Indexed In
- Open J Gate
- Cosmos IF
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
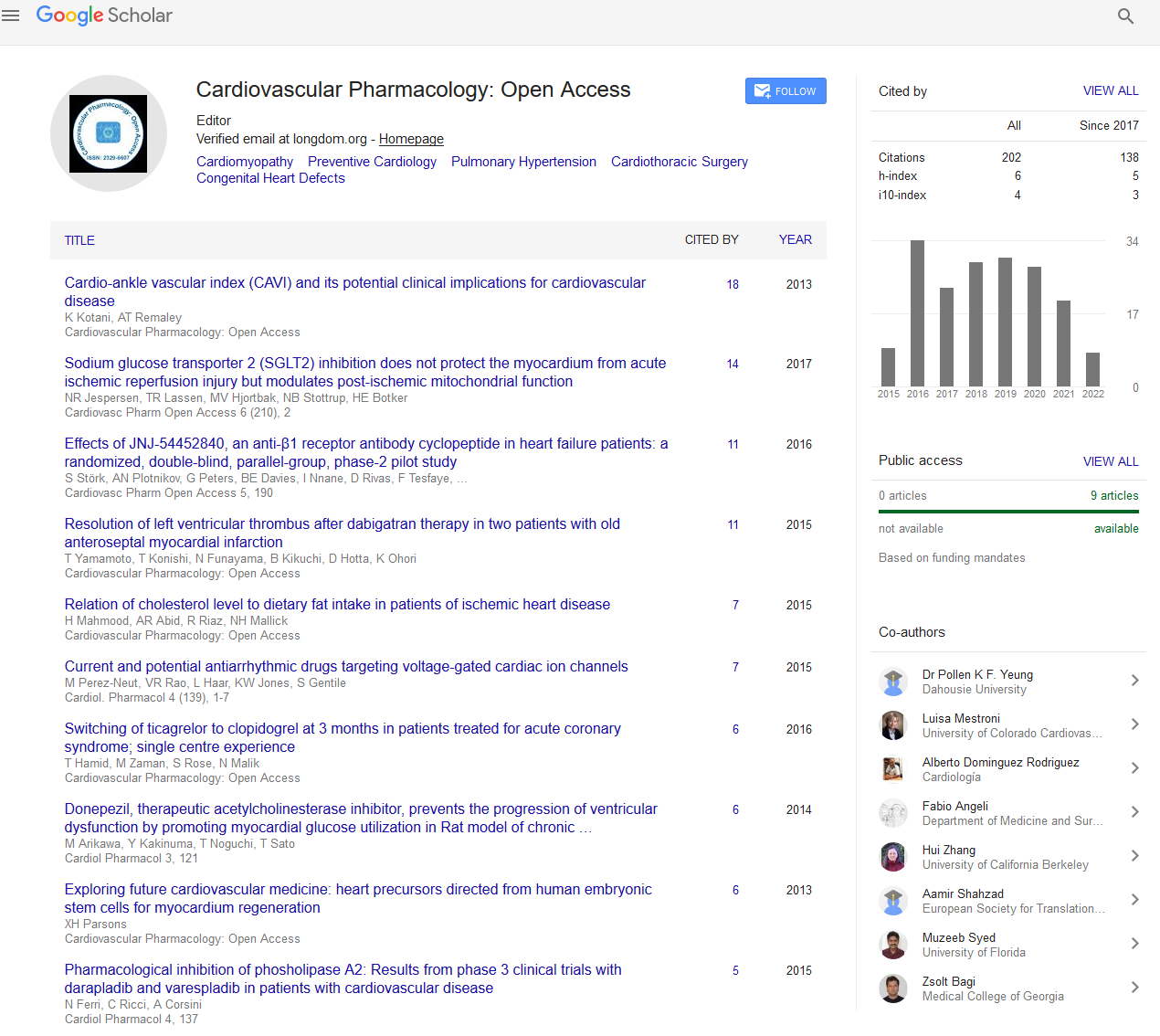
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Perspective - (2023) Volume 12, Issue 2
Pulmonary Hypertension (PH) Related to Chronic Obstructive Pulmonary Disease (COPD): An Overview
Joanne Bogaard*Received: 03-Mar-2023, Manuscript No. CPO-23-20482; Editor assigned: 06-Mar-2023, Pre QC No. CPO-23-20482 (PQ); Reviewed: 20-Mar-2023, QC No. CPO-23-20482; Revised: 27-Mar-2023, Manuscript No. CPO-23-20482 (R); Published: 03-Apr-2023, DOI: 10.35248/2329-6607.23.12.335
Description
The onset of pulmonary hypertension in COPD is related to an increased risk of severe acute exacerbations and has a negative impact on survival and exercise capacity. Regrettably, not all COPD patients who qualify for long-term oxygen therapy do so. Even in those who gain from long-term oxygen therapy, the high pulmonary artery pressure may be reversed but not normalized. Additionally, the new understanding of the crucial roles that endothelial dysfunction and inflammation play in the aetiology of PH justifies the use of statins and certain pulmonary vasodilators with antiproliferative characteristics.
The WHO classifies Pulmonary Hypertension (PH) related to lung disorders and/or hypoxemia as category 3, which includes PH secondary to Chronic Obstructive Pulmonary Disease (COPD). Variable definitions of PH in COPD include resting mean Pulmonary Artery Pressure (mPAP) >20-25 mm Hg. PH in COPD has a negative impact on endurance and exercise capacity and is linked to a higher incidence of acute exacerbations. Endothelial dysfunction and systemic inflammation also play significant roles in the aetiology of PH, according to recent investigations. There is a great deal of interest in researching specific pulmonary vasodilators with antiproliferative capabilities in PH related to COPD as a result of their recent development. Depending on how PH is defined (mPAP >20 versus >25 mm Hg), how severe the COPD is (Forced Expiratory Volume in one second (FEV1)), and how the pulmonary artery pressure is measured, the prevalence of PH in stable COPD can range from 20% to 91% (echocardiography versus right heart catheterization).
Stable-state activity may increase Pulmonary Artery Pressure (PAP) to around twice the level of its resting value in individuals with severe COPD, whether or not they have resting PH. Activities of everyday life like walking or climbing stairs might temporarily cause PH in those with severe COPD. When REM sleep occurs in people with severe COPD, oxygen saturation may drop by 20%-30% while PAP may increase by as much as 20 mm Hg. PAP may increase by as much as 20 mm Hg during an acute COPD exacerbation before dropping back to normal following recovery. Before Long-Term Oxygen Therapy (LTOT) became widely accessible, it was well known that the presence of PH was linked to a poor prognosis for COPD. The level of mPAP, rather than the FEV1, the degree of hypoxemia, or the degree of hypercapnia, is the greatest predictive predictor, even on LTOT. Patients with starting mPAP >25 mm Hg had a 5-year survival rate of just 36%, while patients with beginning mPAP ≤ 25 mm Hg have a 5-year survival rate of 62%. Exercise capacity can also be predicted independently by PH.
PAP is dependent on Cardiac Output (CO), Pulmonary Vascular Resistance (PVR), and Pulmonary Artery Wedge Pressure (PAWP) in terms of hemodynamics. Whereas PH during exercise arises mostly from an increase in CO in the face of a relatively "fixed" PVR, that is, there is less recruitability and distensibility of pulmonary arteries, resting PH in COPD is primarily caused by a raised PVR. PVR, PAWP, and PAP are all increased by hyperinflation, especially when exercising. The loss of the pulmonary vascular bed caused by emphysema, polycythemia, and hyperinflation, as well as hypoxic pulmonary vasoconstriction and vascular remodelling, have all been linked to higher PVR in COPD in the past. Endothelial dysfunction and systemic inflammation are now understood to be important factors in the development of PH. In fact, endothelial dysfunction brought on by cigarette smoke is thought to be the first event in the natural history of PH in COPD.
The Right Ventricle (RV) gradually experiences hypertrophy and dilatation-cor pulmonale in response to the elevated PVR. The decreased RV Ejection Fraction (EF) is due to this rise in RV End-Diastolic Volume (RVEDV), or preload, to maintain a normal Stroke Volume (SV). In stable COPD patients, the RV contractility as measured by the end systolic pressure-volume relation is normal, and the RV functions along an extension of the Frank-Starling curve for typical RV function. When COPD is stable, resting PH is often mild to moderate (mPAP 20-35 mm Hg) and not present until the disease has progressed (FEV1 50%). Obstructive Sleep Apnea (OSA), Pulmonary Embolism (PE), and left heart disease are a few additional causes of severe PH (mPAP >35-45 mm Hg), which are uncommon (3%-13%). Patients with growing dyspnea with stable airway obstruction or those who have mild to moderate airway obstruction with a very low diffusing capacity, severe hypoxemia, and hypocapnia should be suspected of having PH related to COPD. Before attributing PH to COPD, a diagnosis of PH in COPD should motivate a search for other causes of PH, especially left heart dysfunction, OSA, and PE.
Citation: Bogaard J (2023) Pulmonary Hypertension (PH) Related to Chronic Obstructive Pulmonary Disease (COPD): An Overview. Cardiovasc Pharm. 12:335.
Copyright: © 2023 Bogaard J. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.