Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- The Global Impact Factor (GIF)
- China National Knowledge Infrastructure (CNKI)
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
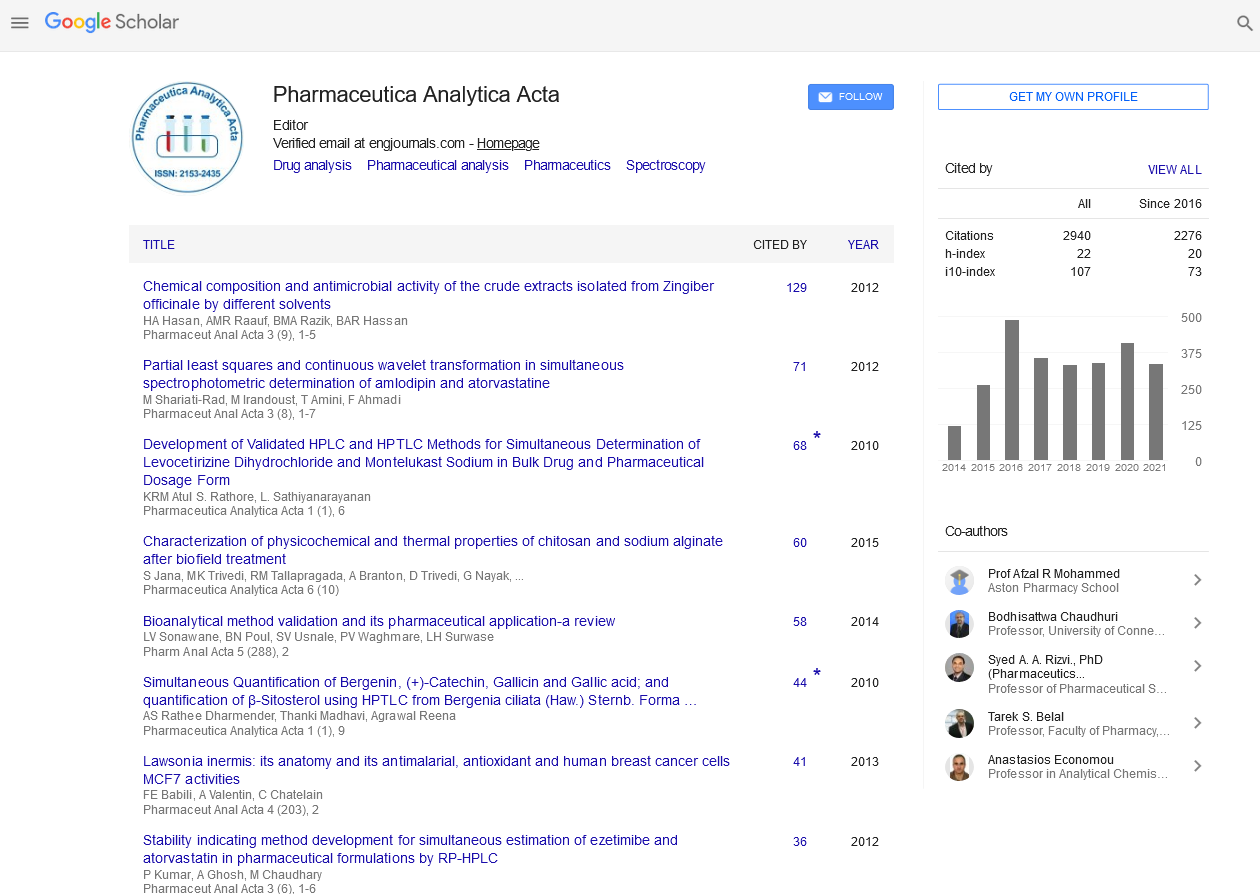
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Perspective - (2022) Volume 13, Issue 3
Prevalence of Drug-Drug Interactions in Sarcoma Patients
Lobos Saida*Received: 01-Mar-2022, Manuscript No. PAA-22-16446; Editor assigned: 04-Mar-2022, Pre QC No. PAA-22-16446(PQ); Reviewed: 18-Mar-2022, QC No. PAA-22-16446; Revised: 25-Mar-2022, Manuscript No. PAA-22-16446(R); Published: 01-Apr-2022, DOI: 10.4172/ 2153-2435.22.13.664
Description
Drug-Drug Interactions (DDI) have become a major concern in the treatment of cancer patients. However, there is a scarcity of evidence in sarcoma patients. The aim of this study was to determine the frequency of DDI associated with antitumor treatments, identify risk factors for DDI, and assess the impact of a pharmacist assessment before to anticancer treatment. The development of molecularly targeted drugs, such as pazopanib and regorafenib in nonadipocytic STS, imatinib in dermatofibrosarcoma, and crizotinib in inflammatory myofibroblastic tumour, has opened new therapeutic options for STS treatment. Regorafenib, cabozantinib, and lenvatinib are multitargeted tyrosine kinase inhibitors that have shown activity in individuals with advanced bone sarcoma.
Drug interaction occurs when the effect of a drug changes due to the presence of another drug, herbal medicine, food or drink. DDI in oncology is especially important due to its narrow therapeutic index and the toxicity of some anticancer drugs. Cancer patients are at increased risk of DDI because they often take drugs besides antineoplastic agents, such as drugs to relieve symptoms of cancer, treat the toxicity caused by cancer treatment, or treat comorbidity. Therefore, one-third of outpatients with cancer are exposed to potential DDI. In addition, about 40% of cancer patients treated with conventional treatments also have alternative medicine (CM), which is defined as a medical approach that is not usually part of traditional medicine, such as herbs, vitamins, naturopathic medicine, and homeopathy. Although some CM may be beneficial, others may cause herb-drug or vitamin-drug interactions, which could affect the efficacy or safety profile of cancer treatments. For the first time we identified the baseline factors associated with DDI in sarcoma patients. The type of antitumor protocol seems primordial since patients treated with TKI were at higher risk to present a major DDI. Different factors may explain this result. First, oral targeted therapies such as TKI are prescribed for long periods of time, in patients with potential comorbidities. Second, all TKIs (pazopanib, sorafenib, sunitinib, and regorafenib) are metabolized by the cytochrome P450 enzyme (CYP) and appear in the presence of CYP3A4 inhibitors or inducers. It can cause significant fluctuations in metabolic clearance. Finally, PPI administration is known to significantly reduce the bioavailability of TKIs such as pazopanib. Overall, the risk of DDI in sarcoma patients treated with TKI is expected to increase by 28%. In contrast, patients treated with gemcitabine-based protocols have a 14% reduction in the risk of DDI. One explanation may be related to CYPindependent gemcitabine metabolism, unlike TKIs. Therefore, pharmacists could favor to perform medication reconciliation in sarcoma patients treated with TKI rather than in patients treated with gemcitabineprotocol.
Clinical pharmacist interventions on DDIs were more frequently required among sarcoma patients treated with TKI than intravenous cytotoxic chemotherapy. Since the risk of toxicity is higher in TKItreated patients, we developed in our center a follow up of these patients by plasma drug monitoring and systematic phone calls. Plasma drug monitoring, could be also helpful to detect new pharmacokinetic drug interactions or herb-drug interactions.
Citation: Saida L (2022) Prevalence of Drug-Drug Interactions in Sarcoma Patients. Pharm Anal Acta. 13:664.
Copyright: © 2022 Saida L. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.