Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- ResearchBible
- Ulrich's Periodicals Directory
- Access to Global Online Research in Agriculture (AGORA)
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- MIAR
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2024) Volume 15, Issue 2
Preliminary Data on the Prevalence and Associated Risk Factors of Urinary Schistosomiasis among School Children in Abebche Commune, Eastern Chad
Mahamat Hassan Abdel-Aziz1,2,3, Hamit Mahamat Alio1,2,4*, Kemba Samafou1,2, Abdel-Mahamoud Adam3 and Bilong Bilong Charles Felix12Department of Medical Parasitology and Mycology of the Health and Human Sciences, University of N'Djamena, N’Djamena, Chad
3Department of Science and Technology, National Institute of Science and Technology of Abeche, Abeche, Chad
4Department of the Renaissance, University Hospital of N’Djamena, N’Djamena, Chad
Received: 04-Oct-2023, Manuscript No. JBP-23-23240; Editor assigned: 09-Oct-2023, Pre QC No. JBP-23-23240 (PQ); Reviewed: 23-Oct-2023, QC No. JBP-23-23240; Revised: 30-Oct-2023, Manuscript No. JBP-23-23240 (R); Published: 06-Nov-2023, DOI: 10.35248/2155-9597.24.15.507
Abstract
Schistosomiasis is the world's second-largest parasitic endemic caused by trematodes of the genus Schistosoma. The aim of this study was to determine the prevalence of urinary schistosomiasis among school children in two areas, peri-urban and urban, in the commune of Abeche. A parasitological survey was carried out among school children in the town of Abeche. Parasitological analyses were carried out at the Abeche Provincial Hospital laboratory and the Chemistry and Microbiology Laboratory of the institute National superior the sciences and technology d'Abeche. The method used for parasitological analysis was centrifugation. A total of 723 pupils aged 5 to 15, 587 boys (81.18%) and 136 girls (18.82%) from 5 elementary school in the peri-urban area and 4 elementary school and 2 secondary schools in the urban area, took part in the study. The overall prevalence of Schistosoma haematobium schistosomiasis was 23.24%. Prevalence was 25.7% in boys versus 12.5% in girls (P<0.05). The prevalence of the peripheral zone was 29.2%, and that of the urban zone, Schistosoma haematobium infection, was (11.5%) P<0.05. The difference in prevalence is statically significant. The group prevalence of subjects in the (5-10) age group was (19.2%) and that of the (11-15) age group was 26.8%. The difference was not statically significant (P>0.05). Of the infested pupils, 100% were treated with 40 mg/kg praziquantel. Bilharzia is present in this city, and intensifying health education campaigns among the population would help delay the onset of this parasitosis and enable the authorities to set up a national helminthiasis control program.
Keywords
Prevalence; Urinary schistosomiasis; Peri-urban area; Urban area
Introduction
Schistosomiasis or bilharzia is a water-dependent parasitic disease prevalent worldwide, especially in sub-Saharan Africa [1]. In 2017, WHO estimated that 250 million people were affected by the disease in 52 countries worldwide, and 800,000 deaths were recorded annually [2]. Second only to malaria in tropical and subtropical regions, schistosomiasis is a real public health problem in endemic countries, including 42 in Africa [2-4]. Some studies have shown that nearly 800 million people worldwide are exposed to the disease [5]. Schistosomiasis has been associated with growth failure, malnutrition, cognitive impairment and reduced work capacity, and is transmitted by freshwater molluscs as intermediate hosts [6,7]. Many studies confirm that the distribution of schistosomiasis is strongly linked to the physical environment, such as hydro- agricultural developments, which create a context favorable to the development of this disease [8,9]. The highest prevalence rates are recorded in tropical and subtropical regions, among communities living along rivers [10-13].
To date, no national survey has been carried out in Chad to assess the distribution of urogenital bilharziasis throughout the country, and even less so in Ouaddaï province. In other regions, a few studies have been carried out on this subject; for example, urinary schistosomiasis prevalence rates of 26.4%, 24.9% and 39.2% have been found respectively in N’Djamena in the Sahelian zone, in the Torrock and Rong population in the Sahelo-Sudanian zone, in the population living around the Ounianga lakes in the Sahara [14-16]. In addition, recently 55% haematuria rate was reported due to Schistosoma haematobium infection in school-age children in the Salamat region of Sudanian [17].
The aim of this study is to determine the prevalence of urinary schistosomiasis in urban and peri-urban areas in the commune of Abeche, which has not previously been documented in the transmission of this disease, and to establish the main risk factors associated with this transmission.
Material and Methods
Material
Study area: This study was conducted in the commune of Abeche, located between the 10th and 15th degrees North latitude and the 13th and 24th degrees East longitude in eastern Chad (Figure 1). The annual rainfall in this area ranges from 200 mm to 800 mm [18]. There are two seasons, the dry season runs from October to June and the rainy season runs from July to September [19]. Inhabitants of this area were around 178896 [20]. Among the 28 areas of Abéche health district, 20 are urban and 8 are suburban [21]. Many Urinary Schistosomiasis cases were reported in Abéché health district (Pers. Comm). However, no preventive chemotherapy was implemented yet in this area [22]. About Eleven schools were chosen for this study, five suburban primary schools and six urban schools (four primary schools and two secondary schools) (Table 1). This cross- sectional prospective study was conducted from December 2020 to May 2022.
| Schools locations | Schools name | Dates of collection |
|---|---|---|
| Suburban primary schools | Renaissance | 16 December 2020, 24 and 25 May 2022 |
| Kinine | 17 December 2020 | |
| Djabaye | 11 December 2020 and 22 November 2021 | |
| Kamina | 23 December 2020 | |
| Djatinié | 02 December 2021 | |
| Urban primary schools | Foyer | 02 December 2021 |
| Gendarmerie | 21 December 2020 | |
| Amitié | 09 December 2020 | |
| Abouna Adam | 15 December 2020 | |
| Urban secondary schools | Ben Rachid | 23 December 2021 |
| Boustane | 25 December 2021 |
Table 1: Schools locations in Abéché commune.
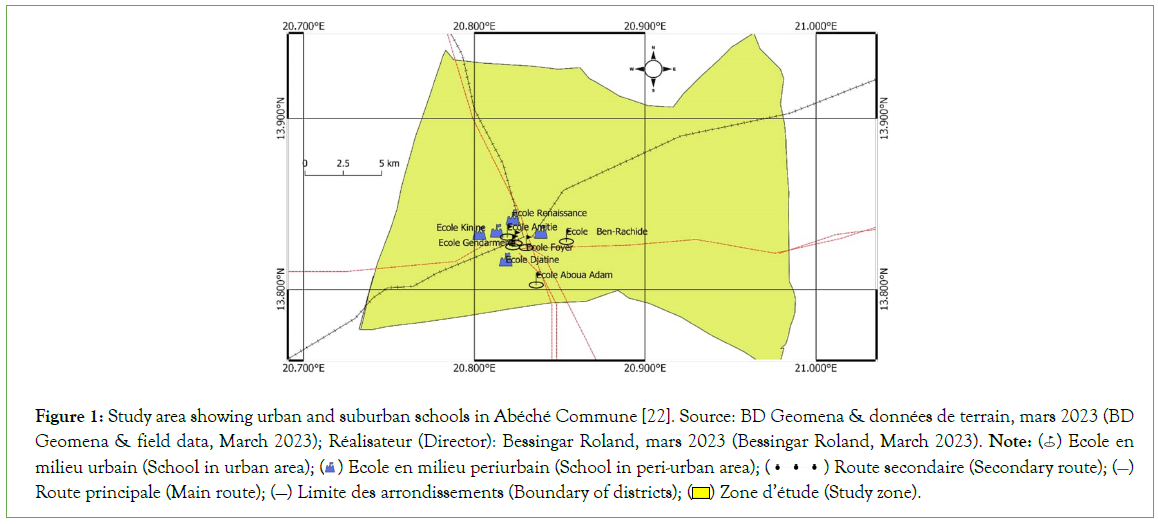
Figure 1: Study area showing urban and suburban schools in Abéché Commune [22]. Source: BD Geomena & données de terrain, mars 2023 (BD Geomena & field data, March 2023); Réalisateur (Director): Bessingar Roland, mars 2023 (Bessingar Roland, March 2023). Note:  Ecole en milieu urbain (School in urban area);
Ecole en milieu urbain (School in urban area);  Ecole en milieu periurbain (School in peri-urban area);
Ecole en milieu periurbain (School in peri-urban area);  Route secondaire (Secondary route);
Route secondaire (Secondary route);  Route principale (Main route); (—) Limite des arrondissements (Boundary of districts);
Route principale (Main route); (—) Limite des arrondissements (Boundary of districts);  Zone d’étude (Study zone).
Zone d’étude (Study zone).
Ethics statement: Before data collection, ethical clearance that approving this protocol study was obtained from the National Bioethics Committee of Chad, under N°004PT/PM/MESRI/ SE/SG/CNBT/SG/2023. Sampling survey authorizations were obtained from the health Sub-division delegates of Ouaddaï and the National Education and Civic Promotion delegates of Ouaddaï. Parasitology experiences undertaken in the Laboratory of Abeche Sub-division hospital, received the authorization of the related Director. School children, teachers and parents were sensitized about the purpose of the study and parental consent was obtained.
Study population: School children are the most affected and exposed population to urinary schistosomiasis in Sub-Saharan African [12]. Male or female school children, between 5 years and 15 years old who have been resident for at least six months in study areas, have obtained parental consent and have not received any chemotherapy treatment 3 months before were included in this study.
In each school, targeted school children were randomly selected, then submitted to oral questions to assess their exposition to associated risks factors of the diseases. The questions asked include the gender, the education levels, the presence or not of latrines at home, the access or not to drinking water, whether or not their habitat were close to the river and whether or not they use river for swimming, washing plates or doing laundry. Thereafter, each pupil received 60 mL of sterile transparent container with a cap, labeled with a unique number. The pupils were carefully instructed on how to dispense mid-stream urine into the sample container [23]. All the urine samples were collected and conserved at around -20°C with in isothermal cooler until use.
Methods
Parasitological analysis: In the Laboratory, visual aspect of each urine sample was exanimated to detect the presence or absence of macro haematuria. Thereafter, eggs of Schistosoma haematobium were detected using eggs concentration technique [24]. Briefly, 10 mL of each urine sample was centrifuged at 1,000 rpm for 10 min. The different pellets obtained were separately putting between slide and coverslip, and then observed with a microscope at 10X then 40X. The pupils that were positive to Urinary schistosomiasis were immediately received Praziquantel (PZQ) as recommended [23].
Statistical analysis: Data on oral questionnaires and parasitological analysis were entered into Microsoft Excel and loaded into SPSS version 20.0 (IBM). The Pearson Chi-Square (χ2) test was used to compare differences in prevalence between age groups, gender, and school location and associated risk factors. Statistical significance was set at p<0.05.
Results
Data on study population
A total of 723 pupils were included in this study, 243 (33.6%) were from urban schools and 480 (66.4%) from suburban schools. Of the 723 pupils included, 136 (18.8%) were girls and 587 (81.2%) were boys. A significant difference was obtained between male and female of urban schools (P<0.001) and suburban schools (P<0.001) (Table 2).
| Schools locations | Schools names | Ni | Gender | P-value | |
|---|---|---|---|---|---|
| Girls | Boy | ||||
| N1 (%) | N2 (%) | ||||
| Suburban areas | Kinine | 47 | 15 (31.9)b | 32 (68.1)a | 0.0004 |
| Kamina | 44 | 3 (6.8)b | 41 (93.2)a | 0.0001 | |
| Renaissance | 162 | 32 (19.8)b | 130 (80.2)a | 0.0001 | |
| Djatinié | 81 | 14 (17.3)b | 67 (82.7)a | 0.0001 | |
| Djabaye | 146 | 18 (12.3)b | 128 (87.7)a | 0.0001 | |
| Subtotal 1 | 5 Schools | 480 | 82 (17.1)b | 398 (82.9)a | 0.0001 |
| Urban areas | Foyer | 30 | 8 (26.7)b | 22 (73.3)a | 0.0007 |
| Abouna-Ad | 33 | 3 (9.1)b | 30 (90.9)a | 0.0001 | |
| Amitié | 27 | 2 (9.1)b | 25 (92.6)a | 0.0001 | |
| Ben-Rachid | 41 | 14 (34.1)b | 27 (65.9)a | 0.007 | |
| Boustane | 57 | 18 (31.6)b | 39 (68.4)a | 0.0002 | |
| Gendarmerie | 55 | 9 (16.4)b | 46 (83.6)a | 0.0001 | |
| Subtotal 2 | 6 Schools | 243 | 54 (22.2)b | 189 (77.8)a | 0.0001 |
| Total (N) | 11 Schools | 723 | 136 (18.8)b | 587 (81.2)a | 0.0001 |
Note: Ni-Total number of children in schools i; N1-Number of girls; N2-Number of boys; a and b difference is statically significant, a being the highest value and b the lowest value.
Table 2: Distribution of schoolchildren in urban and suburban schools of Abéché Commune.
Prevalence and associated risk factors of urinary schistosomiasis
Of the 723 analyzed urines, 168 (23.23%) were containing at least one egg of Schistosoma haematobium, 28 (11.52%) urine infections in pupils of Urban schools and 140 (29.2%) urine infections in pupils of Suburban schools (Table 3). Among the 168 infected urines, 17 (12.5%) were belong to girls and 151 (25.7%) were belong to girls; 66 (19.2%) were aged between 5 years and 10 years old and 102 (26.8%) were aged between 11 years to 15 years old. A significant difference in the urine infection rate was found between the schools locations (p<0.0001), genders (p<0.0001) and age groups (p=0.0167) (Table 3). Among school children living in urban areas, urine infection rate were similar between genders (P=0.2) and age groups (P=0.05). However, among school children living in suburban areas, a significant difference were found in urine infection rate, between genders (p=0.003) and age groups (p=0.002) (Table 3).
| Schools locations features | Genders | Numbers of pupils examined (Ne) | Number of pupils parasitized Np (%) | P-value |
|---|---|---|---|---|
| Urban |
Girls | 54 | 4 (7.41) | 0.2 |
| Boys | 189 | 24 (12.70) | ||
| Subtotal | 243 | 28 (11.52) | ||
| Age ranges | Ne | Np (%) | ||
| (5-10) | 84 | 5 (5.95) | 0.05 | |
| (11-15) | 159 | 23 (14.47) | ||
| Subtotal | 243 | 28 (11.52) | ||
| Suburban | Genders | Ne | Np (%) | |
| Girls | 82 | 13(15.85) | 0.003 | |
| Boys | 398 | 127 (31.91) | ||
| Subtotal | 480 | 140 (29.16) | ||
| Age ranges | Ne | Np (%) | ||
| (5-10) | 259 | 61(23.55) | 0.002 | |
| (11-15) | 221 | 79 (35.75) | ||
| Subtotal | 480 | 140 (29.16) | ||
| Setting/Modality | Genders | Ne | Np (%) | |
| Girls | 136 | 17 (12.50)b | 0.0001 | |
| Boys | 587 | 151 (25.72)a | ||
| Total | 723 | 168 (23.23) | ||
| Age ranges | Ne | Np (%) | ||
| (5-10) | 343 | 66 (19.24)b | 0.0167 | |
| (11-15) | 380 | 102(26.84)a | ||
| Schools locations | Ne | Np (%) | ||
| Suburban | 480 | 140 (29.16)a | ||
| Urban | 243 | 28 (11.52)b | ||
| Total | 723 | 168 (23.23) | ||
Note: Ne-Number of pupils examined, Np-Number of parasitized individuals, (%)-Percentage of infection rate, the different letters a and b in line indicate that the difference is statically significant, a being the highest value and b the lowest value.
Table 3: Schistosoma haematobium egg excretion rates by age group and gender age groups and genders: intra-living environment analysis.
Among the 168 infected pupils, 147 (23.6%) were in primary schools and 21 (21.2%) in secondary schools. In primary schools, the number of infected pupils varied from 2 (3.9%) to 48 (33.3%); the most infected pupils were in Class 5 and the less infected in Class 1. A significant difference in urine infections rate was found between pupils of primary classes (p<0.0001). In secondary schools, the number of infected pupils varied from 4 (11.1%) to 5 (29.4%); the most infected pupils were in From 5 and the less infected in From 1. Urine infection rate was similar between pupils of secondary classes (p=0.2) (Table 4).
| Education levels | Number of pupils examined | Number of pupils parasitized (%) | P-value | |
|---|---|---|---|---|
| Primary | Class 1 | 51 | 2 (3.9)a | <0.0001 |
| Class 2 | 76 | 5 (6,.6)c | ||
| Class 3 | 71 | 16 (22.5)ab | ||
| Class 4 | 111 | 22 (19.8)b | ||
| Class 5 | 144 | 48 (33.3)a | ||
| Class 6 | 171 | 54 (31.6)a | ||
| Subtotal | Class 1 to 6 | 624 | 147 (23.6) | |
| Secondary | From 1 | 36 | 4 (11.1) | 0.2 |
| From 2 | 20 | 6 (30.0) | ||
| From 3 | 26 | 6 (23.1) | ||
| From 4 | 17 | 5 (29.4) | ||
| Subtotal | From 1 to 4 | 99 | 21 (21.4) | |
| Total | 10 | 723 | 168 (23.24) | |
Note: (%)-Percentage, a and b in line indicate that the difference is statically significant, a being the highest value and b the lowest value.
Table 4: Urine Infection rate of Schistosoma haematobium eggs in different education levels.
Among the 723 school children questioned, 706 (97.6%) said that they had latrines at home, 484 (66.94%) said that they had access to drinking water, 712 (98.47%) said that they bathed in the river, 713 (98.61%) said that they doing laundering or washing plates in the river and 459 (63.48%) said that they living close to the river. The infection rate were similar between school children who said that they had latrines at home (23.65%) and those who said that they did not have latrines at home (5.88%) (P=0.08). The infection rate were similar between school children who said that they had access to drinking water (24.79%) and those who said that they did not have access to drinking water (20.08%) (P=0.16). The infection rate were similar between school children who said that they doing laundering or washing plates in the river (23.42%) and those who said that they did not doing laundering or washing plates in the river (10%) (P=0.47). The rates of infected urines differed significantly between school children who said that they bathed in the river (22.61%) and those who said that they did not bathing in the river (63.6%). The rates of infected urines differed significantly between school children who said that they living close to the river (32.68%) and those who said that they did not living close to the river (6.82%) (Table 5).
| Settings | Children’s respond | Number of students recorded (%) | Number of students parasitized (%) | P-value |
|---|---|---|---|---|
| Latrines in the home | Yes | 706 (97.6) | 167 (23.65) | 0.08 |
| No | 17 (2.35) | 1 (5.88) | ||
| Total | 723 (100) | 168 (23.23) | ||
| Access to drinking water | Yes | 484 (66.94) | 120 (24.79) | 0.16 |
| No | 239 (33.05) | 48 (20.08) | ||
| Total | 723 (100) | 168 (23.23) | ||
| Swimming in the marigots | Yes | 712 (98.47) | 161 (22.61) | 0.006 |
| No | 11 (1.52) | 7(63.64) | ||
| Total | 723 (100) | 168 (23.23) | ||
| Laundry, dishes | Yes | 713 (98.61) | 167 (23.42) | 0.47 |
| No | 10 (1.38) | 1(10) | ||
| Total | 723 (100) | 168 (23.23) | ||
| Neighbouring water courses | Yes | 459 (63.48) | 150 (32.68) | 0.0001 |
| No | 264 (36.51) | 18 (6.82) | ||
| Total | 723 (100) | 168(23.23) | ||
Note: (%)-Percentage of infection rate.
Table 5: Main risk factors for urinary schistosomiasis.
The study also showed that infestation rates varied according to gender, age group and living environment (Table 3). Indeed, boys were more often infested than girls (25.72% vs. 12.50%) were, younger school children less parasitized than their elders (19.24% vs. 26.84%) were, and peri-urban dwellers more infested than urban dwellers (29.16% vs. 11.52%). Taking into account the living environment, it appears that the differences in prevalence of urinary bilharzias are noted above between genders on the one hand and age groups on the other, now only concern the suburban area (Table 3).
Although almost all students (706 or 97.65%) reported having home latrines, a good proportion (23.65%) tested positive for parasites. This infection rate is only relatively (p=0.08) higher than that of pupils parasitized by S. haematobium but without a home latrine, i.e. 5.88%; thus the presence of a latrine does not seem to reduce S. haematobium infestation. Children living close to a stream (459 pupils, 63.49%) were significantly (p=0.0001) more likely to be carriers of S. haematobium eggs (32.68%) than those living further away, 264 (6.82%). Almost all school children 712 (98.48%) said they bathed in marshes; of these, 161 (22.61%) eliminated S. haematobium eggs. Paradoxically, of the 11 (1.52%) pupils who said they did not bathe in the marshes, 7 (63.64%) were infested with S. haematobium. Having drinking water at home didn't seem to reduce the prevalence of S. haematobium schistosomiasis in school children either, since among those who said they had drinking water, 24.79% had eliminated eggs of this parasite; a proportion statistically equal to 20.08% was that of children affected but without a drinking water supply. Similarly, the proportion of children (23.42%) reporting that they washed their clothes in ponds and eliminated parasite eggs was not statically different (p=0.47%) from that of children (10%) reporting that they did not use this practice but still carried S. haematobium (Table 5).
Discussion
The aim of this study was to determine the prevalence of urinary schistosomiasis in peri-urban and urban school children in the commune of Abéché, in the Sahelian zone, and to identify the main risk factors associated with transmission of this parasitosis. In the course of this work, 168 of the 723 participants sampled were infested with Schistosoma haematobium, giving an overall prevalence of 23.24%. This prevalence is comparable to the 26.85% obtained in N'Djaména (also in the Sahelian zone), Chad by Hamit et al. [14]. On the other hand, it is lower than the 55% obtained by Vislosky et al. in the Salamat province of Chad [17]. This difference in prevalence could be explained by the geographical position of Salamat. Indeed, Salamat province is located in the Sudanian zone, and is therefore much more watered; it has both perennial and temporary watercourses. Compared with other countries, the prevalence of 23.24% is lower than those obtained in Cameroon in the humid tropical southwest by Green et al. and Sumbele et al., i.e. 31.5% and 32.6% respectively [25,26]. Overall, boys were significantly more infested (27.4%) than girls (12.5%); this difference can only be observed in suburban areas. This finding, also made by Sengor, Dankoni et al. and Hamit et al. respectively in rural Senegal, Kékem (West Cameroon) and N'Djaména (Chad), is contrary to that made by Tagajdid et al. in Morocco and in Benin by (30) Ibikounlé et al.; the latter authors noted that girls and boys were infested in the same way, i.e. with no significant difference [14,27-30]. In the present work, this result indicates that peri-urban communities reside in environments heavily contaminated by S. haematobium. Indeed, given the growing urbanization of the Abéché commune, sanitation work and improved living conditions would reduce the rate of schistosomiasis infestation [31].
The low prevalence of urinary schistosomiasis among girls may be linked to local customs, which keep girls more occupied with domestic activities, unlike boys, who have more free time and engage in swimming and other extracurricular activities, leading them to frequent marigots and other waterholes. What's more, feminine intimacy is said to discourage girls from bathing in the presence of boys [32]. The absence of a statistically significant link between the presence of urinary schistosomiasis and the presence of drinking water in the home, on the one hand, and between prevalence and the presence of latrines, on the other, is essentially due to the failure of school-age children to observe basic hygiene measures [13,14]. This observation corroborates the results of KiKi-barro et al. in Ivory Coast [33]. In addition, proximity to watercourses and bathing in marigots were found to be risk factors for schistosomiasis. This observation corroborates that of Adoubryn et al. in Mali [34]. In order to combat this disease effectively, we agree with Oyono et al. that chemoprevention campaigns should be organized on a regular basis, following a well-defined timetable by the Ministry of Public Health [35]. It would also be important to set up a national program to combat schistosomiasis and intestinal helminthiasis.
Limitations of the study
The examination must be repeated on 3 urine samples spaced several days apart, as the excretion of parasite eggs is very often intermittent. We worked only on a single sample. Non-application of internal quality control for slide reading data; 24 hour urine: all 24-hour urine must be collected in a clean bottle and processed as soon as received, within 20 min.
Conclusion
The present study reveals that urinary schistosomiasis is well established in Abeche and, in particular, does a real public health problem in Chad in general, deserve greater attention. Its distribution is uneven between urban and peri-urban environments. The infestation of school children is closely linked to the hygienic and environmental conditions favorable to the development of intermediate hosts, and to the dissemination of Schistosoma haematobium eggs. The fight against this disease calls on the public authorities to set up a national program to combat schistosomiasis, whose mission will include raising public awareness, organizing ongoing screening surveys and treatment campaigns, and developing drinking water supply points.
Acknowledgment
The authors are grateful to the academic authorities of the University of Yaoundé, the Ministries of Public Health and National Education of Chad, as well as the provincial hospital of Abeche, provincial education delegation, school principals, parents and pupils for their collaboration throughout this study. This work is based on research supported in part by technical and material contributions from members of the Laboratory of Parasitology and Ecology of the University of Yaoundé and the Laboratory of Parasitology and Mycology of the Faculty of Human Health Sciences of the University of N'Djamena.
Conflict of Interest
There is no conflict of interest among authors.
References
- OMS. Aide-mémoire N 115. 2016.
- Richter J, Hatz C, Campagne G, Bergquist NR, Jenkins JM. Ultrasound in schistosomiasis: A practical guide to the standard use of ultrasonography for assessment of schistosomiasis-related morbidity: Second international workshop, October 22-26 1996, Niamey, Niger. World Health Organization. 2000.
- Traoré M, Landouré A, Diarra A, Kanté B, Sacko M, Coulibaly G, et al. Geographic distribution and epidemiology of urinary schistosomiasis in Mali: Implications for a control program. Mali Med. 2007;22(3):22-28.
[Google Scholar] [PubMed]
- Clements AC, Garba A, Sacko M, Touré S, Dembelé R, Landouré A, et al. Mapping the probability of schistosomiasis and associated uncertainty, West Africa. Emerg Infect Dis. 2008;14(10):1629-1632.
[Crossref] [Google Scholar] [PubMed]
- Aubry P, Gaüzère BA. Schistosomoses ou bilharzioses. Médecine Trop. 2018;8(7):1-8.
- Zhou H, Ohtsuka R, He Y, Yuan L, Yamauchi T, Sleigh AC. Impact of parasitic infections and dietary intake on child growth in the schistosomiasis-endemic Dongting Lake Region, China. Am J Trop Med Hyg. 2005;72(5):534-539.
[Crossref] [Google Scholar] [PubMed]
- King CH. Parasites and poverty: The case of schistosomiasis. Acta Trop. 2010;113(2):95-104.
[Crossref] [Google Scholar] [PubMed]
- Molyneux DH, Hotez PJ, Fenwick A. “Rapid-impact interventions”: How a policy of integrated control for Africa's neglected tropical diseases could benefit the poor. PLoS Med. 2005;2(11):e336.
[Crossref] [Google Scholar] [PubMed]
- Steinmann P, Keiser J, Bos R, Tanner M, Utzinger J. Schistosomiasis and water resources development: Systematic review, meta-analysis, and estimates of people at risk. Lancet Infect Dis. 2006;6(7):411-425.
[Crossref] [Google Scholar] [PubMed]
- de la Santé OM. Agir pour réduire l'impact mondial des maladies tropicales négligées: Premier rapport de l'OMS sur les maladies tropicales négligées. 2011:172-173.
- Alio HM, Tidjani A, Otchom BB, Tidjani MT, Felix BB. An epidemiological assessment of the infectious forms of intestinal helminths in school children from Chad. J Biol Life Sci. 2013;4:341-361.
- Bintou LY, Sodio B, Sacko M. Persistance de la schistosomiase urinaire en zones endémiques soumises aux traitements de masse répétés au Mali. Int J Biol Chem Sci. 2019;13(1):369-381.
- Félix BB, Alio HM, Gaël OM, Jacques N, Samafou K. Intestinal Helminthiases among school children in the Sahelian and Sudanian Zones of Chad: Prevalence and risk factors. Int J Trop Dis Health. 2022;43(21):15-26.
- Hamit MA, Fombotioh N, Issa RA, Samafou S. Epidemiological profile of urinary schistosomiasis in three primary schools in the city of N’Djamena (Chad). European J Biomed Pharm Sci. 2020;7:242-246.
- Lalaye D, de Bruijn ME, de Jong TP. Impact of a mobile health system on the suppression of Schistosoma haematobium in Chad. Am J Trop Med Hyg. 2021;105(4):1104-1108.
[Crossref] [Google Scholar] [PubMed]
- Moser W, Batil AA, Ott R, Abderamane M, Clements R, Wampfler R, et al. High prevalence of urinary schistosomiasis in a desert population: Results from an exploratory study around the Ounianga lakes in Chad. Infect Dis Poverty. 2022;11:1-5.
[Crossref] [Google Scholar] [PubMed]
- Visclosky T, Hashikawa A, Kroner E. Discovery of a hidden schistosomiasis endemic in the Salamat region of Chad, Africa. Glob Health Sci Pract. 2022;10(1):e2000703.
[Crossref] [Google Scholar] [PubMed]
- Yamingue B, Ngaressem GM. Tchotsoua M. Acteurs urbains et gestion de l’eaudans la ville de Sarh (sud du Tchad). Syllabus Rev. 2015;6(1):69-98.
- Dombor DD, Djebe M. Problématique de l'accès à l'eau potable dans la ville d’Abéché au Tchad. Annales de l’Université de Moundou. 2019;5(2):93-119.
- INSEED. Le Deuxième Recensement Général De La Population Et De L’habitat (RGPH2) de 2009. Institut Nationale de la Statistique des Etudes Economiques et Démographique. 2010;235.
- Plan national de développement sanitaire 2018-2021. Ministère de la Santé Publique. 2018:135.
- Bessingar R. Carte de la commune d’Abéché. 2023.
- World Health Organization. Schistosomiase et géohelminthiases: Prévention et lutte: Rapport d'un Comité d'experts de l'OMS. Organisation mondiale de la Santé. 2004.
- Chelsea M, William AP Jr. Schistosomiase. Actualités. 2021.
- Green AE, Anchang-Kimbi JK, Wepnje GB, Ndassi VD, Kimbi HK. Distribution and factors associated with urogenital schistosomiasis in the Tiko Health District, a semi-urban setting, South West region, Cameroon. Infect Dis Poverty. 2021;10(1):1-5.
[Crossref] [Google Scholar] [PubMed]
- Sumbele IU, Tabi DB, Teh RN, Njunda AL. Urogenital schistosomiasis burden in school-aged children in Tiko, Cameroon: A cross-sectional study on prevalence, intensity, knowledge and risk factors. Trop Med Health. 2021;49(1):1-75.
[Crossref] [Google Scholar] [PubMed]
- Senghor B. Prévalence et intensité d’infestation de la bilharziose uro-génitale chez les enfants d’âge scolaire à Niakhar (milieu rural sénégalais). DEA Bio Dakar: Université Cheikh Anta Diop de Dakar. 2010;2010(278):100.
- Dakoni N, Saotoing P, Tchawe R, Koé V, Ndikwé JL, Nlôga AN, et al. Epidemiological survey on schistosomiasis caused by Schistosoma haematobium and Schistosoma mansoni in primary schools in the Sub-Division of Taïbong-Dziguilao, Far-North Region Cameroon. J Applied Biosci. 2015;90:8397-8407.
- Tagajdid R, Lemkhente Z, Errami M, El Mellouki W, Lmimouni, B. Prevalence of intestinal parasitic infections in Moroccan urban primary school students. Bull Soc Pathol Exot. 2012;105(1):40-45.
[Crossref] [Google Scholar] [PubMed]
- Ibikounlé M, Satoguina J, Fachinan R, Tokplonou L, Batcho W, Kindé-Gazard D. Épidémiologie de la bilharziose urinaire et des géohelminthiases chez les jeunes scolaires des zones lacustres de la commune de So-Ava, sud-Bénin. J Appl Biosci. 2013;70:5632-5639.
- Ernould JC, Labbo R, Chippaux JP. Course of urinary schistosomiasis in Niamey, Niger. Bull Société Pathol Exot. 2003;96(3):173-177.
[Google Scholar] [PubMed]
- Njiokou E, Onguene-Onguene AR, Tchuem-Tchuente LA, Kenmogne A. Urban schistosomiasis in Cameroon: A longitudinal study of its transmission in a new site of an extension of the intestinal schistosomiasis focus in Mélen, Yaoundé. Bull Société Pathol Exot. 2004;97(1):37-40.
[Google Scholar] [PubMed]
- Kiki-Barro PCM, Kassi FK, Konate A, Angora EK, Menan E. Prevalence of intestinal helminthiasis among primary school children in San-Pedro, South-west, Cote d’Ivoir. Revue International des Sciences Médicales. 2017;19(3):173-178.
- Adoubryn KD, Ouhon J, Yapo CG, Assoumou EY, Ago KM, Assoumou A. Epidemiological profile of the schistosomiasis in school children in the Agneby Region (south-east of Côte-d'Ivoire). Bull Société Pathol Exot. 2006;99(1):28-31.
[Google Scholar] [PubMed]
- Oyono MG, Lehman LG, Bilong BCF. Multiparasitism among school children of Akonolinga, Nyong and Mfoumou Division, Centre Region of Cameroon. J Biol Sci. 2019;10(2):90-105.
Citation: Abdel-Aziz MH, Alio HM, Samafou K, Adam AM, Felix BBC (2024) Preliminary Data on the Prevalence and Associated Risk Factors of Urinary Schistosomiasis among School Children in Abeche Commune, Eastern Chad. J Bacteriol Parasitol. 15:507.
Copyright: © 2024 Abdel-Aziz MH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.