Indexed In
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2023) Volume 7, Issue 4
Randomised Controlled Trial for Evaluation of Post Operative Analgesia after Ultrasound Guided Oblique Subcostal Transverse Abdominis Plane Block versus Erector Spinae Plane Block in Patients Undergoing Laparoscopic Cholecystectomy under General Anaesthesia
Shweta Mahaja*Received: 20-Nov-2023, Manuscript No. JSA-23-23955; Editor assigned: 22-Nov-2023, Pre QC No. JSA-23-23955 (PQ); Reviewed: 06-Dec-2023, QC No. JSA-23-23955; Revised: 13-Dec-2023, Manuscript No. JSA-23-23955 (R); Published: 20-Dec-2023, DOI: 10.35248/2684-1606.23.07.225
Abstract
Objectives: Despite laparoscopic cholecystectomy minimally invasive nature, it is not without pain. Considering the studies and facts mentioned before in the text we have planned to study the comparative efficacy of ultrasound guided bilateral oblique subcostal transverse abdominis plane block with bilateral erector spinae plane block in post operative analgesia in patients undergoing laparoscopic cholecystectomy.
Methods: The randomised controlled study was conducted at Indira Gandhi Medical College, Shimla, India, from March 2020 to March 2021. Patients were given blocks according to the computer-generated randomisation 30 minutes before shifting to the operation theatre. Group A received B/L Transversus Abdominis Plane (TAP) and group B received B/L ESP block. Patient VAS score, Numeric Rating Scale (NRS) score and demand of rescue analgesia with patient satisfaction was recorded for 48 hrs post-operatively.
Results: A total of 70 patients were included (35 in each group). In the post-operative period, the mean Visual Analog Scale (VAS) scores were statistically significant up to 4 hours postoperatively between the two groups with significantly lower VAS scores in Group B than in Group A. The mean time of first analgesic requirement in group A and group B was 3.83 ± 1.2 and 6.79 ± 4.2 hours respectively. Erector Spinae Plane Block (ESP) group received lesser doses of rescue analgesic as compared to OSTAP group showing better analgesia in ESP than Oblique Subcostal Transversus Abdominis Plane Block (OSTAP).
Conclusion: Both TAP and ESP blocks can be used to provide post-operative analgesia with stable intraoperative hemodynamics with no complications in laparoscopic cholecystectomy. However, ESP as compared to OSTAP block has lower VAS scores, lesser demand for rescue analgesic and prolonged duration of analgesia. ESP is simple, easier to learn and perform and provides better patient satisfaction without causing any noticeable side effects.
Keywords
Cholelithiasis; Laparoscopic cholecystectomy; Post operative pain; Post-operative analgesia; Oblique subcostal transverse abdominal plane block; Erector spinae plane block; VAS score
Introduction
For past 100 years, classic cholecystectomy has been the surgery of choice for removal of diseased gall bladder until 1987 when laparoscopic cholecystectomy became the gold standard for treatment of cholelithiasis [1]. Despite its minimally invasive nature, laparoscopic cholecystectomy is not without pain. Patients experience considerable amount of pain in first 24 hours post operatively and the etiology of pain is multi factorial which includes pain at trocar site (somatic pain), visceral pain (intraabdominal pain), and shoulder tip pain which is a referred visceral pain [2]. The management strategies involve the use of pharmacological methods like the use of NSAIDS/COX2 inhibitors, local anesthetic infiltration at the site of incision as well as intraperitoneally. The journey of pain alleviation in laparoscopic surgeries have moved from classic era of general anaesthesia to spinal and epidural anaesthesia which were superseded by more advanced techniques like fascial plane blocks including Rectus sheath block, Transverse abdominis plane block and Erector spine plane block. The Ultrasound guided fascial plane blocks has revolutionized the pain control regimen as the blind techniques may cause inappropriate blockade and even injury to the abdominal viscera. Later studies showed that the distribution of a Transverse abdominis plane block was non dermatomal and did not cross the midline [3]. Hence, it failed to provide complete analgesia for the abdominal surgeries along the midline and upper quadrant. Therefore, an optimal analgesia for midline surgeries was required and new modalities like Erector spinae plane block came into light. Ultrasound guided Erector spinae plane block is described as a novel technique, which can be useful in thoracic and abdominal surgeries [3]. When performed bilaterally the analgesia is even more sound [4,5].
Considering the studies and facts mentioned before in the text we have planned to study the comparative efficacy of ultrasound guided bilateral oblique subcostal transverse abdominis plane block with bilateral erector spinae plane block in post-operative analgesia in patients undergoing laparoscopic cholecystectomy.
Materials and Methods
After the approval from research and ethics committee, a Clinical Trials Registry - India (CTRI) registration CTRI/ 2020/11/029192 was obtained. The study was carried out in patients, undergoing Laparoscopic Cholecystectomy at IGMC, Shimla in the year 2020-2021 after obtaining written informed consent from the patients. The ASA 1 and ASA 11 patients with age group of 18 yrs-65 yrs were included in the study. After enrolment, the participants were randomly allocated to either the OSTAP group (Group A, n=35) or the ESP group (Group B, n=35). On the day of the surgery, a previously prepared and sealed opaque envelope containing the random group assignment was opened by research assistant who was not involved in this study. The group allocation was then conveyed to the block practitioner before block performance. To eliminate performance bias, all blocks were performed by experienced regional anesthesiologists. All anesthesiologists in charge of intraoperative anesthesia management, outcome assessors, patients and follow-up personnel were blinded to group allocation. We expected that a satisfactory percentage of patients receiving ESP and TAP block would have complete satisfaction regarding pain control. Therefore, we conducted a pilot study with 10 patients per group, none of which were included in this study. We calculated the sample size of 70 patients total to provide statistical power of 0.80 and one sided 97.5% CI. The data of the study was recorded in the record charts and the results were evaluated using statistical tests (Analysis of Variance (ANOVA), Chi-square, Mann-Whitney Test, Post-hoc test) as applicable. p-value>0.05 was taken as not significant, while p<0.05 was considered significant. Group A–Oblique Subcostal Transverse Abdominal Plane Block (OSTAP) with 15 ml of 0.25% bupivacaine on each side. Group B–Erector Spinae Plane Block (ESP) with 15 ml of 0.25% bupivacaine on each side.
After routine pre-anaesthetic check-up and routine investigations, the patients were explained about the procedure to be undertaken. The patients were informed about the use of Visual Assessment Scale (0-10), 0 for no pain and 10 for worst pain. Overnight fasting and routine pre medication was advised to the patients on the day before the surgery. Oblique Subcostal TAP Block was performed in supine position using high frequency linear transducer (6-13 Hz, Sonosite) with in plane technique. The transducer was placed immediately below the costal margin on the oblique part. The rectus abdominis, transverse abdominis, internal oblique and external oblique muscles are identified. A 23G spinal needle was inserted using in plane technique with approach from medial to lateral. After confirming the correct placement of the needle and the negative aspiration, the drug (0.25% bupivacaine 15 ml) was injected along the subcostal line in the transverse abdominis plane. Same procedure was applied on the other side with total drug volume of 30ml. Erector Spinae Plane Block under USG guidance was given with patients in sitting position. The transducer was placed lateral to T7 spinous process in a longitudinal parasagittal orientation. Erector Spinae Muscles were identified superficial to the tip of T7 transverse process. A 23G spinal needle was inserted by using out of the plane approach. The tip of the needle placed into fascial plane on the deep (anterior) aspect of ESP muscles. 15 ml of 0.25% bupivacaine was injected after confirming the position of the needle. Same procedure was repeated on the other side with total drug volume of 30 ml.
After 30 minutes the patients were shifted to OT and all patients were subjected to routine intraoperative monitoring. General anaesthesia was given by inj. Fentanyl 2 mcg/kg i.v. and inj. propofol 2 mg/kg i.v. Maintenance was done with Isoflurane 0.2% -1% and N2O and O2, 66% and 33% concentration respectively. Neuromuscular Blockade was achieved with inj. Atracurium 0.3 mg/kg i.v. and was maintained at 0.1 mg/kg i.v. Inj. Ondansetron 0.15 mg/kg i.v. vital monitoring was done throughout the surgery as per department protocol. Neuromuscular blockade was reversed with inj. Neostigmine 50 mcg/kg i.v. and glycopyrrolate 10 mcg/kg i.v.
The level of postoperative pain was assessed in PACU every 30minutes for 1hour and then subsequently at 2,4,8 and 24 hrs post-operatively. Whenever VAS was more than 4 rescue analgesia with inj. Diclofenac 75 mg i.v. was given. If patients still complaints of pain within the duration of Diclofenac, a second rescue analgesic inj. Tramadol 50 mg i.v. was given and noted. The total dose of rescue analgesic given in first 48 hours was also calculated.
Postoperative nausea and vomiting were assessed. Patient satisfaction scoring was done according to 5 point Likert scale as classified in the following table. When patients were fully satisfied the score is 5, somewhat satisfied 4, undecided 3, not really satisfied 2 and not at all satisfied 1. Patients were monitored for any postoperative complications like haematomas, paraesthesia.
The research assistant also recorded demographic data, including type of surgery; surgical duration (defined as the interval from skin incision to closure) and propofol consumption.
Results
The data of the study was recorded in the record chart and results were evaluated using statistical tests (Chi-Square, Unpaired t-test) as applicable. p-Value >0.05 was taken as not significant, while p<0.05 significant, <0.01 highly significant and <0.00very highly significant.
All the data was tabulated and analyzed using SPSS for windows [SPSS version 22, IBM Corp, Armonk, NK].
Following statistical significance tests were applied:
1. Continuous data was analyzed using unpaired t-test for between group comparisons.
2. Categorical data was analyzed using Chi-square test.
3. Graph and tables were used to present the data.
Finally, the calculated values were compared and the level of significance was determined. The level of significance was set at p<0.05.
Two patients from group A and 2 from group B were excluded because they complained of severe pain in Post Anesthesia Care Unit (PACU) immediately after shifting as (VAS>5) and were taken as block failures (Figure 1).
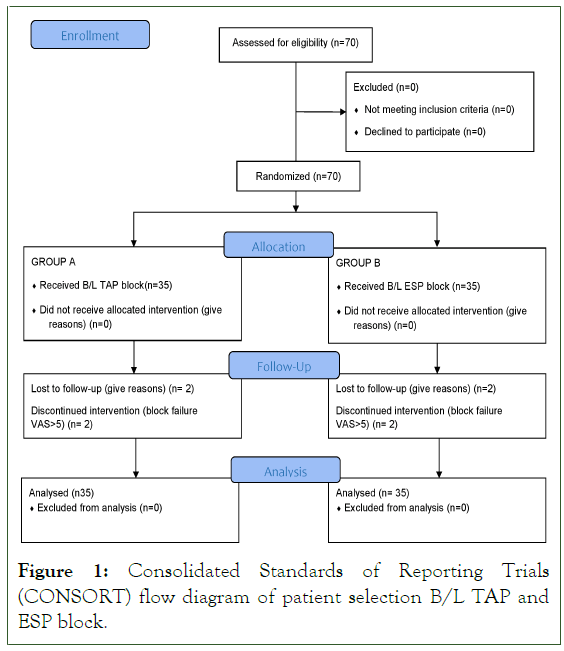
Figure 1: Consolidated Standards of Reporting Trials (CONSORT) flow diagram of patient selection B/L TAP and ESP block.
Following observations were made:
The demographic data and baseline parameters with respect to HR, Mean Arterial Blood Pressure (MAP) and SPO2 were found to be comparable between the two groups (Table 1 and Figure 2). The difference in intra-operative vitals with respect to HR, MAP and SPO2 of the patients between two study groups was not statistically significant (Figure 3).
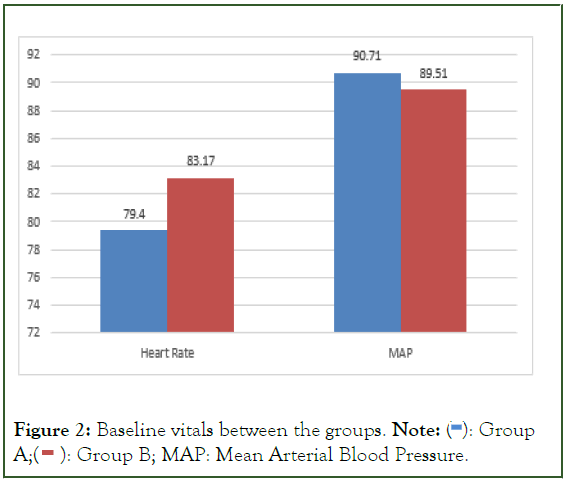
Figure 2: Baseline vitals between the groups. Note:  Group A;
Group A;  Group B; MAP: Mean Arterial Blood Pressure.
Group B; MAP: Mean Arterial Blood Pressure.
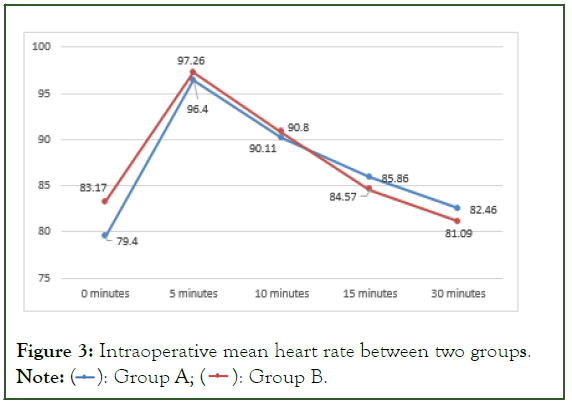
Figure 3: Intraoperative mean heart rate between two groups. Note:  Group B.
Group B.
| Parameter | Group A (n=35) | Group B (n=35) | p value | Result |
|---|---|---|---|---|
| Age | 40.86 ± 10.7 | 41.0 ± 12.3 | 0.9 | Not significant |
| Weight | 60.31 ± 9 | 61.3 ± 9.2 | 0.65 | Not significant |
Note: P=Probability; n=Total number
Table 1: Demographic profile.
It was found that there was no statistically significant difference in heart rates (PACU) of study participants between group A and group B at any point of time. It was comparable in two groups at all time intervals.
It was found that participants among group A had statistically significantly higher MAP (PACU) than those in group B at 30 minutes (p=0.047) and 60 minutes (p=0.02) respectively. There was no statistically significant difference in MAP among study participants between group A and group B at 0 minutes (p=0.8), 2 hours (p=0.2), 4 hours (p=0.9) and 8 hours (p=0.48) respectively (Figure 4).
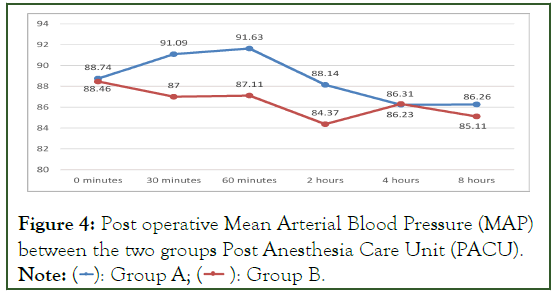
Figure 4: Post operative Mean Arterial Blood Pressure (MAP)
between the two groups Post Anesthesia Care Unit (PACU). Note: 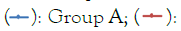 Group B.
Group B.
The post operative mean VAS score among study participants of group A were statistically significantly (p<0.05) more up to 4 hours post operatively than that of group B. The mean duration of surgery in majority of the cases was 30 minutes. However, VAS scores were found to be comparable at 8 hours post operatively (p>0.05) in both the groups.
At 24 hours postoperatively, mean VAS score in group A was 0.8 ± 0.99 and group B was 0.94 ± 0.73 which was statistically insignificant (p=0.49) (Table 2).
| Group | N | Mean | SD | p value | ||
|---|---|---|---|---|---|---|
| Post OP | 0 minutes | Group A | 35 | 0.54 | 1.04 | 0.005* |
| Group B | 35 | 0.03 | 0.17 | |||
| PACU | 30 minutes | Group A | 35 | 1.2 | 1.51 | 0.001* |
| Group B | 35 | 0.17 | 0.45 | |||
| 60 minutes | Group A | 35 | 1.69 | 1.73 | 0.001* | |
| Group B | 35 | 0.31 | 0.58 | |||
| Ward | 2 hours | Group A | 35 | 2.11 | 2.11 | 0.001* |
| Group B | 35 | 0.57 | 1.15 | |||
| 4 hours | Group A | 35 | 1.91 | 1.67 | 0.04* | |
| Group B | 35 | 1.2 | 1.21 | |||
| 8 hours | Group A | 35 | 1.26 | 1.34 | 0.055 | |
| Group B | 35 | 1.83 | 1.1 | NS | ||
| 24 hours | Group A | 35 | 0.8 | 0.99 | 0.49 | |
| Group B | 35 | 0.94 | 0.73 | NS | ||
| 48 hours | Group A | 35 | 0.06 | 0.24 | 0.7 | |
| Group B | 35 | 0.09 | 0.37 | NS |
Note: Level of significance at P<0.05; N=frequency; SD=Standard Deviation NS-Not significant and *=Statistically significant using paired ‘t’ test; Post OP=Postoperative, PACU: Post Anesthesia Care Unit, P=Probability.
Table 2: Post operative Visual Analogue Scale (VAS) between the two groups.
The mean time of first analgesic requirement in group A and group B was 3.83 ± 1.2 and 6.79 ± 4.2 hours respectively (Figure 5). It was found that time for first analgesic requirement was shorter among study participants in group A than those in group B and it was statistically significant (p=0.001). Out of the 70 patients, 15 patients from group A (42.85%) and 23 from group B (65.7%) were given inj. Diclofenac single dose as rescue analgesic. While 15 (42.85%) patients from group A and 12 (34.3%) patients from group B were given inj. Diclofenac and inj. Tramadol as rescue analgesic in first 24 hours respectively. Only 5 (14.3%) patients from group A required 3 doses (inj. Diclofenac+inj. Tramadol+inj. Diclofenac) of rescue analgesic while none from group B required 3 doses of rescue analgesic in first 24 hours (Table 3).
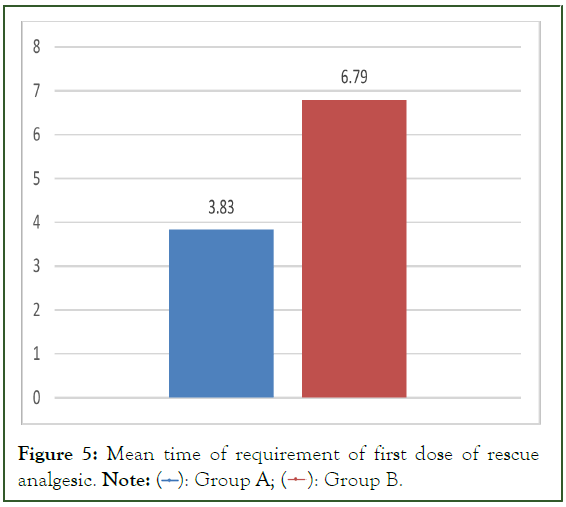
Figure 5: Mean time of requirement of first dose of rescue analgesic. Note:  Group B.
Group B.
| Group A (N=35) | Group B (N=35) | p value 0.03 Significant |
|||
| Injection | N | % | N | % | |
| Inj. Diclofenac | 15 | 42.85 | 23 | 65.7 | |
| Inj. Diclofenac + Inj. Tramadol | 15 | 42.85 | 12 | 34.3 | |
| Inj. Diclofenac + Inj. Tramadol + Inj. Diclofenac | 5 | 14.3 | 0 | 0 | |
Note: P=Probability, N=Frequency; Level of significance at P<0.05; significant using Chi square test
Table 3: Total dose of rescue analgesia between the groups.
It was found that PONV was more among study participants of group A than group B, however that was statistically insignificant (p=0.3). There were no complications reported like hematoma at block site, pneumothorax or any hemodynamic instability.
The patient satisfaction was assessed using Likert 5-point patient satisfaction score. It was found that participants who were totally satisfied were significantly more in Group B than in Group A (P=0.004). Comparing the values, patients in group B were more satisfied than patients in group A with p-value 0.004 which was statistically significant. Also, patients who were not satisfied at all were more in group A than group B with p-value of 0.02 which was statistically significant (Table 4).
| Group A | Group B | Total | p value | |
|---|---|---|---|---|
| Not at all Satisfied | 8 (22.9) | 1 (2.9) | 9 | 0.02* |
| Not really satisfied | 5 (14.3) | 2 (5.7) | 7 | 0.15 |
| Undecided | 12 (34.3) | 6 (17.1) | 18 | 0.27 |
| Somewhat satisfied | 9 (25.7) | 15(42.9) | 24 | 0.22 |
| Very much satisfied | 1 (2.9) | 11(31.4) | 12 | 0.004** |
| Total | 35 | 35 | 70 |
Note: P=Probability; *=Statistically significant using paired ‘t’ test
Table 4: Patient’s satisfaction level between the two groups
Discussion
Gall stone disease is very common in our population with a prevalence rate of 10-20%6. It is commonly associated with personal risk factors like age, gender, sedentary life style, obesity and dietary habits. In 1987 laparoscopic cholecystectomy was introduced [1]. Despite all the advantages like minimally invasive procedure, there is a considerable amount of pain and discomfort to the patient after laparoscopic cholecystectomy [2]. Laparoscopic cholecystectomies are mostly performed under general anaesthesia; however, there is increasing proclivity towards regional anaesthesia due to effective peri-operative pain control, improved patient comfort, early ambulation, shortened hospital stay and decreased burden on the PACU unit [6].
In 2009, El-Dawlatly AA used transverse abdominis plane block for laparoscopic cholecystectomy [7]. Later on, Hebbard P et al described use of Ultrasound guided TAP block for better visualization of the anatomical structures and the needle which resulted in more effective blockade and lesser discomfort to the patient [8]. With the search for better alternatives, in 2016 Forrero M et al, described Erector Spinae block which resulted in blockage of the dorsal and ventral rami of spinal nerve roots [9].
Both the blocks ESP and OSTAP help to maintain stable intraoperative hemodynamic. The study conducted by Abdelhamid BM et al, and Malawat A et al were also corresponding to our study [10,11].
Post operative analgesia was analysed using VAS score among both groups. In study conducted by Sahoo et al comparing USG guided OSTAP block versus ESP block versus control group in laparoscopic cholecystectomy for postoperative analgesia [12]. In their study they found that in first 6 hours post operatively the NRS score on coughing and movement was lower in ESP group than OSTAP group which was statistically significant(p<0.05) and after 6 hours it was comparable in both the groups. While in control group it was comparable after 9 hours. These finding were in accordance with our study. In the study conducted by Abdelhamid BM et al, VAS in the ESP group was significantly lower compared to TAP group at 12th post operative hour which was contradictory to our study results [10]. In another Root Canal Treatment (RCT) conducted by Ibrahim et al, comparing the analgesic efficacy of ESP versus OSTAP given bilaterally and trocar site infiltration with 40 ml of 0.25% bupivacaine [13]. Among the ESP and OSTAP group, mean VAS scores at movement and at rest were higher in the OSTAP group. These observations were comparable to our study.
In a study conducted by Kamel AA et al, in 2020 comparing bilateral USG guided ESP versus TAP block for post-operative analgesia after total abdominal hysterectomy [14]. It was seen that the VAS scores were significantly lowered in ESP group at 30 min, 2, 12, 16, 20 and 24 hours.
In our study also, it was observed that mean VAS score among ESP group participants were lower than OSTAP group participants throughout the post operative period.
The time of requirement of first dose of rescue analgesic post operatively were compared and it was observed that ESP bock provides longer duration of postoperative analgesia than the OSTAP block. The results of study conducted by Sahoo SP et al, was contradictory to our study but the study by Routray SS et al, was in correspondence to our study [12,15].
Finally, it was observed that there was statistically significant difference in the number of patients receiving doses of rescue analgesic between the two groups. ESP group received lesser doses of rescue analgesic as compared to OSTAP group showing better analgesia in ESP than OSTAP block. Also, the incidence of PONV was comparable between the two groups. Overall, the number of patients requiring anti emetic was slightly higher in the OSTAP group than ESP group. It was observed according to patient satisfaction scale that the patients in the ESP group were more satisfied than the OSTAP group.
The limitations in our study were that, the patient dissatisfaction due to needle prick bilaterally while performing the block which can be overcome by performing blocks after induction. It is convenient to perform OSTAP block under general anesthesia. On the other hand, positioning for ESP block can be a challenge after anesthesia and requires a dedicated team of operating room personnel for positioning only. Also, the patients were not blinded. Block was given before general anesthesia to assess the sensory blockade in awake patients. Thirdly, the duration of post operative blockade can be increased by increasing the dose of drug being used.
Conclusion
From our study we concluded that both OSTAP and ESP block can be used to provide post operative analgesia with stable intraoperative hemodynamics with no complications in laparoscopic cholecystectomy. However, ESP as compared to OSTAP block has lower VAS scores, lesser demand for rescue analgesic and prolonged duration of analgesia. ESP is simple, easier to learn and perform and provides better patient satisfaction without causing any noticeable side effects.
Acknowledgement
All research performed by department of Anaesthesia, Indira Gandhi Medical College, Shimla, Himachal Pradesh, India.
Funding
None
Conflicts of Interest
There are no conflicts of interest.
References
- Bucher P, Pugin F, Buchs NC, Ostermann S, Morel P. Randomized clinical trial of laparoendoscopic single-site versus conventional laparoscopic cholecystectomy. Br J Surg. 2011;98(12):1695-1702.
[Crossref] [Google Scholar] [PubMed]
- Bisgaard T, Warltier DC. Analgesic treatment after laparoscopic cholecystectomy: a critical assessment of the evidence. The Journal of the American Society of Anesthesiologists. 2006;104(4):835-846.
[Crossref] [Google Scholar] [PubMed]
- Støving K, Rothe C, Rosenstock CV, Aasvang EK, Lundstrøm LH, Lange KH. Cutaneous sensory block area, muscle-relaxing effect, and block duration of the transversus abdominis plane block: A randomized, blinded, and placebo-controlled study in healthy volunteers. Reg Anesth Pain Med. 2015;40(4):355-362.
[Crossref] [Google Scholar] [PubMed]
- Bonvicini D, Tagliapietra L, Giacomazzi A, Pizzirani E. Bilateral ultrasound-guided erector spinae plane blocks in breast cancer and reconstruction surgery. J Clin Anesth. 2018;44:3-4.
[Crossref] [Google Scholar] [PubMed]
- Chin KJ, Adhikary S, Sarwani N, Forero M. The analgesic efficacy of pre‐operative bilateral erector spinae plane (ESP) blocks in patients having ventral hernia repair. Anaesthesia. 2017;72(4):452-460.
[Crossref] [Google Scholar] [PubMed]
- Stinton LM, Shaffer EA. Epidemiology of gallbladder disease: Cholelithiasis and cancer. Gut Liver. 2012;6(2):172.
[Crossref] [Google Scholar] [PubMed]
- El-Dawlatly AA, Turkistani A, Kettner SC, Machata AM, Delvi MB, Thallaj A, Kapral S, Marhofer P. Ultrasound-guided transversus abdominis plane block: description of a new technique and comparison with conventional systemic analgesia during laparoscopic cholecystectomy. Br J Anaesth. 2009;102(6):763-767.
[Crossref] [Google Scholar] [PubMed]
- Hebbard P. Subcostal transversus abdominis plane block under ultrasound guidance. Anesth Analg. 2008;106(2):674-675.
[Crossref] [Google Scholar] [PubMed]
- Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block: a novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41(5):621-627.
[Crossref] [Google Scholar] [PubMed]
- Abdelhamid BM, Khaled D, Mansour MA, Hassan MM. Comparison between the ultrasound-guided erector spinae block and the subcostal approach to the transversus abdominis plane block in obese patients undergoing sleeve gastrectomy: A randomized controlled trial. Minerva Anestesiol. 2020;86(8):816-826.
[Crossref] [Google Scholar] [PubMed]
- Malawat A, Verma K, Jethava D, Jethava DD. Erector spinae plane block and transversus abdominis plane block for postoperative analgesia in cesarean section: A prospective randomized comparative study. J Anaesthesiol Clin Pharmacol. 2020;36(2):201.
[Crossref] [Google Scholar] [PubMed]
- Sahoo SP, Jayasingh SC, Routray SS, Mohapatra B. Laparoscopic Cholecystectomy-Comparison of two different techniques of ultrasound guided blocks for postoperative pain relief. International Journal of Health and Clinical Research. 2021;4(8):96-100.
- Ibrahim M. Erector spinae plane block in laparoscopic cholecystectomy, is there a difference? A randomized controlled trial. Anesth Essays Res. 2020;14(1):119.
[Crossref] [Google Scholar] [PubMed]
- Kamel AA, Amin OA, Ibrahem MA. Bilateral ultrasound-guided erector spinae plane block versus transversus abdominis plane block on postoperative analgesia after total abdominal hysterectomy. Pain Physician. 2020;23(4):375.
[Crossref] [Google Scholar] [PubMed]
- Routray SS, Mohanty R, Pradhan K, Pani S. Evaluation of efficacy of ultrasound guided erector spinae plane block and oblique subcostal transversus abdominis plane block for postoperative analgesia in laparoscopic cholecystectomy. Panacea J Med Sci. 2020;10(2):128-134
Citation: Mahajan S (2023) Randomised Controlled Trial for Evaluation of Post Operative Analgesia after Ultrasound Guided Oblique Subcostal Transverse Abdominis Plane Block versus Erector Spinae Plane Block in Patients Undergoing Laparoscopic Cholecystectomy under General Anaesthesia. J Surg Anesth. 7:225.
Copyright: © 2023 Mahajan S, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
