Indexed In
- Open J Gate
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Geneva Foundation for Medical Education and Research
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2024) Volume 12, Issue 2
Reactance Inversion in Pediatric Respiratory Diseases
Alberto Vidal*Received: 28-Mar-2024, Manuscript No. HCCR-24-25298; Editor assigned: 01-Apr-2024, Pre QC No. HCCR-24-25298 (PQ); Reviewed: 15-Apr-2024, QC No. HCCR-24-25298; Revised: 22-Apr-2024, Manuscript No. HCCR-24-25298 (R); Published: 29-Apr-2024, DOI: 10.35248/2375-4273.24.12.399
Abstract
Impulse Oscillometry measures the impedance of the respiratory system, which is composed of resistance and reactance. Reactance, resonance frequency, and reactance area are oscillometry parameters related to each other and can be altered in obstructive or restrictive respiratory diseases. Recently, the phenomenon of reactance inversion has been described, which corresponds to a distortion of the reactance curve at low frequencies in impulse oscillometry. This pathophysiological phenomenon has been found in cystic fibrosis, prematurity with or without bronchopulmonary dysplasia, low birth weight, and bronchial asthma. Reactance inversion has been related to decreased lung function on spirometry, increased intrarespiratory differences, and/or small airway dysfunction on impulse oscillometry.
Keywords
Reactance inversion; Asthma; Cystic fibrosis; Prematurity; Lung function
Introduction
Impulse Oscillometry (IOS) is a lung function test that has experienced great development in respiratory diseases since it was marketed 30 years ago [1]. Currently, it has proven to be a useful test in the diagnosis and monitoring of diseases such as bronchial asthma, cystic fibrosis, bronchiolitis obliterans, prematurity with or without bronchopulmonary dysplasia, neuromuscular disease, obstructive sleep apnea and vocal cord dysfunction [2,3]. IOS measures Lung Impedance (Zrs) which evaluates the relationship between pressure and oscillatory flow changes in and out of the lungs and is composed of Lung Resistance (Rrs) and Lung Reactance (Xrs). The Xrs is composed of inertance and elastance. The inertance results from the movement of the air column in the conduction airways and represents the positive component of the Xrs. The elastance represents the elastic recoil properties of lung tissue in response to distension, also called stored or rebound energy, and corresponds to the negative component of the Xrs [4]. Elastance derived from low-frequency reactance has been shown to be a consistent measure of small airway constriction and heterogeneity compared to the frequency dependence of resistance. Therefore, the low-frequency reactance and associated elastance may be a more clinically useful measure of small airway disease [5]. On the other hand, in chronic diseases such as bronchial asthma, elastance at low frequencies has been identified as a good parameter to reflect the obstruction of the peripheral airway and its recruitment after the administration of bronchodilators [6]. When the inertance and elastance forces of the respiratory system are balanced or equated, the Xrs will be equal to zero, a point known as Resonant Frequency (Fres). On the other hand, the reactance area (AX), or Goldman's triangle, is the area between the horizontal axis below 0 and the Xrs curve whose most angled vertex is Fres. Therefore, a lower Xrs and/or a higher Fres will cause increases in the AX value [7]. The decrease in Xrs, or the increase in the Fres or AX, may reflect in IOS the degree of compromise of lung function due to obstructive or restrictive pediatric respiratory diseases [8]. Figure 1 shows the normal reactance curve and its relationship with Fres and AX. On some occasions at low frequencies (for example, at 5 or 10 Hertz), a distortion of the Xrs curve occurs, which inverts upwards, mistakenly delivering “less negative” values, which will result in a falsely lower AX calculation. This pathophysiological phenomenon is called Reactance Inversion (RI). This distortion can be automatically corrected with software incorporated into last generation Oscillometers that delivers a new value called corrected reactance (Xrsc). Figure 2 shows curves of Xrs (inverted and corrected), and their respective differences in the value of AX.
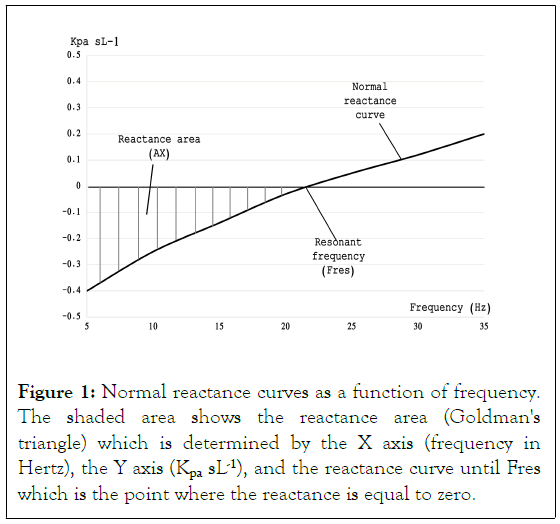
Figure 1: Normal reactance curves as a function of frequency. The shaded area shows the reactance area (Goldman's triangle) which is determined by the X axis (frequency in Hertz), the Y axis (Kpa sL-1), and the reactance curve until Fres which is the point where the reactance is equal to zero.
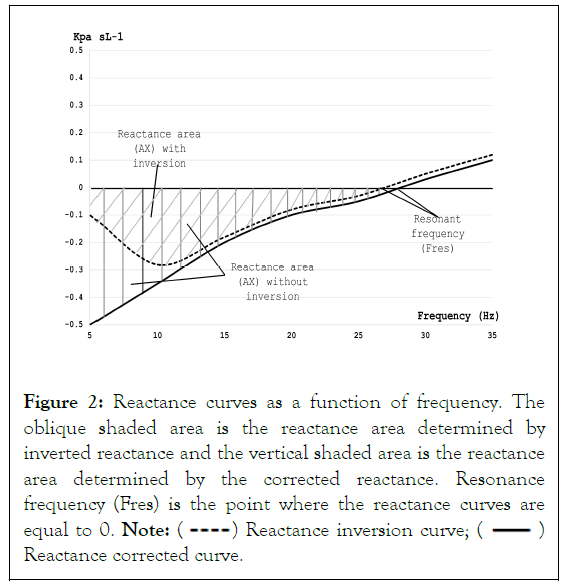
Figure 2: Reactance curves as a function of frequency. The
oblique shaded area is the reactance area determined by
inverted reactance and the vertical shaded area is the reactance
area determined by the corrected reactance. Resonance frequency (Fres) is the point where the reactance curves are equal to 0. Note:  Reactance inversion curve;
Reactance inversion curve;  Reactance corrected curve.
Reactance corrected curve.
The purpose of this review was to describe the available scientific evidence that has reported this reackPasL-1tance reversal in pediatric respiratory diseases.
Methodology
A review of the scientific evidence on reactance inversion was carried out. The search for articles was carried out in March 2024 in the Medline (PubMed), Web of Science (WOS), EBSCO Host, Science Direct, and SCOPUS databases. MeSH terms and free terms in their English version were used. The terms were grouped into two dimensions: i) reactance inversion ii) children. The Boolean operator “y'' was used to integrate the two dimensions. In addition, abstracts of publications published at the American Thoracic Society (ATS) and European Respiratory Society (ERS) congresses were reviewed. The articles found were grouped into three categories: cystic fibrosis, prematurity, and asthma.
Results
Five studies were found where RI is investigated. Four of these studies corresponded to publications and one to a presentation at the ATS congress. According to the type of study, one clinical case and four cross-sectional studies were found. According to the type of chronic disease, one study was found that analyzes RI in cystic fibrosis, two studies describe it in prematurity with or without bronchopulmonary dysplasia, and other two studies relate it to bronchial asthma.
Discussion
The evidence found in this review demonstrates that RI is not limited to a single pediatric respiratory pathology. RI is a transversal pathophysiological phenomenon whose genesis could be multifactorial. The research characteristics in RI grouped into categories by disease are described below.
Reactance inversion and cystic fibrosis
RI was reported for the first time in 2019 in a 6-year-old boy with cystic fibrosis who required hospitalization due to respiratory exacerbation. The patient underwent IOS upon admission and before medical discharge. The therapy administered for exacerbation improved the clinical symptoms and the Rrs and Xrs parameters of the IOS. However, the Xrs curve of the IOS (admission and discharge) showed that RI was evident at approximately a frequency of 7 hertz. The authors proposed that this finding could be explained by the differences in respiratory time constants of the alveolar units. Obstructed units with high time constants may not have sufficient time to distend at high frequencies, resulting in lower volume change (greater elastic reactance) for given pressure swings at the mouth. Conversely, at lower frequencies units have more time to fill, leading to greater small airway and alveolar recruitment and the elastic reactance would be diminished, which could reflect the inhomogeneity in ventilation present in this disease [9].
Reactance inversion and prematurity
A study performed IOS on children aged 4 to 6 years with a history of prematurity, finding two patterns of Xrs curves: with RI and without RI. At frequencies of 10 Hertz, children with RI showed significantly more negative Xrs (-0.35 kPasL-1 vs -0.16 kPasL-1, p=0.009) and greater intra-respiratory differences (Xrsex-Xrsin 0.09 kPasL-1 vs 0.04 kPasL-1, p=0.004) than children without RI. This reflects that the presence of RI can alter the interpretation of Xrs values at lower frequencies, which could be explained by greater expiratory narrowing of the airway [10]. In another cohort of premature children born at less than 29 weeks of gestation (high risk of bronchopulmonary dysplasia) who underwent IOS between 5 and 7 years, it was found that at frequencies of 10 Hertz the group with RI had higher values of Rrs (0.92 kPasL-1 vs 0.69 kPasL-1, p=0.048), greater intrarespiratory difference in Rrs (0.2 kPasL-1 vs 0.07 kPasL-1, p=0.009) and greater intrarespiratory difference in Xrs (0.1 kPasL-1 vs 0.02 kPasL-1 , p = 0.044) than children without RI. The authors hypothesize that this phenomenon could be explained by tracheobronchomalacia, which is common in premature infants [11]. In these two studies, it was postulated that the RI phenomenon may make the interpretation of the Xrs difficult at very low frequencies such as 5 hertz (X5), recommending its replacement by X10. This is probably true for Oscillometers that do not have the automatic X5 correction software. In the Oscillometers that have this correction system, the effect of RI would be eliminated, delivering its real value (X5c) that would be more negative and representative of the pathophysiology of the patient and their disease.
Reactance inversion and asthma
A cross-sectional study carried out in a large number of children with persistent asthma demonstrated that the prevalence of RI decreases linearly with age (preschoolers 83.5%, schoolchildren 66.2%, and adolescents 43.3%, p<0.0000001). At all ages, the FEV1 averages were lower in spirometry and IOS parameters tha t reflect tota l (R5) and peripheral airway obstruction such as AX resistance difference at 5 minus 20 Hertz (DR5-R20) were significantly higher in the group in which the corrected reactance at 5 Hertz was used (X5c) compared to the group in which reactance at 5 Hertz was used without correction (X5). Furthermore, the X5c parameter correlated better than X5 with IOS-spirometry parameters, such as R5, AX, DR5-R20, and FEF25-75 in all categories. From this study, it is clear that RI is a common phenomenon in persistent asthma, being more frequent in preschoolers and schoolchildren. Furthermore, the corrected value of reactance at 5 Hertz (X5c) correlates better than the value of reactance at 5 Hertz without correction (X5) in those parameters that measure peripheral airway obstruction in both spirometry and IOS [12]. In a recent publication carried out on 62 school children with moderate-severe asthma in controller treatment. Three groups were identified: Group 1 without RI, group 2 with RI that disappears after bronchodilator, and group 3 with RI that persists after bronchodilator. Children with RI (groups 2 and 3) had lower birth weights than those in group 1 (0.9 and 0.6 kg less, respectively). RI was also more frequent in children with a lower gestational age, with an average of 3 weeks less in group 2 than in group 1. Patients with RI had worse lung function in spirometry (lower FEV1 and FEF25-75) than those without RI. Two groups of patients with RI were identified: A group in which the RI disappeared after the bronchodilator and another group in which the RI persisted after the bronchodilator, which was associated with greater resistance of the total airway (R5) and the airway peripheral airway (AX, DR5-R20 and DR5-R20/R5) in IOS. The findings of this study could indicate that RI is a marker of peripheral airway obstruction in pediatric asthma, and that could be related to the lower gestational age or birth weight [13].
Conclusion
RI is a recent finding found in the IOS of pediatric patients with cystic fibrosis, prematurity with or without bronchopulmonary dysplasia, and asthma. Its presence has been associated with decreased lung function in spirometry, as well as intrarespiratory differences or small airway dysfunction in IOS. This new phenomenon could be a marker of severity in pediatric respiratory diseases whose causes are still unknown. More studies are required to understand its clinical significance and long-term consequences.
Conflict of Interest Statement
The author has no conflicts of interest to declare.
Funding
The author has no relevant financial or non-financial interests to disclose
References
- Vogel J, Smidt U. Impulse oscillometry: Analysis of lung mechanics in general practice and the clinic, epidemiology and experimental research. pmi-Verlag-Gruppe; 1994.
- Bednarek M, Grabicki M, Piorunek T, Batura-Gabryel H. Current place of impulse oscillometry in the assessment of pulmonary diseases. Respir Med. 2020;170:105952.
[Crossref] [Google Scholar] [PubMed]
- Kaminsky DA, Simpson SJ, Berger KI, Calverley P, De Melo PL, Dandurand R, et al. Clinical significance and applications of oscillometry. Eur Respir Rev. 2022;31(163).
[Google Scholar] [PubMed]
- King GG, Bates J, Berger KI, Calverley P, de Melo PL, Dellacà RL, et al. Technical standards for respiratory oscillometry. Eur Respir J. 2020;55(2).
[Google Scholar] [PubMed]
- Bhatawadekar SA, Leary D, Maksym GN. Modelling resistance and reactance with heterogeneous airway narrowing in mild to severe asthma. Can J Physiol Pharmacol. 2015;93(3):207-214.
[Crossref] [Google Scholar] [PubMed]
- Bhatawadekar SA, Leary D, de Lange V, Peters U, Fulton S, Hernandez P, et al. Reactance and elastance as measures of small airways response to bronchodilator in asthma. J. Appl. Phys. 2019;127(6):1772-1781.
[Crossref] [Google Scholar] [PubMed]
- McDowell KM. Recent diagnosis techniques in pediatric asthma: Impulse oscillometry in preschool asthma and use of exhaled nitric oxide. Immunol Allergy Clin. 2019;39(2):205-219.
[Google Scholar] [PubMed]
- Gupta N, Sachdev A, Gupta D, Gupta S. Oscillometry-The future of estimating pulmonary functions. Karnataka Paediatr J. 2021;35(2):79-87.
- Allen JL, Ren CL, McDonough J, Clem CC. " Reactance inversion" at low frequencies in a child undergoing treatment of a cystic fibrosis exacerbation. Pediatr Investig. 2019;3(04):257-260.
[Crossref] [Google Scholar] [PubMed]
- Allen JL, McDonough J, Ren CL, Clem C, DeMauro S, Chidambaram A, et al. Ain't Misbehavin':" Reactance inversion" at low frequencies during lung function measurement by Impulse Oscillometry (IOS) in former preterm children. InC28. Pediatric Respiratory Physiology. Am Thorac Soc. 2020:A4673-A4673.
- Tsukahara K, Scully T, McDonough J, Boas H, DeMauro SB, Ren CL, et al. Reactance inversion in a cohort of former preterms: Physiology or artifact?. Pediatr Pulmonol. 2023;58(9):2681-2684.
[Crossref] [Google Scholar] [PubMed]
- González Vera R, Vidal Grell A, Yarur AM, Meneses CO, Castro-Rodriguez JA. “Reactance inversion” at low frequencies during lung function measurement by impulse oscillometry in children with persistent asthma. J Asthma. 2022;59(8):1597-1603.
[Google Scholar] [PubMed]
- González Vera R, Grell AV, Castro-Rodríguez JA, Palomino Montenegro MA, Yarur AM. Reactance inversion in moderate to severe persistent asthma: Low birth weight, prematurity effect, and bronchodilator response. J Asthma. 2024:1-20.
[Crossref] [Google Scholar] [PubMed]
Citation: Vidal A (2024) Reactance inversion in pediatric respiratory diseases. Health Care Curr Rev. 12:399.
Copyright: © 2024 Vidal A. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

