Indexed In
- Open J Gate
- Genamics JournalSeek
- SafetyLit
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
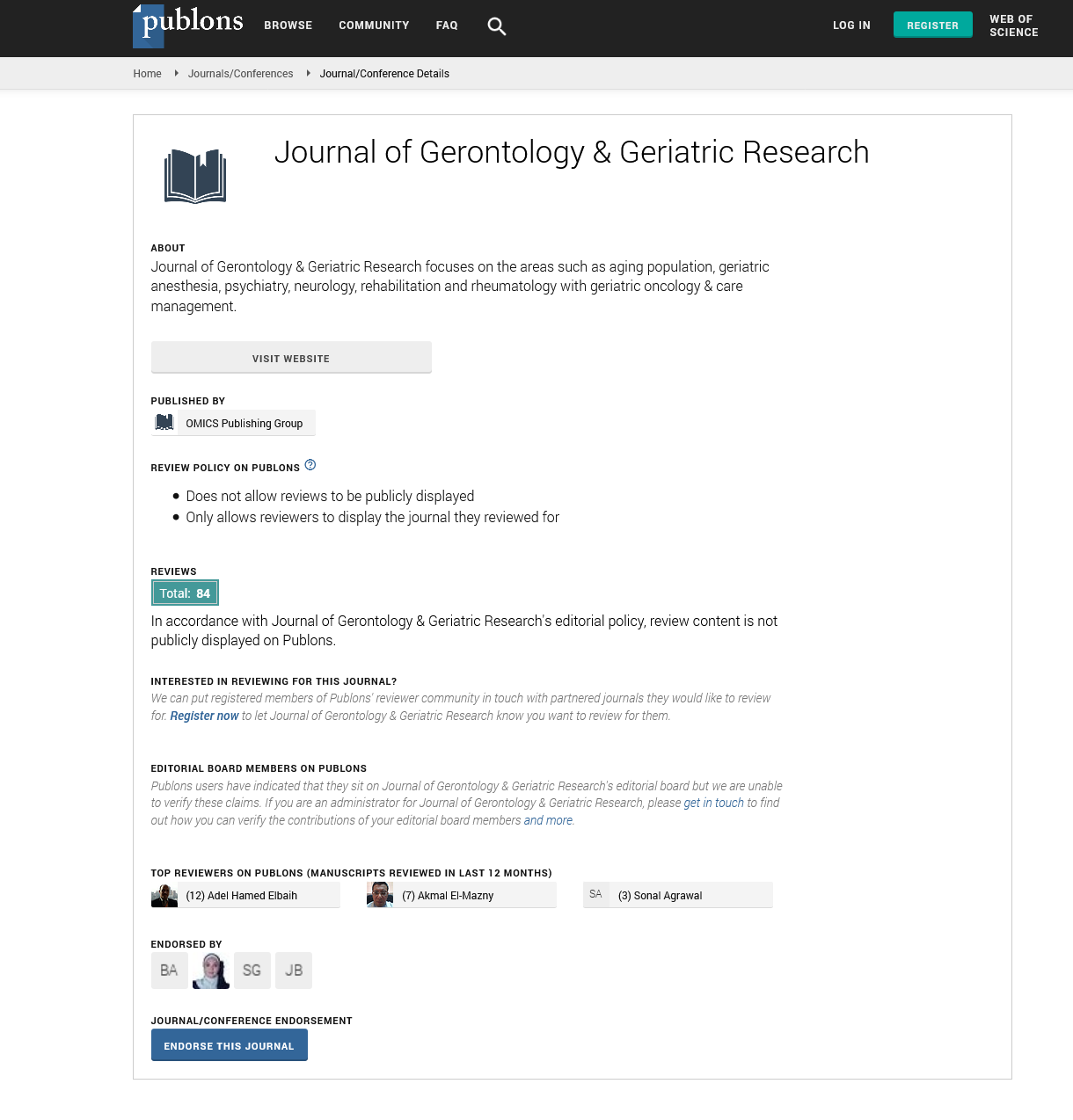
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Short Communication - (2022) Volume 11, Issue 5
Predictive of Functional Outcomes in Older Trauma Patients
William Eardley*Received: 05-May-2022, Manuscript No. jggr-22-17195; Editor assigned: 07-May-2022, Pre QC No. P-17195; Reviewed: 15-May-2022, QC No. Q-17195; Revised: 20-May-2022, Manuscript No. R-17195; Published: 25-May-2022, DOI: 10.35248/2167-7182.2022.11.614
Introduction
Patients who are older are more susceptible to bad outcomes following trauma than those who are younger. Sarcopenia, or bone mass loss, is common in trauma patients hospitalized to the Intensive Care Unit (ICU), and it has been linked to poor outcomes including mortality and ICU days. However, it is unclear whether it can predict other consequences. We anticipated that in elder trauma patients admitted to the ICU, sarcopenia predicts poor functional outcomes. We conducted a two-year retrospective review of patients aged 55 and older admitted to a surgical ICU in a Level I trauma hospital. On admission Computed Tomography (CT), total skeletal muscle cross-sectional area was measured at the L3 level and corrected for height using sex-specific cut-offs. Inhospital mortality, functional outcomes determined by the Glasgow Outcome Scale (GOS) at discharge, and discharge disposition were the primary outcome measures. To find determinants of primary outcomes, researchers employed multivariable logistic regression. In the United States, older people are the fastest-growing demographic group treated in trauma centres. It is widely known that they are more susceptible to negative consequences, with the highest case fatality rates reported in individuals aged 75 and up. Despite having same injury severity, they have a higher chance of fatality than their younger counterparts. However, the increase in morbidity and death is not only due to age. Comorbidities, preinjury functional level, and nutritional condition have all been linked to their increased susceptibility to poor outcomes. Frailty has been postulated as a better predictor of worse outcomes in elder trauma patients than age alone [1,2].
Using frailty for risk stratification in a trauma patient group, on the other hand, is quite difficult; many of the frailty indices are sophisticated and difficult to apply quickly at the bedside of an injured patient. Sarcopenia has been proposed as a proxy marker for frailty and has been demonstrated to be an independent predictor of poor in-hospital complications in elder trauma patients as an alternative. Sarcopenia is defined as a decrease of skeletal muscle mass that is accompanied by functional, metabolic, and immunologic implications as a result of ageing. The skeletal muscle, in addition to its crucial role in mobility, maintains protein synthesis rates in other vital tissues during times of stress since it is the body's greatest protein reserve. It's also in charge of immune processes like antibody formation, wound healing, and the creation of white blood cells during an infection. Sarcopenia as a marker of frailty has the benefit of being able to be assessed quickly and objectively using axial Computed Tomography (CT) imaging, which is frequently performed on trauma patient. In older trauma patients, sarcopenia are exceedingly frequent and undervalued [3].
This is a two-year retrospective research of trauma patients aged 55 and over admitted to a surgical ICU at an urban Level I trauma hospital, with a convenience sample of all patients (2012 and 2014). Based on findings in the trauma literature demonstrating that the death rate increases after the age of 55, the age of 55 years or older was adopted as the inclusion criteria. We only included patients admitted to the surgical ICU in order to evaluate the effect of sarcopenia in moderately to seriously injured patients, as its influence is unlikely to be seen in mildly damaged patients referred to ordinary wards. If a CT scan of the abdomen was not performed at the time of admission, the patient was ruled out. Patient demographics, injury mechanisms, Injury Severity Score (ISS), Glasgow Coma Scale (GCS) at presentation, and comorbidities were all gathered. End-stage renal disease requiring hemodialysis, end-stage liver disease, advanced dementia, Chronic Obstructive Pulmonary Disease (COPD) requiring home oxygen, metastatic cancer, history of stroke, or immunosuppressant usage were among the life-limiting conditions collected. In-hospital mortality, functional status at discharge as judged by the Glasgow Outcome Scale (GOS), and discharge disposition were the key outcome outcomes [4,5].
Conclusion
We also included discharge disposition as one of our primary objectives, which, together with functional outcomes, could be a more meaningful outcome for older patients who value quality of life over lifespan. Despite the fact that our 2 test did not give statistically significant results due to a limited number of patients discharged to dependent care, sarcopenic patients were discharged to dependent care twice as often (11%) as non-sarcopenic patients (5 percent). This was comparable to the findings of a study that looked at discharge disposition in older patients who had suffered a blunt traumatic injury. While adjusting for age and other major covariates, Fairchild found that every 1 cm2 increase in the psoas muscle cross-sectional area was associated with a 20% rise in body weight.
Conflict of Interest
None.
REFERENCES
- Airagnes G. Childhood adversity and depressive symptoms following retirement in the Gazel cohort. J Psychiatric Res. 2016;82:80-90.
- Bandeen-Roche K. Frailty in older adults: A nationally representative profile in the United States. J Geront Series A. 2015;70:1427-1434.
- Baryshnikov I. Relationships between self-reported childhood traumatic experiences, attachment style, neuroticism and features of borderline personality disorders in patients with mood disorders. J Affective Disorders. 2017;210:82-89.
- Brown DW. Adverse childhood experiences and the risk of premature mortality. Amer J Preven Med. 2009;37:389-396.
- Chen C. The prevalence of subjective frailty and factors associated with frailty in Taiwan. Arch Gerontol Geriatr. 2010;50:S43-S47.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Citation: Eardley W (2022) Predictive of Functional Outcomes in Older Trauma Patients. J Gerontol Geriatr Res. 11: 614.
Copyright: © 2022 Eardley W. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.