Indexed In
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2019) Volume 3, Issue 1
Predictors of Timely Initiation of Breast-Feeding among Rural Women using Case Study Design in Dawuro Zone, Southern Ethiopia in 2018
Teshome Negash*Received: 29-Mar-2019 Published: 17-Apr-2019
Abstract
Background: Globally rate of early initiation (within the first hour) of breast-feeding was below 40%, in developing counties 39% and in Africa 47%. Breast-feeding within the first hour of life was a potential mechanism for health promotion for neonate. From a public health perspective, it was important that newborns be breastfed at birth and It was internationally recommended that timely initiation and promotion of exclusive breast-feeding as the optimal method of infant feeding for the first six months of life.
Objective: It was assessed Predictors of timely initiation of breast feeding among rural woman in Dawuro Zone.
Methods: A community-based case study design with both quantitative and qualitative method was conducted in Dawuro Zone, Southern Ethiopia from January up to August 2018. Sample size was 598 rural women, and which was calculated using single population proportion formula. Interviewer administered structured questionnaire for quantitative and four FGDS for qualitative study were used to collect data. Frequency table and cross tabulation was done. AOR and OR with 95% CI were considered for statistical significance. Bivariate analysis was used to determine presence of crude association. Multivariate logistic regression model was employed to control confounding.
Results: More than sixty percent of the women were not initiated breastfeeding within the first one hour after delivery. Early initiation of breastfeeding was associated with many material and neonatal factor in addition to belief of a community.
Conclusion: In order to advance the rates of breastfeeding within the first hour of life, health care professionals must encourage the factors favouring TIBF practice such as ANC guidance regarding the advantages of breastfeeding, health education for women during family planning period and giving care up to full term birth, counselling on rue of delivery, and stimulate this practice in vulnerable situations such as women with cesarean section and preterm birth. In other hand the health development army must promote the importance of timely initiation of breastfeeding for neonate growth and developments at each one to five network.
Recommendation: Ministry of health should strength health promotion program on breast feeding for rural women. Regional health bureau should give training for health developmental army in rural set up to enhance promotion of breast-feeding at community level.
Keywords
Rural woman; Infant pair; Timely initiation of breast-feeding
Introduction
Globally prevalence of early initiation (within the first hour initiation) of breast-feeding was below 40%, and in Africa it was 47%. The prevalence of timely initiation of breast-feeding in some developing countries other than Ethiopia was documented as in Ghana (41%), Sudan (54.2%), Zambia; (70%), Jordan (49.5%), North Jordan (86.6%), Nepal (72.2%), Bolivia; (74%). In Ethiopia, two third of babies do not receive breast-feeding within the first one hour after delivery and breast-feeding within the first one hour of life was a potential mechanism for health promotion [1]. From a public health perspective, it was important that newborns be breastfed at birth and it was internationally recommended that timely initiation and promotion of exclusive breast-feeding as the optimal method of infant feeding for the first six months of life [2,3].
Timely initiation of breast-feeding is the easiest, cost effective and lifesaving interventions for the health of the new-born. About Twenty two percent of neonatal deaths could be prevented, if all infants are put to the breast within the first hour of birth [4].
Breast-feeding was very common in Ethiopia, about 98% of children ever breastfed and Ethiopian government had developed infant and young child feeding guidelines giving appropriate emphasis to key messages on timely initiation of breast feeding in [5,6]. Study done in rural Ethiopia in 2010 the prevalence of timely initiation of breast-feeding was about 52% [7].
Nearly half of new born children in Ethiopia exposed for easily preventable neonatal death and morbidity even if breast feeding was universal due to low prevalence of timely initiation of breast feeding. Exclusive breast-feeding preceded by timely initiation and appropriate complementary feeding practices were universally accepted as essential elements for the satisfactory growth and development of infants and for prevention of childhood illness [8].
Statement of the problem
In Africa decrement of child death was a burning issue which was thematized in MDG at the September 2010 MDG Summit, world leaders put forward an ambitious action plan a roadmap outlining what is needed to meet the goals by the agreed deadline of 2015. Thus, one of the strategies adopted to decrease children death was timely initiation of breast-feeding, and ANC follow up in health institution. Early breast-feedings enhance growth and development of immunity and then prevent neonate from communicable disease. Investing on neonate was equivalent to investing on generation but there were so many factors which affect neonatal health. Dawuro zone has multi-diversified cultures from that, in rural set up of Dawuro Zone the woman has cultural and social influence on breast-feeding of the child. The significance of this study was it identified the potential predictor of timely initiation of breast feeding and evaluated the prevalence of breast-feeding initiation within the first hour of life. And also, it was provided important information for program planer and decision maker to focus on the key area of intervention which helps to achieve the millennium development goal. Promoting early initiation of breastfeeding within 1 hour of birth and exclusive breastfeeding up to 6 months of age in early infancy was regarded as crucial components of child survival strategies that could prevent up to 13% of deaths among children under 5 years of age [9]. The finding was easiest to implement in resource scarce area like Dawuro Zone which was west Southern part of Ethiopia (Figure 1).

Figure 1: Schematic presentation of conceptual framework for timely initiation of breast-feeding (Tefera Belachew, BMC Public Health 2011, 11:217).
Objective of the Study
General objective of the study: It was assessed predictors of timely initiation of breast feeding in Dawuro Zone among rural women. Specific objective of the study: It was identified socio demographic effects on timely initiation of breast feeding in Dawuro Zone among rural women.
It was identified maternal and neonatal factors which affected timely initiation of breast feeding in Dawuro Zone among rural women. It was assessed factor affecting exclusive breast feeding in Dawuro Zone among rural women. It was assessed timely initiation of supplementary feeding in Dawuro Zone among rural women.
Materials and Methods
Study area
The study was conducted in selected wereda of Dawuro Zone. Dawuro Zone was one of the seventy Zones in Southern Ethiopia, which was located South West of Ethiopia 515 km apart from Addis Ababa which was capital City of Ethiopia, 275 km apart from Hawassa which was regional City of SNNPR but now the counsel of Dawuro people decided to be Dawuro regional state in 2019 and requested for federal government to announce its state.
The Dawuro Zone had ten Wereda and one City administration. Based on central statistics agency report of 2007, the Zonal projected total population in 2018/19 was 950218. From these females were 49% (465,606) and males were 51% (484,611). Approximately 91% of the populations are rural dwellers and 9% of the populations are urban dwellers 85% of their income source is agriculture and the remains 15% is trade and others. The Zone has three agro ecologies. The potential health coverage of the Dawuro Zone is 92%. In the Zone there are one General hospital, one primary hospital, 23 health centre and 177 health posts. All rural weredas found in the Zone were included in the study to represent the rural population. For logistic and cost reasons two wereda namely Mareka and Gena-Bosa weredas were randomly selected by a lottery method. Using simple random sampling, twenty peasant associations (Ten from Mareka and Ten from Gena-Bosa) were selected [10]. Mareka Wereda was one of the Wereda in Dawuro Zone in which Zonal city was established namely Tarcha and the Wereda city was 17 km apart from Zonal City namely Waka. The Wereda was administratively divided into 37 kebeles. The potential health coverage of the Wereda was 85%. There are 4 health center, 33 health post, one YFS center, 70 primary schools and 6 secondary schools and 2 preparatory schools. Based on central statistics agency report of 2007, the Mareka wereda projected total population in 2018/19 is 200341. From these population females are 48% (96,163) and males are 52% (104,177) from total population. Gena-Bosa Wereda was one of the Wereda in Dawuro Zone and the Wereda city was 40 km apart from Zonal City namely Karawo. The Wereda was administratively divided into 36 kebeles. The potential health coverage of the Wereda was 75%. There were 4 health centres, 38 health posts. Based on central statistics agency report of 2007, the Gena-Bosa wereda projected total population in 2018/19 was 150332. From these population females are 49.8% (73,662) and males are 50.2% (76,669) in the district. Ninety percent of the both Wereda populations were rural dwellers, and the remaining ten percent of the both Wereda populations are urban dwellers. Approximately 89% of their income source was agriculture and the remain 11% of their income source was from trade and others. Both wereda covered an area of 93240 hectares from these 31.77% was high land, 40% was mid land, and the remaining 28.23% was low land. Both districts were rich in rivers and mountains of different shapes and size.
Study design and period
Community based case study design was conducted from January to August 2018 by using both quantitative and qualitative methods for triangulation. Cases were woman- infant pair who initiated breast feeding within one hour of delivery.
Source population
All women of child bearing age (15-49 years) in Dawuro Zone and study population was all women with infant (<1 year of age) found in Mareka and Gena-Bosa districts during the study period. Study subject was woman with infant found in selected kebele of Mareka and Gena-Bosa district in January up to August 2018 fiscal year. Inclusion and exclusion criteria for quantitative study All rural women infant pairs found in selected Kebele of Mareka and Gena-Bosa District who were not severely and mental ill were included in the study. But all rural women infant pairs who were severely ill and not found in the selected Kebele and not found in selected house holed during interview of the Mareka and Gena- Boas District were excluded from the study.
Sample size determination for quantitative study
Sample size was calculated using a formula for single population proportion, assuming and EPI-INFO software by using the following assumption. Since there was no study in Ethiopia on initiation of breast-feeding within one hour delivery up to knowledge of investigator but there was study conducted in Nigeria and the proportion of woman with infant initiate breast-feeding within one hour of delivery were 23% therefore this proportion was used in this study hence it was in one of the African nation which was nearest for Ethiopia. Thus the following assumption was used to estimate maximum sample size such as; a proportion of woman with infant initiate breast-feeding within one hour after delivery level was 23%, margin of error was 5%, non-respondents rate was 10%, confidence interval level was 95%, and the design effect of two was considered to obtain sufficiently large sample size because there was steps during recruitments. Based on these assumptions the total samples size was calculated using the formula indicated below gave 598 respondents.
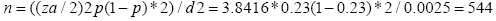
Where: n was minimum possible sample size, N was actual sample size. Z α/2 was standard score value for 95% confidence interval level of two sides normal distribution which was 1.96, and d2 was margin of error which was 5%. P was proportion of woman with infant who were imitated breast-feeding was 23%. Then minimum possible sample size was n=544. Considering 10% non-response rate total sample size was equal to n + n* 10%. Then N was equal to 544+54 =598. Hence 598 women with infants were involved in the study.
Sampling technique for quantitative study
Random sampling method was used to select 598 women with infants in Dawuro Zone. There were nine rural wereda and one town administration in Dawuro Zone. Then first we were sampled two wereda on simple random sampling and secondly, we were sampled 24 rural kebeles on simple random sampling from two wereda by lottery methods. Then the sample unity in selected kebele was house-hold with woman infant pair and after census sample unity was proportionally allocated to each selected kebele therefore the study unity in each selected kebele was 24-woman infant pair. Thirdly by giving clear orientation for data collector’s woman infant pair was selected through simple random sampling technique from the each kebele and it was checked by supervisors. Finally, the study unity was identified by using key informants on the day of the survey and those who was eligible for the study was identified and interviewed by the data collectors, if there was two study unity in one household one was selected by lottery method, and if absent the next nearest study unity was used.
Data collection technique for quantitative study
The data for the quantitative section of the study was collected by face to face interview with 5 trained data collectors for 10 days who were BSC nurse with some experience in data collection. Interviewer administered structured questionnaire was used to collect data. The instrument was adapted from web site, guide line for safe woman hood [8,11].
Sample size determination and sampling technique for qualitative study
For qualitative study participants were recruited by judgmental sampling technique. Homogeneity for participants was based on sex categories. The participants for the six FGDs were selected by using judgmental sampling technique.
Data collection technique for qualitative study
Six FGDs (three FGDs with women, three FGDs with men in the household of woman infant pair were conducted in six kebele. Each FGD comprised of ten to twelve participants. For the FGDs participants such as woman infant pair, religious leaders, health development army chairpersons; other key community resource people like TBA, witchcraft, and shaman were purposely selected from six kebeles those kebele that was not included in quantitative parts of the study. A total of 72 women and men found in Gena- Bosa and Mareka district (32 males and 40 females) were included. The age of the participants ranged from 25 to 41 years. The average time taken for each FGD was 45 minutes. All participants engaged well with the topic and responded excitedly to the questions [8,12].
Procedure for FGD
FGDs were conducted in six kebeles that were not included in quantitative parts of the study such as; Menidida kebele, Deshi kebele, Aruse kebele, Woledhane kebele, Woledahan-Gono kebele, and Mela-Galida kebele. For the six-group discussion, appropriate rapport was established before starting the focus group discussion. The respondents were assured that their responses were kept confidential. The principal investigator moderated all focus group discussion session and the two trained supervisors were assisted in note taking of all the discussions. After the focus group discussion was over, the facilitator thanks the participants for taking their time to participate on study. After each group discussion the principal investigator gave appropriate feedback. Then principal investigator and supervisors were transcribed the minutes, carry out preliminary coding of transcript and identified a consistent theme that was directly related to the objective of the study [8,13].
Variables
Dependent variable: Timely initiation of breast-feeding among rural women.
Independent variables: Back ground factor that affects Timely initiation of breast-feeding like: Age of the woman, marital status of a woman, Educational status of a woman, Educational status of a husband, Occupation of a woman, Occupation of a husband, Parity of a woman, Religion, and Ethnicity. Other factor affects TIBF like: awareness on timely initiation of breast-feeding, counselling during ANC follow up on TIBF, Gestational age, woman nutritional status, mode of delivery, Bleeding at delivery, and place of delivery, Birth weight, gender of a neonate, and practice of woman at birth for new born.
Operational definitions: Timely initiation of breast-feeding: A woman who was started breast-feeding for a neonate after expulsion of placenta up to one hour after delivery.
• High bleeding at delivery: The woman has continuous bleeding at delivery and after delivery which highly soaked packed gauze and blanket of the bed.
• Low bleeding at delivery: The woman has spot of bleed at delivery which was slightly soaked packed gauze and blanket of the bed.
• Very low birth weight: New born whose weight less than 1.5 kg or very small in body size.
• Low birth weight: New born whose weight was less than 1.5 kg up to 2.5 kg or small in body size
. • Normal birth weight: New born whose weight was 2.5 kg up to 4 kg or good in body size.
• High birth weight: New born whose weight was greater than 4 kg or big in body size.
• Gestational age: Duration of pregnancy prior to birth.
• ANC utilization: A woman who was followed at least the first and the forth ANC follow up on her pregnancy was considered as ANC utilizer, but woman didn’t follow the 4th ANC was not considered as ANC utilizer.
• Method of delivery: A woman who gave birth spontaneously through vagina was normal vaginal delivery and when she gave birth through vagina assisted by health professional it was assisted vaginal delivery. But a woman gave birth through abdominal opening of a uterus by surgical procedure was delivery by caesarean section.
• Place of delivery: A woman who gave birth at home was home delivery and who gave birth in the health institution was institutional delivery.
• Gender of a neonate: The social classification of neonate to which sex was analogous.
• Exclusive breast feeding: Giving only breast milk for a neonate four month up to six months.
• Well-nourished woman: When woman was well on looking, no pallor on palm, and upper arm circumference greater than 24 cm at postnatal period but when she has pallor on palm, and upper arm circumference less than 24 cm at postnatal period she was malnourished.
Data processing and analysis: For quantitative study, data was entered to computer using Epi data version 3.1 and exported to SPSS 16.0 software. The following descriptive variable analysis methods were considered such as; Frequency table, cross tabulation, OR and AOR with 95% CI and P value less than 0.05 were considered for statistical significance in pear-sons’ chi square test. Bivariate analysis was done to determine presence of crude statistical association between independent variables and the dependent. Variable with p-value less than 0.2 or 0.25 in bivariate analysis was considered as a candidate to be entered in multivariate logistic regression. Multivariate logistic regression model was employed to control confounding variable.
Multivariate regression was usefully to examine three or more variable at a time. The goal of multivariate regression was to arrive at the set of ‘B’ value called regression coefficient for the explanatory variables or independent variable. For qualitative study, the data was analysed by thematic approach and merged in to quantitative findings.
Data quality assurance: Data collectors & supervisors had bachelor’s degree and who were trained for four day on the objective of the study, and method of data collection, interview technique & content of questionnaire. Two supervisors were assigned to maintain data quality by coordinating the Kebele and facilitating the logistics.
Data was checked for completeness, accuracy, and consistency by supervisors & principal investigator after the data collection on daily base. Double entry was performed to assure quality of data. The questionnaire was prepared first in English and translated into Amharic retranslated in English. Pretesting of the questionnaires in the same wereda on those who was not included as the study subject was done.
Results and Discussion
Socio-demographic characteristics
A total of five hundred ninety-eight-woman infant pairs were invited to participate in the study and of which five hundred ninety were responded the interviewer administered structured questionnaires and returned completely making a response and the response rate was 98.6%. Women age ranged from 21 to 35 years (median was in the range of 26-30 years), ninety percent were married and twentysix percent were primiparous. A few (6%) of women Education level was ranged from first cycle to a diploma up first degree and the majority (94%) were illiterate. Nearly 66% of women attended at least one antenatal visit during their last pregnancy and of these only 3.5% received information on breastfeeding during their ANC visit. Sixty-two percent of woman’s gestational age ranged from 35 to 40 weeks, and thirty-four percent of woman do not know their gestational age. The most (79%) of women gave birth by SVD. Sixty-six percent of women were wish male neonate and 34% of the women were wish female neonate at their gestation period. Majority of the neonate’s birth weight ranged from 2.5 kg to 4 kg and some neonate birth weight were ranged from 1.5 kg to 2.5 kg but 0.3% of the neonate birth weight below 1.5 kg.
Awareness about timely initiation of breast feeding
Three hundred sixty women (60.2%) of the respondent were not heard about timely initiation of breast feeding after delivery. Only 39.8% of the respondents were heard about timely initiation of breast feeding and of which almost all women were initiated breast feeding within first 1hr after delivery. Fifty nine percent of women stated that first breast milk was cause abdominal cramping and not easily digestible for a neonate; thus, women were not agreed on timely initiation of breast feeding after delivery.
This was supported by the first focus group result with adult Men. In this focus group the discussants were agreed that they were not heard about TIBF, which was not given nearby in their kebele from health institution. Discussants were also agreed that TIBF had no benefit for neonate, but it had benefit for women by preventing breast distention due to first breast milk accumulation thus it cause breast pain [14].“I was discharged first breast milk by manual because it causes breast pain then this pain was radiated to all body parts of the mother and it cause abdominal cramping in neonate” (34-year, religious leader, male).
Feeding of a neonate
Sixty percent of women were giving cow milk and water for neonate within first 24 hr after delivery on other hand 43% of women gave breast milk for a neonate within first 24 hr after delivery; but majority were not timely initiated breast feeding for their neonate after delivery.
Neonatal care
Majority (79.00%) of the women declare that male neonate was prone for neonatal illness like tonsillitis, hiccup, umbilical cord infections and they need more care than female; thus there was gender biased care in the family; the most common wish of woman during ANC period was to get male neonate at birth because a male has more social value in the community in culture [15]. Which was supported by FGD “I went to church for pray in my pregnancy to get male neonate than female because male neonate gave care to me and all the family when I was aged and he was grow adult.” (30-year-old woman).
Bleeding at delivery
Fifty percent of women had bleeding for 24 hr after delivery and the amount ranges from socking two pair of gauzes up to 500 ml. Most of the woman got advice to return health institution when the bleeding extended more than 24 hr and greater than normal but there was no ambulance service to get postnatal care when the situation was most horrible in the home at far distance.
Place of delivery
Fifty six percent of woman gave birth at home which was assisted by TBA and neighbour. Majority of the rural women were belief that when woman utilized institutional delivery services, she had made a sin due to that her foetus was anomalies and her labour was unusual, thus she went to health institution to give birth. Forty four percent of rural women gave birth in health institution which was assisted by different health professional.
This was supported by FGD result with adult women. In this FGD the discussants were agreed that home delivery was very good for woman and neonate because home-made care was available easily but institutional delivery was not good for both woman and neonate because it lack home-base care in need of woman. “Home delivery is very good for women because she can discharge her first milk to prevent breast pain and to give umbilical cord care by local methods” (36-year, male).
Counselling about TIBF during ANC follow up
From two hundred ANC adherent women majority (94.7%) of the women were not counselled about timely initiation of breast feeding for their neonate during their ANC follow up and they were not aware about benefit of a cholesterol (first) breast milk for their neonate. Which was supported by in-depth interview “health professionals had no time to communicate with client in ANC clinic only they seen appointment cared and examine abdomen and ask me what you fell? Then call others to enter the clinic for examination.” (28-year-old rural woman).
Medical problem during ANC follow up
Fifty percent of rural women had medical problem during ANC follow up and they were not counseled on birth plan and TIBF, thus majority gave birth at home by SVD with some birth complication, and 7.5% of neonatal death occurred from total birth occurred at home. The Study showed that majority of rural woman had morning sickness up to chronic medical problem during their ANC follow up and the most commonly occurred (75%) medical problem was HTN range mild to severe degree of hypertension which was managed in the hospital. From total gestational hypertensive women one third of rural women (33%) women were developed sever hypertension and they were stayed in bed a week up to months in range gave birth in hospital by cesarean section.
ANC follow up
Majority (66.50%) of the rural women had no ANC follow up in their pregnancy and in addition to that from (33.50%) those who attended ANC 75% of the attendants were not completed their ANC follow up as standard of WHO guide line. From those who were not completed the ANC 95% conducted home delivery and had no initiation of breast feeding for their neonate within first one hour after delivery.
Parity of the woman
Twenty six percent of respondent was primipara and they were not initiated timely breast-feeding practice within first one hour after delivery due to there was no awareness on TIBF at ANC follow up period. Seventy three percent of rural woman were multi parous and majority of them were not aware on TIBF for their age, thus they were not knew the benefit of early breast feeding practice for the neonate and for mother.
Occupation of woman and husband
Majority (95%) of women who were home lady and their husband were farmers were not timely initiated breast feeding for their neonate but women who were employed and their husband were employed were timely initiated breast feeding for their neonate within first one hour after delivery.
Route of delivery
The result showed that majority 478 (79.90%) of women were gave birth via SVD in home and some in health institution, but some 100 (16.70%) of women were gave birth via AVD in health institution and a few 20 (3.30%) of women were gave birth via C/S in health institution (Table 1).
| Characteristics | Numbers | Percent | |
|---|---|---|---|
| Age of a woman | |||
| 21-25yr | 90 | 15.1 | |
| 26-30yr | 299 | 50 | |
| 31-35yr | 200 | 33.4 | |
| Greater than 35yr | 9 | 1.5 | |
| Woman educational status | |||
| Illiterate | 557 | 93.14 | |
| Read and write only | 20 | 3.34 | |
| Primary school | 10 | 1.67 | |
| Secondary school | 8 | 1.33 | |
| Diploma | 2 | 0.33 | |
| Degree | 1 | 0.16 | |
| Religion of a woman | |||
| Orthodox Christian | 300 | 50.2 | |
| Muslim | 23 | 3.8 | |
| Protestant Christian | 195 | 32.6 | |
| Catholic Christian | 70 | 11.7 | |
| Cultural/traditional | 10 | 1.7 | |
| Ethnicity of a woman | |||
| Dawuro | 578 | 96.65 | |
| Wolayita | 20 | 3.34 | |
| Amhara | 4 | 0.66 | |
| Marital status of a woman | |||
| Married | 560 | 93.6 | |
| Unmarried | 16 | 2.7 | |
| Divorced | 16 | 2.7 | |
| Widowed | 6 | 1 | |
| A woman currently live with | |||
| Alone | 32 | 5.4 | |
| Woman and father | 6 | 1 | |
| Husband | 560 | 93.6 | |
| Current occupation of a woman | |||
| Government employee | 30 | 5 | |
| Private employee | 28 | 4.7 | |
| Merchant | 100 | 16.7 | |
| Home lady | 400 | 66.9 | |
| Student | 40 | 6.7 | |
| Average monthly income of a woman | |||
| 50 | 200 | 33.4 | |
| 100 | 300 | 50.16 | |
| 200 | 90 | 15.05 | |
| >200 | 8 | 1.33 | |
| Husband’s educational status | |||
| Illiterate | 20 | 3.5 | |
| Read and write only | 140 | 25 | |
| Primary school | 263 | 46.9 | |
| Secondary school | 60 | 10.7 | |
| Diploma | 62 | 11.07 | |
| Degree | 15 | 2.68 | |
| Husbands’ occupation | |||
| Farmer | 376 | 67.14 | |
| Employed (Private) | 10 | 1.78 | |
| Employed (Govt.) | 11 | 1.96 | |
| Small Scale Merchants | 161 | 28.75 | |
| Husband not alive | 2 | 0.35 | |
| Parity of the woman | |||
| Primipara | 160 | 26.8 | |
| Multiparous | 438 | 73.2 | |
| ANC follow | |||
| Woman who have ANC follow up | 200 | 33.44 | |
| Woman who have no ANC follow up | 398 | 66.55 | |
| Frequency of ANC follow up | |||
| Once | 100 | 16.72 | |
| Twice | 100 | 16.72 | |
| Not follow ANC | 398 | 66.55 | |
| Type of ANC woman visited | |||
| Only 1st visit | 63 | 10.7 | |
| Only 2nd visit | 0 | 0 | |
| Only 3rd visit | 0 | 0 | |
| Only 4th visit | 37 | 6 | |
| Not visited | 198 | 33.1 | |
| 1st and 2nd | 200 | 34.3 | |
| 1st and 3rd | 40 | 6.7 | |
| 1st and 4th | 60 | 10 | |
| Medical problem during ANC follow up | |||
| No | 360 | 60.2 | |
| Ye | 238 | 6.7 | |
| Type of medical problems that a woman had during ANC follow up | |||
| HTN | 30 | 75 | |
| DM | 6 | 15 | |
| Anaemia and PEM | 2 | 5 | |
| Anaemia | 2 | 5 | |
| No medical problem | 360 | 60.2 | |
| Woman counselling about TIBF during ANC follow up | |||
| No | 379 | 63.4 | |
| Ye | 219 | 3.5 | |
| Place of delivery | |||
| Health center | 200 | 33.44 | |
| Hospital | 60 | 10 | |
| Home | 338 | 56.52 | |
| Assistant of Home delivery | |||
| TBA | 44 | 31.42 | |
| Neighbour | 96 | 68.57 | |
| Route of delivery | |||
| AVD | 400 | 79.9 | |
| C/S | 20 | 3.3 | |
| SVD | 100 | 16.7 | |
| Bleeding at delivery | |||
| Less than 500 ml | 200 | 33.4 | |
| Greater than 500 ml | 98 | 16.4 | |
| Not known | 300 | 50.2 | |
| Duration of bleeding after delivery | |||
| Up to one hour | 100 | 16.7 | |
| More than one hour | 98 | 16.4 | |
| For 24 hr | 400 | 66.9 | |
| Gender of neonate | |||
| Male | 200 | 33.4 | |
| Female | 398 | 66.6 | |
| Gender of neonate which woman wish at ANC visit | |||
| Male | 400 | 66.9 | |
| Female | 198 | 33.1 | |
| Type of gender take more care at neonatal period | |||
| Male | 400 | 66.9 | |
| Female | 198 | 33.1 | |
| Gestational age | |||
| Women who do not know their GA | 338 | 56.52 | |
| Women who know their GA | 260 | 43.47 | |
| Woman gave birth | |||
| At term | 380 | 63.54 | |
| At pre term | 64 | 10.72 | |
| At post date | 104 | 17.39 | |
| Birth weight | |||
| Less than 1.5 kg | 4 | 0.3 | |
| 1.5 kg-2.5 kg | 284 | 47.49 | |
| 2.5 kg-4 kg | 310 | 51.83 | |
| Woman agreement on TIBF | |||
| No | 358 | 59.86 | |
| Yes | 239 | 39.96 | |
| First breast milk has disadvantage for new born | |||
| No | 60 | 10.04 | |
| Yes | 538 | 89.96 | |
| What is disadvantage of first breast milk? | |||
| It causes abdominal cramping | 310 | 51.83 | |
| It is not easily digestible | 180 | 30.1 | |
| All | 108 | 18.06 | |
| What you give new born at first time | |||
| Breast milk | 262 | 43.8 | |
| Butter | 97 | 16.4 | |
| Cow milk | 237 | 39.8 | |
| Water | 1 | 0 | |
| Nothing per os in the 1st hour | 1 | 0 | |
Table 1: Characteristics of a women, babies, deliveries, and ANC follow up in Dawuro Zone, South West Ethiopia, January 2018 (N=598).
Timely initiation of breast-feeding among rural women The result showed that 238 (39.80%) of women were timely initiated breast feeding for their neonate and 360 (60.20%) of women were not timely initiated breast feeding for their neonate. Timely initiation of breastfeeding was associated with place of delivery, immediate post-natal advice on breast feeding to the mother, educational status of the women, ANC counselling on timely initiation of breast feeding, route of delivery, parity of a woman, and awareness of the mother on timely initiation of breast feeding.
This was supported by the FGD result with adult women. In this focus group the discussants were agreed that when a neonate was initiated breast feeding immediately after birth it cause crying of a neonate due to its difficulty to digestion and then the women went to traditional healer and gave traditional medicine to a neonate to facilitate the digestion of a cholesterol. “One woman in our village was gave local medication to her neonate to make easily digest first breast milk after giving first breast milk to her neonate then the neonate has abdominal distention and difficulty of breathing then final a neonate was died due to immediate initiation of breast feeding” (32 year, women).
Bivariate logistic regression of predictors of the study subject with dependent variables in Dawuro Zone, South West Ethiopia, 2018 (N=598).
Socio-demographic variables, route of delivery, medical problem during ANC follow up, giving cow milk to a neonate at birth, place of delivery, and counselling on timely initiation of BF during ANC follow up had association with timely initiation of breast feeding in bivariate logistic regression and three variables had significant association with timely initiation of breast feeding (Table 2).
| Variable | Timely initiation of breast feeding | OR of 95% CI | |
|---|---|---|---|
| No TIBF n (%) | TIBF n (%) | ||
| Attendance of school | |||
| Yes | 14 (34.14) | 27 (65.85) | 1.00 |
| No | 346 (62.11) | 211 (37.89) | 3.17 (1.62, 6.7) *** |
| Level of education | |||
| Above grade 8th | 3 (27.27) | 8 (72.72) | 1.00 |
| Grade 1st-8th | 6 (20.00) | 24 (80.00) | 1.06 (0.80, 1.60) |
| Illiterate | 351 (97.50) | 206 (57.22) | 3.92 (3.05, 5.03) *** |
| Route of delivery | |||
| AVD | 81 (82.50) | 19 (18.00) | 1.00 |
| C/S | 1 (0.00) | 19 (100.00) | 1.02 (0.70, 1.45) |
| SVD | 278 (58.15) | 200 (41.84) | 0.31 (0.22, 0.44) *** |
| Medical problem at ANC follow up | |||
| Yes | 300 (83.33) | 60 (16.66) | 1.00 |
| No | 60 (25.21) | 178 (74.60) | 3.50 (1.56,6.32) ** |
| Counselling on TIBF during ANC | |||
| Yes | 45 (20.54) | 174 (79.45) | 1.00 |
| No | 315 (83.11) | 64 (16.88) | 2.34 (1.44,5.78) * |
| Place of delivery | |||
| Health institution | 60 (12.60) | 200 (87.40) | 1.00 |
| Home | 300 (92.80) | 38 (7.20) | 2.34 (1.44,5.78) ** |
| Gender of a neonate which women wish at ANC visit | |||
| Male | 160 (44.44) | 200 (55.55) | 1.00 |
| Female | 200 (72.46) | 38 (15.96) | 1.20 (1.65,8.61) |
| Birth weight | |||
| 2.5 kg-4 kg | 50 (20.00) | 200 (80.00) | 1.00 |
| 1.5 kg-2.5 kg | 247 (86.97) | 37 (13.02) | 1.20 (0.23,2.00) |
| Less than 1.5 kg | 3 (75.00) | 1 (25.00) | 4.32 (3.23,7.53) |
| Women gestational age | |||
| Women know their GA | 60 (23.07.85) | 200 (76.92) | 1.00 |
| Women not know their GA | 250 (86.80) | 38 (13.20) | 2.56 (4.67,16.89) |
| Women gave birth at which gestational age | |||
| At term | 150 (39.47) | 230 (60.52) | 1.00 |
| At post date | 100 (96.15) | 4 (3.84) | 1.67 (5.87,11.68) |
| At pre term | 60 (93.75) | 4 (6.25) | 1.9 (6.78,7.89) |
| Age of a woman | |||
| Greater than 35yr | 10 (66.60) | 60 (33.40) | 1.00 |
| 31-35yr | 70 (30.1) | 120 (60.90) | 2.20 (1.34,8.21) |
| 26-30yr | 80 (5.00) | 50 (95.00) | 4.32 (3.23,7.53) |
| 21-25yr | 200 (33.40) | 8 (66.60) | 3.20 (1.23,19.10) |
| Women agreement on TIBF | |||
| Very agree on TIBF | 5 (3.49) | 139 (96.51) | 1.00 |
| Agree on TIBF | 25 (89.67) | 38 (10.32) | 1.43 (3.54,7.69) |
| Neutral on TIBF | 4 (40.00) | 6 (60.00) | 1.54 (5.78, 9.89) |
| Disagree on TIBF | 250 (83.33) | 50 (16.66) | 1.56 (4.21,9.67) |
| First breast milk has disadvantage for new born | |||
| Yes | 300 (88.75) | 38 (11.24) | 1.00 |
| No | 60 (23.07 | 200 (76.93) | 2.45 (4.65,8.32) |
| What is disadvantage of first breast milk for a new born? | |||
| It causes abdominal pain | 200 (64.51) | 110 (35.45) | 1.00 |
| It is not easily digestible | 100 (55.55) | 80 (44.44) | 3.20 (2.23,2.00) |
| All the above disadvantage | 60 (57.14) | 45 (42.85) | 4.32 (6.23,7.53) |
| What you give for a new born in the 1st one hour after birth? | |||
| Breast milk | 80 (28.38) | 222 (71.61) | 1.00 |
| Butter | 120 (94.48) | 7 (5.51) | 1.40 (2.34,18.21) |
| Cow milk | 158 (83.59) | 31 (16.40) | 2.32 (13.23,17.53) |
| Water | 1 (100.00) | 0 (0.00) | 4.20 (3.34,9.21) |
| Nothing per os in 1 stone hr. | 1 (100.00) | 0 (0.00) | 5.20 (11.23,29.10) |
p* means PV<0.01, p** means PV<0.05, p*** means PV<0.02 and p means PV>0.02
Table 2: Bivariate logistic regression of predictors of the study subject with dependent variables in Dawuro Zone, South west Ethiopia, January 2018 (N=598)
Independent predictors of timely initiation of breast feeding by rural women
The variables with PV<0.2 in bivariate logistic regression were entered in to multivariate logistic regression to get independent predictors of timely initiation of breast feeding and the following independent predictors had significant association with timely initiation of breast feeding such as counselling on timely initiation of breast-feeding during ANC follow up and place of delivery. The association in multivariate logistic regression revealed that rural women who had no counselling on timely initiation of breast feeding during ANC follow up were more likely not timely initiated breast feeding than those had counselling on timely initiation of breast feeding during ANC follow up [AOR 2.01, 95% CI (1.20, 3.37)] with PV<0.05, rural women who gave birth in home were more likely not timely initiation of breast feeding than those gave birth in health institution [AOR 2, 95% CI (1.35, 2.95)] with PV<0.01 (Table 3).
| Variable | TIBF | AOR of 95% CI | |
|---|---|---|---|
| Non users n (%) | User n (%) | ||
| Counselling on timely initiation of breast-feeding during ANC follow up | |||
| Yes | 45 (20.54) | 174 (79.46) | 1.00 |
| No | 315 (83.11) | 64 (16.89) | 2.01 (1.20, 3.37) ** |
| Place of delivery | |||
| Health institution | 60 (12.60) | 200 (87.40) | 1.00 |
| Home | 300 (92.80) | 38 (7.20) | 2.00 (1.35, 2.95) * |
Table 3: Multivariate logistic regression of maternal and institutional variables of study subject with TIFB in Dawuro Zone, South West Ethiopia Zone, June 20178 (N=844).
Discussion
This study was assessed a series of potential predictors including age, educational level of the woman, awareness on timely initiation of breast feeding, ANC follow up, socioeconomic of the family, birth weight of the neonates, gestational age of the women, counselling during ANC follow up, place of delivery, perception of the woman on breast feeding, gender of the neonates and route of delivery toward timely initiation of breast feeding after delivery by rural women.
The mean age of the rural women was 26.35 with SD of 1.98. From total non-timely initiator of breast feeding for their neonate the majority (85%) of non-timely initiator of breast feeding rural women had age range mean and below the mean but women with age range between 20yr-28yr was very vulnerable for less breast milk production so that early initiation of breast feeding and repeated gave of breast feeding for the neonate was important for increment of breast milk production in their mammary gland [9,10].
Three hundred seventy-nine (63.37%) of respondents were not counselled during their ANC follow up for timely initiation of breast feeding and not did timely initiated breast feeding for their neonate. Out of 379 women who were not initiated timely breast feeding 55.55% reasoned out that first breast milk was not easily digestible and 44.44% reasoned out that first breast milk cause abdominal cramping on neonate. This was in line with the study conducted in North Gondar on exclusive breast feeding [16].
The study revealed that rural women who were not counselled for timely initiation of breast feeding during ANC follow up were more likely not timely initiated breast feeding than those who were counselled on timely initiation of breast feeding during ANC follow up [AOR 2.01, 95% CI (1.20, 3.37)] with PV<0.05 [17,18].
It showed that from total respondent majority 577 (96.48%) respondents were not attended the school and from them three hundred thirty three (59.52%) of the respondents had no awareness on timely initiation of breast feeding and was not timely initiated breast feeding for their neonate, and 41 (6.85%) of the respondents was attended the school and had awareness for timely initiation of breast feeding of their neonate hence increasing educational status of rural woman was obligatory for increment of awareness on timely initiation of breast feeding by rural women to increase timely initiation of breast feeding [18,19].
This was supported by FGD result with adult men. In this FGD discussants were agreed that when the woman was not attended the school, she was not went to health institution to get health information from health professional and not follow media rather than she went traditional healer and TBA to get health information and medicine but she went to health institution only when she was severely ill.
The study showed that from total rural women three hundred eighty-eight (56.52%) of the respondents were gave birth in home and three hundred (88.56%) of them were not initiated timely breast feeding for their neonate. It showed that two hundred sixty (43.47%) of rural woman were gave birth in health institution from them two hundred (87.40%) of rural women were initiate timely breast feeding [18]. Rural women who gave birth in home were more likely not initiated timely breast feeding for their neonate than those who gave birth in health institution to initiated timely breast feeding [AOR 2.00, 95% CI (1.35,2.95)] with PV<0.05.
It indicated that three hundred (50.16%) of respondents were disagree on timely initiation of breast feeding for their neonate and from them two hundred fifty (83.33) rural women were not initiated timely breast feeding for their neonate. One hundred twenty-six (21.07%) of rural woman were gave butter for their neonate after birth and from them one hundred twenty (94.48) not initiated timely breast feeding for their neonate. Mostly cited reasons for giving butter for their neonate by the rural women were butter made the neonate stool soft to defecate, it made rapid closure of the fontanel in neonate, and it was prevented constipation but which was harm full traditional practice in rural set up of the Ethiopia. This was in line with study conducted in North West Ethiopia on inclusive breast-feeding practice [18].
In this study timely initiation of breast feeding by rural women was significantly associated with counselling on timely initiation of breast-feeding during ANC follow up and place of delivery with PV<0.05 and <0.01 respectively. In addition to this attending school, route of delivery, medical problem during ANC follow up and gestational age were positively associated with timely initiation of breast feeding by the rural women to their neonate.
This was supported by FGD result with adult women. In this FGD discussants were agreed that when the rural women were educated, pregnancy completed nine months, and no medical problem during pregnancy they gave new born care immediately after birth including breast feeding. This was in line with study conducted in Arsi Zone, South-East Ethiopia [19].
The study showed that rural women who were not counselled on timely initiation of breast feeding during ANC follow up were more likely not initiated timely breast feeding than those with counselled on timely initiation of breast feeding during ANC follow up [AOR 2.01, 95% CI (1.20, 3.37)] with PV<0.01. Rural women who gave birth in home were more likely not initiated timely breast-feeding practice to their neonate than those who utilize institutional delivery [AOR 2.00, 95% CI (1.35,2.95)] with PV<0.05. These were bit in line with study conducted in safe delivery service utilization in Sekela, North West Ethiopia [20].
Strength and limitation of the study
Strength of the study was that the response rate was hundred percent and it was used both qualitative and quantitative methods. Therefore, this stud was the prominent for other researchers. On other hand the limitation of the study was that since some questions included sensitive issues, responses were sorted and could create desirability bias or response bias. There were others social cognitive variables which were highly predictive of behaviours in other models were not incorporated and the results were interpreted for the catchment population which was some of the limitation of the study.
Conclusion
This study had found out that majority (60.20%) of rural women were not initiated timely breast feeding practice for the neonate in presence of health institution, health workers and local media for local language communication in both district to introduce awareness and benefit of timely initiation of breast feeding message in the community at large in rural set up. Timely initiation of breast feeding for a neonate within one hour after delivery was the best practice when done by the rural women to maintain neonatal health by giving the breast milk cholesterol which was equivalent to immunization.
Most (63.37%) of the rural women were not counselled for timely initiation of breast feeding during their ANC follow up to start breast feeding with in the first one hour after delivery despite there were midwife nurse in each health center and hospital during ANC and more than two health extension worker in each kebele in each district of Dawuro Zone to introduces breast feeding related morbidity and benefit of breast feeding message to increase precipitation of rural women on early initiation of breast feeding. Community’s leader and influential person were not agreed on timely initiation of breast feeding by rural women due to it cause cramping of abdomen because it was crude for digestion for a neonate opment armies in each kebele to create awareness about timely initiation of breast feeding on community leaders and influential person in the rural community at large and at household level.
It showed that rural women who were attended the schools had awareness on timely initiation of breast-feeding practice and had positive attitude toward giving first breast milk for a neonate to maintain health of a neonate rather than illiterate women. Therefore, increasing educational level of rural women was compulsory for increment of timely initiation of breast feeding for a neonate by making rural women to understand the first breast milk (cholesterol of breast milk) and its benefit. Because when the rural woman was educated, and she was aware about cholesterol then she would give cholesterol for her neonate, but when she was not attended the school, she was not aware about cholesterol and TIBF.
It clearly showed that promoting positive attitude toward cholesterol of breast milk, counseling on timely initiation of breastfeeding during ANC follow up, giving birth in health institution and attending school by rural women were extremely essential to increase timely initiation of breast feeding for their neonate by rural women then to decrease neonatal illness and death in the country.
This study showed that there was statistically significant association between place of delivery and counselling on timely initiation of breast-feeding during ANC follow up of rural women with timely initiation of breast feeding for a neonate with PV<0.05.
The role of shaman, religious leader, family, local media, health development army and IEC materials had significant positive influence on timely initiation of breast feeding by the rural women in addition to health extension worker, midwifery nurse, and health institution behaviour because the study revealed that majority of rural women believe shaman’s advice and religious leader to timely initiate breast feeding to their neonate.
The study confirmed that rural women who were followed IEC materials on promotion of breast-feeding practice in rural set up, attained ANC follow up and reached local media had positive attitude toward first breast milk (cholesterol) to timely initiate breast feeding to their neonate. Therefore, synchronized integration was required to increase timely initiation of breast-feeding practice in the community by the rural women for early breast-feeding practice meaning within one hour after delivery. Timely initiation of breast feeding was one of the most important health promotive behaviours of the women by increasing immunity of a neonate to maintain health because neonate was prone for neonatal disease.
In order to advance the rate of breast feeding with in the first hour of life, health professional must encourage the factors favouring timely initiation of breast feeding practice; such as ANC guidance regarding the advantage of breast feeding, health education during family planning period and caring up to full term birth, counselling on benefit of roué of delivery, and stimulate this practice in vulnerable situations such as woman with cesarean section and per term birth. In other hand the health development army must promote the importance of timely initiation of breast feeding for a neonate growth and development at each one to five networks in the community.
Recommendation
Information, education and communication programs on breast feeding practice should be strengthened and emphasis should be given to encourage the rural women to up take ANC services and counselling for timely initiation of breast-feeding during ANC follow up at all level of health institution in the Zone/district. Shaman, witchcraft, local communication media and family should be involved to increase perception of rural women to timely initiate of breast-feeding practice in addition to health worker. Ethnographic study should be done to assess the influence of native culture on timely initiation of breast feeding in rural women by other researchers.
Recommendation
Information, education and communication programs on breast feeding practice should be strengthened and emphasis should be given to encourage the rural women to up take ANC services and counselling for timely initiation of breast-feeding during ANC follow up at all level of health institution in the Zone/district. Shaman, witchcraft, local communication media and family should be involved to increase perception of rural women to timely initiate of breast-feeding practice in addition to health worker. Ethnographic study should be done to assess the influence of native culture on timely initiation of breast feeding in rural women by other researchers.
Ethical Consideration
Ethical approval and clearance were obtained from the Wolaita Sodo University Dawuro Tarcha campus Public Health department Ethical Clearance Committee. Letter of cooperation to Mareka and Gena-Bosa weredas were obtained from Dawuro Zone chief administrative office and Dawuro Zone health department office to respective wereda health office, and selected Keble administration. Signed informed consent was obtained from all participants who were advised that they could withdraw from the study without having to provide justification. Informed consent was obtained from spouse when spouse was conservative by informing the purpose of the study.
Dissemination Plan
The findings of this study was presented to WSU, DTC, regional health bureau, Dawuro zone health department annual meeting, Dawuro Zone administration counsel, Mareka Wereda administration counsel and other organizations who were working on under five nutrition services final it should be published in a scientific journal.
Acknowledgment
I would like to thank the WSU Dawuro Tarcha campus research coordinating office for providing material support. My thanks also go to Dawuro Zone health department, Mareka wereda health office particularly, Ato Aklilu Asefaw and Menegash Negash. Final I would like to thank midwifery nurse of Dashi health center and Duga health center.
REFERENCES
- Tewodros A, Jemal H, Dereje H. Determinants of exclusive breast-feeding practices in Ethiopia. Ethiop J Health Dev 2009;23:12-18.
- World Health Organization (WHO) Global Strategy for Infant and Young Child Feeding, Geneva, 2003.
- Edmond KM, Zandoh C, Quigley MA, Amenga ES, Owusu A. Delayed breast-feeding initiation increases risk of neonatal mortality. Pediatrics 2006; 117: e380-386.
- Federal Ministry of Health (FMOH) National strategy for Infant and Young Child Feeding (IYCF). Family Health Department, Ethiopia, 2004.
- United Nations Children’s Fund (UNICEF) Programming guide infant and young child feeding. Nutrition Section, Programmes, New York, 2004.
- Tesfaye S, Mulusew G, Tefera B. Determinants of timely initiation of breastfeeding among mothers in Goba Woreda, South East Ethiopia: A cross sectional study. BMC Public Health 2011; 11: 217.
- Teshome N. Factors affecting utilization of reproductive health services by adolescent females using the health belief model in Mareka district, Dawuro Zone Southern Ethiopia. J Cult Society,2016;21.
- Jones G, Steketee RW, Black RE, Bhutta ZA, Morris SS. How many child deaths can we prevent this year?Lancet 2016;362: 65-71.
- Darmstadt GL, Bhutta ZA, Cousens S, Adam T, Walker N. Evidence based, and cost-effective interventions: How many newborn babies can we save? Lancet 2005;365: 977-988.
- Teshome N. Outpatient satisfaction on health center services using qualitative study design in Mareka district, Dawuro Zone Southern Ethiopia. J Health Med Nurs 2016;29.
- Nakao Y, Moji K, Honda S, Oishi K. Initiation of breastfeeding within 120 minutes after birth is associated with breastfeeding at four months among Japanese women: A self-administered questionnaire survey. Int Breastfeed J 2008;3:1.
- Merewood A, Brooks D, Bauchner H, MacAuley L, Mehta SD. Maternal birthplace and breastfeeding initiation among term and preterm infants: A state-wide assessment for Massachusetts. Pediatrics 2006; 118:1048-1054.
- Walker M. Breastfeeding the late preterm infant. J Obstet Gynecol Neonatal Nurs 2008;37:692-701.
- Indu KS, Byrne. Early initiation of breastfeeding: A systematic literature review of factors and barriers in South Asia. Int Breastfeed J 2016; 11:1210-22.
- Edmond KM, Kirkwood BR, Amenga-Etego S, Owusu-Agyei S, Hurt LS. Effect of early infant feeding practices on infection-specific neonatal mortality: An investigation of the causal links with observational data from rural Ghana. Am J Clin Nutr 2007; 4: 1126-1131.
- Alemayehu T, Haidar J, Habte D. Determinants of exclusive breastfeeding practices in Ethiopia. Ethiop J Health Dev 2009;23:12-18.
- Vieira TO, Vieira GO, Giugliani ER, Mendes CM, Martins CC. Determinants of breast-feeding initiation within the first hour of life in Brazilian: Cross-sectional study. BMC Public Health 2010;10:760.
- Gurmesa T, Abebe G. Safe delivery service utilization in Metekel Zone, Northwest Ethiopia. Ethiop J Health Sci 2008; 17:213-222.
- Mulumebet A, Abebe G, Tefera B. Predictors of safe delivery service utilization in Arsi Zone South-East Ethiopia. Ethiop J Health Sci 2011; 21:95-106.
- Alemayehu ST, Fekadu MA, Solomon MW. Institutional delivery service utilization and associated factors among mothers who gave birth in the last 12 months in Sekela District, North West of Ethiopia. BMC pregnancy and child birth,2012;12:74.
Citation: Negash T. (2019) Predictors of Timely Initiation of Breast-Feeding among Rural Women using Case Study Design in Dawuro Zone, Southern Ethiopia in 2018. J Clin Med Sci;3:111. doi: 10.35248/2593-9947.19.3.111
Copyright: ©2019 Negash T. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
