma is significantly different from 0, which means that there is heterogeneity between subjects described as unobserved covariates.
| Variable name | Category | Coef | Exp(Coef) | SECoef(HIH) | Z-value | P-value | 95% CI |
|---|---|---|---|---|---|---|---|
| Past medical history | Yes | 0.98 | 2.67 | 0.26 | 3.78 | p ≤ 0.05 | 1.60-4.44 |
| Weight | 0.04 | 1.04 | 0.01 | 4.32 | p ≤ 0.05 | 1.02-1.06 | |
| TB category | II | 0.82 | 2.27 | 0.26 | 3.16 | p ≤ 0.05 | 1.36-3.76 |
| Residence | Rural | 0.689 | 1.99 | 0.19 | 3.58 | p ≤ 0.05 | 1.37-2.90 |
| HIV status | Positive | -0.39 | 0.68 | 0.18 | -2.20 | p ≤ 0.05 | 0.48-0.96 |
| Alcohol used | Drinker | -0.709 | 0.49 | 0.22 | -3.16 | p ≤ 0.05 | 0.32-0.76 |
| Localization of TB | Pulmonary | -0.43 | 1.54 | 0.22 | 2.01 | p ≤ 0.05 | 0.44-1.01 |
| Frailty parameter, sigma square= 0.1172 | SE(HIH) = 0.016, P-value = p ≤ 0.05 | ||||||
Penalized marginal log-likelihood=-871.231 Convergence Criteria: Parameters 7.31e-06 likelihood = 0.00 gradient = 5.21e-08 LCV= The approximate likelihood cross-validation criterion in the semi parametrical case 1.52044
Table 1: Multiple Covariate Analysis of Shared Log-Normal Frailty Model.
This can be estimated using the modified Wald test = Wm(σ) = 0.117174 / 0.015844 = 7.4 > 1.64. This is significant for the usual one-sided test threshold. The modified Wald test (Wm) is a test of the significance of the variance of the distribution of variable effects occurring at the boundaries of the parameter space. For zero variance (σ = 0), it indicates that the weak component does not contribute to the model. Frailty item, the test hypothesis of the variance term is given by H0: σ2 = 0 or H0: θ = 0 versus H1: σ2> 0 or H1: θ > 0. Since the vulnerability entry was significant, the same patient can be estimated as = 0.1. The initial body weight of patients with tuberculosis was 1.041, controlled for all other covariates (including weakness), and was statistically significant (P ≤ 0.05, CI = (1.02, 1.05). The recurrence in patients with unit (1 kg) tuberculosis increased by 4%. Controlling other covariates, the risk of past TB history with the same level of aging and the risk of recurrence in patients with a history of TB was 2.670-fold higher than in patients without a history of TB. When rural and urban areas are compared to the same level of frailty and adjusted for other covariates, the risk of rural areas is 1.992 times that of urban areas (P ≤ 0.05, CI (1.37, 2.90) statistically significant. This indicates that the recurrence of the disease in rural patients increased 0.992 times compared to urban areas.
Concordance Probability for recurrence of TB
A commonly used measure of strength in the proportional hazard model is its discriminating power. This is an indicator used to describe high-risk and low-risk patients. In this study, the authors met the corresponding probability of concordance, which is used to separately calculate the discriminating power and predictive accuracy of the lognormal vulnerability model tuberculosis patient data. These probabilities are evaluated like the probabilities of the parameters of the regression model, so only the distribution of the factors is not asymptotically biased. As shown in Table 2, the discriminating power of the log-normal flail model was provided. Based on the results of the concordance probabilities of the shared logarithmic normal flail model, the estimated and true probabilities of survival were consistent with a probability of 0.865 if two respondents experienced the first recurrence with equal probabilities. This means that the lognormal senility model has a high discriminatory power at the first recurrence.
| Relapse time | Shared Log normal frailty |
|---|---|
| 1st relapse | 0.865 |
| 2nd relapse | 0.773 |
| 3rd relapse | 0.790 |
Table 2: Concordance Probability for Recurrence of TB.
According to the results of the shared lognormal frailty model shown in Table 3, the initial weight, category of TB, localization of tuberculosis, HIV status, alcohol use, past medical history, and place of residence were identified as important risk factors for time to recurrence in tuberculosis patients. The findings of this model (including frailty section w) show that for every 1 kg increase in the initial body weight of tuberculosis patients, an increase of 0.044 kg. The risk ratio for category II tuberculosis is 2.265 times that of category I, meaning a recurrence rate. The rate of tuberculosis increased by 2.265 over that of category I. The remaining risk and confidence intervals have similar interpretations.
| Shared Log Normal frailty | ||
|---|---|---|
| Covariates | Hazard ratio | 95% CI |
| Initial weight | 1.044 | 1.021 - 1.064 |
| Category of TB | 2.265 | 1.363 – 3.372 |
| Localization of TB | 1.542 | 0.440 – 1.100 |
| HIV Status | 0.676 | 0.480 - 0.961 |
| Alcohol use | 0.492 | 0.320 – 0.761 |
| Past medical history | 2.670 | 1.600 – 4.441 |
| Residence | 1.992 | 1.372 -2.901 |
Table 3: Hazard ratio with 95% CI for shared log normal models.
Discussion
The purpose of the study was to know the factors associated with time to recurrence in TB patients, based on data collected from Bale Robe Hospital. In this study, the method considered to analyze the recurrence rate of tuberculosis patients is the Shared Log Normal frailty model. The results of this model show larger parameter estimates and standard error.
That is, the standard error for Shared Log Normal was 0.016. Also, a test of the significance of frailty terms shows that there are unobserved variations between patients. Repeated incidents from the same patient share a common weakness. The estimated intra-cluster correlation between patient observations is 0.1 for a shared log normal frailty model. This model is the optimal model for tuberculosis and data recurrence rates. This study provides information about the outcome of treatment for tuberculosis recurrence in Addis Ababa in relation to HIV status, and also provides specific associations between several predictors as a result of treatment for tuberculosis recurrence.
In a study conducted in South Africa to evaluate the explanation for the recurrence of pulmonary tuberculosis, a risk factor for failed treatment outcomes was unemployed patients aged 46 years or older who neglected treatment. Recurrence has been reported in the literature, and the main factors for incomplete treatment are drug resistance and lowering of drug-dose adherence. The study was higher in the recurrent tuberculosis category (42.6%). This result is lower than the study carried out in Addis Ababa Ethiopia (46.1%) and in Southern Ethiopia (50%). This high ratio may be due to a higher frequency of drug resistance tuberculosis. In Ethiopia, in Ethiopia, 12% of the redemption cases and most of the disease of renewed infection from rural areas have appreciated, the TB treatment is at least at least Six months, and it is difficult to visit this treatment for these patients as this incomplete treatment appears.
Conclusion
The main goal of this study was to determine the recurrence of TB disease and associated significant risk factors in Robe general hospital from September, 2010 to September, 2016. The study suggests, at a 5% level of significance, that recurrence of the disease is highly affected by alcohol consumption, HIV status, previous history of tuberculosis, type of tuberculosis, place of residence, and location of tuberculosis based on the results of shared log-normal frailty models. Patients with risky behaviours, such as drinking, as well as risky clinical factors, such as positive HIV status or previous family history, have a higher recurrence.
• Consent for publication
Not applicable in manuscript
• Availability of data and material
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
• Competing interests
The authors declare that they have no any competing interests
• Funding
The author received no financial support for publication of this article.
Authors’ contributions
MA developed the strategy for the review, screened titles and abstracts, conducted quality assessment, supported data extraction,contributed to writing of the manuscript, undertook data extraction and conducted quality assessment. All things can be done by this author.
Acknowledgments
First I would like to acknowledge Dr Ayele Taye, Alemayehu Legesse and Dr Denkewu Bito, for their immense and in valuable advice and guidance that contributed to the successful realization of this study. I want to thanks Bale Robe Hospital for allowing me to use the data used in this study and assisting me during data collection.
REFERENCES
- Ethiopia Federal Ministry of Health. Guidelines for clinical and programmatic management of TB. FMOH Addis Ababa. 2014.
- Keseteberhan A. Ethiopia Federal Ministry of Health. Guidelines for clinical and programmatic management of TB, and leprosy and TB/HIV in Ethiopia. Fifth edition. FMOH Addis Ababa. 2012.
- Prentice R. L, Williams B. J, Peterson A. V. On the regression analysis of multivariate failure time data. Biometrika. 1981; 68(2):373-379.
- Nathanson E, Nunn P, Uplekar M. MDR tuberculosis--critical steps for prevention and control. N Engl J Med. 2010; 9(9):363(11):1050-8.
- Helen A, Monde M. Isoniazid to prevent first and recurrent episodes of TB. Trop Doct. 2006; 36(2):83-6.
- Mlotshwa M, Abraham N, Beery M. Risk factors for tuberculosis smear non-conversion in Eden district, Western Cape, South Africa, 2007–2013: a retrospective cohort study. BMC Infect Dis. 2016; 16(1):365.
- Christoph L, Anna M. M, Barbara K, Claudia M. D, Martina S. Clinical Application of Interferon-γ Release Assays for the Prevention of Tuberculosis in Countries with Low Incidence. Pathog Immun. 2016; 1(2):308-329.
- Jones Lopez E C, AyakakaI L J. Effectiveness of the standard WHO recommended retreatment regimen (category II) for tuberculosis in Kampala, Uganda: a prospective cohort study. PLoS Med. 2011; 8(3):e1000427
- Kuldeep S, Srinath S, Dewan PK, Nari SA. Source of previous treatment for re-treatment TB cases registered under the National TB control Programme, India, 2010. PLoS One. 2011; 6(7):e22061
- M Li, DJ Cha, Y Lai, Villaruz AE. The antimicrobial peptide-sensing system aps of Staphylococcus aureus. Mol Microbiol. 2007 Dec;66(5):1136-47
Citation: Abebe M (2021) Recurrence of Tuberculosis and Associated factors Among Treated Patients. Bio Med 13: 455. doi: 10.35248/0974- 8369.21.13.455
Copyright: © 2021 Abebe M. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


