Indexed In
- Genamics JournalSeek
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2021) Volume 0, Issue 0
Postnatal Care Service Utilization and Associated Factors among Women in Goba Woreda, Bale Zone, Ethiopia
Yonas Lamore*Received: 04-Nov-2021 Published: 25-Nov-2021
Abstract
Background: Postnatal care of mothers is essential to reduce maternal morbidity and mortality. Providing postnatal care to recently delivered mothers is quite essential. The aim of the study was to determine the postnatal care utilization and associated factors among women who gave birth in the last 12 months in Goba woreda, Bale Zone, Ethiopia, 2017.
Methodology: A community based cross-sectional study was conducted from March to April, 2017. Lottery method was employed to select the study participants. Binary and multivariable logistic regressions analysis was computed to evaluate the factors associated with postnatal care services utilization.
Result: In this study a total of four hundred twenty-two women were interviewed with a response rate of 100%. Of the total respondents, 178 (42.2%) utilized postnatal care service after delivery within six weeks of their last birth. Educational level of mothers, AOR=1.96, 95% CI=1.06-3.62, maternal knowledge on postpartum danger sign and symptoms, AOR=1.78, 95% CI=1.16-2.72, pregnancy desire AOR=1.89, 95%CI=1.67-3.35, ANC visit AOR=2.80, 95% CI=1.32-5.97 and place of deliver AOR=2.09, 95% CI=1.30-3.34 had showed statistical significant association with postnatal care utilization.
Conclusion: More than half of respondents in Goba woreda were not utilized postnatal care service. Maternal educational status, maternal knowledge on postnatal danger signs and symptom, pregnancy desire for youngest child, ANC attendance and place of delivery found to be independent predictors for PNC service utilization. Therefore, Zonal district and Oromia Health bureau should Improve PNC service utilization by community awareness with focus on maternal danger signs and symptoms during postpartum period, antenatal care and institutional delivery via appointment and counseling about danger sign and symptoms during postpartum period.
Keywords
Postnatal care utilization; Place of delivery; Maternal nutrition; Breastfeeding
Introduction
Postnatal period is the time from delivery of baby till the first 42 days. Risks of maternal and newborn deaths are greatest during the first 24 to 48 hours after birth. Therefore, Providing Postnatal Care (PNC) to recently delivered mothers is quite essential during this period. Globally every year, 40 million women give birth at home without the help of a skilled birth attendant. An estimated of 800 women die during pregnancy or childbirth and around 8,000 newborn babies die during their first month of life per day. Nearly all newborn and maternal deaths 99% occur in developing countries, where pregnant women and newborn babies lack access to basic health care services before, during and after delivery (Save the children, 2013).
In Ethiopia the estimate of maternal mortality ratio for the 7-year period preceding the 2016 EDHS is 412 deaths per 100,000 live births; that is, for every 1,000 births there are about 4 maternal deaths (EDHS, 2016). Studies have shown that postnatal care services utilization is affected by several factors including maternal age, educational level of the women, occupational status of women and husbands, place of delivery, mode of delivery, number of pregnancies, awareness about obstetric related danger sign, and awareness about PNC services. Only 17 percent of women received postnatal care within two days [1,2].
A study conducted on Postnatal Care Service Utilization and Associated Factors among Mothers in Lemo Woreda, Ethiopia showed that many opportunities are missed with low PNC coverage including exclusive breastfeeding, PMTCT, providing of family planning and maternal and new born care. Despite there is no research conducted regarding postnatal care service utilization in the study area. This study was help to identifying factors that affecting postnatal care service utilization. The finding of this study was also help as an input for program managers and other stakeholder who work on maternal and child health to strengthen PNC service utilization and it also used as a base line for other researchers for further study [3].
Materials and Methods
Study design, area and period
A community based quantitative cross-sectional study was conducted in Goba woreda from March to April, 2017 among reproductive age group mothers who gave birth the in last 12 months prior this data collection. The study was conducted in five rural kebeles (the smallest government administrative structure). Goba town is found in Bale zone, Oromiya regional state, Ethiopia. It is one of the 18 woreda in Bale zone. The woreda is located 444 km from Addis Ababa and 13 km from Zonal town; Bale Robe. According to the last census survey (2007) projection to 2017, the estimated population of Goba woreda is 53,121, of whom 26,030 males and 27,091 females.
Sample size determination and sampling technique
For objective one, single population proportion formula and for objective two, by using Epi-info version 7.4.1 StatCalc software was used to calculate the sample size for factors which have significant association in previous studies affecting postnatal care service utilization. The study was conducted out of 15 rural kebeles in five kebeles of Goba Rural woreda. Lottery method was employed to select the study participants. All women who have given birth in the last 12 months prior to the data collection period in Goba rural kebeles were included in the study [4].
Data collection instrument and procedures
The questionnaire was adapted by reviewing literatures of similar studies aiming on postnatal care service utilization and its associated factors. The questioners have three parts, which are socio demographic characteristics, obstetric health related factor, and mother’s awareness on postnatal care service utilization.
Five diploma and two BSc nurses were selected for data collector and supervisor respectively. The training was given for data collectors and supervisor for two days. The training session included the general objective of the study, content of the questionnaire, ways how to keep confidentiality and privacy and mechanisms how to resolve when a problem arises [5,6].
Data quality management
The questionnaire was prepared first in English then translated to Afan Oromo, which is the local language, and to check its consistency, it was back translated to English by an expert of both languages. The questioner was pretested 5% from total sample size on women who had given birth in the past six weeks to oneyear prior the data collection period on Wajitu-Shabe kebele. The data collected for pre-test did not included in the actual data of the thesis. In order to maintain quality of the data, the training was given for both data collectors and supervisors for two days by investigator in data collection procedures.
Data processing and analysis
First the data was checked for its completeness. Then, by entered in to Epi info 7 versions, the data was clean and corrected for errors and exported to Statistical Package for Social Science (SPSS) version 20. Descriptive statistics was used to determine the proportion of postnatal care service utilization. Binary and multiple logistic regressions were computed to assess the factors associated with postnatal care services utilization. Logistic regression analysis was carried out to see the independent effect of each variable on the outcome. Odds ratio and 95% CI was used to measure the statistical association. P-value 0.05 was used to determine the statistical significance of the tests. Finally, the result was presented in texts, tables and graphs.
Operational definition
Postnatal care utilization: Women had at least one checkup during the first 6 weeks by the health professional after home delivery and, for those mothers who gave birth at the health institution came back for postnatal care services after they were discharged to their homes [7-9].
Postnatal care: Refers to the assistance or care given to mother and baby by health workers during the postnatal follow up period such as counsel on baby care, support breastfeeding, maternal nutrition, provide contraception service, and immunize the infant [5].
Postpartum period: Starts after expulsion of placenta up to 42 days (6 weeks).
Ethical consideration
Formal letter was obtained from Madda Walabu University, Goba Referral Hospital, and School of Health Science. Supportive letters were obtained from Bale Zone Health Department and Goba woreda Administrative office. Participants were informed about the objective of the study and consent was obtained from the mothers. All the information given by the respondents was used for research purposes only and confidentiality was maintained by omitting any personal identifiers of the respondents. Participation was on voluntary basis and they could withdraw from the study at any time of data collection [10-13].
Results
Characteristics of the respondents
A total of 422 women who gave birth in the last two years prior to this survey were interviewed with a response rate of 100%. The mean age of the respondents was 29.55 (SD ± 6.34) years (Table 1).
| Variable | Frequency (No) | Percent (%) |
|---|---|---|
| Age | ||
| 15-24 | 108 | 25.6 |
| 25-34 | 199 | 47.2 |
| 35+ | 115 | 27.2 |
| Mean ( ± SD) | 29.55 (SD ± 6.34) | - |
| Religion | ||
| Muslim | 351 | 83.2 |
| Orthodox | 71 | 16.8 |
| Ethnicity | ||
| Oromo | 418 | 99.1 |
| Amhara | 4 | 0.9 |
| Marital status | ||
| Others* | 19 | 4.5 |
| Married | 403 | 95.5 |
| Occupation | ||
| House wife (unemployed) | 410 | 97.2 |
| Employed | 12 | 2.8 |
| Educational status of mother (N=422) | ||
| No formal education | 105 | 24.9 |
| Primary education | 179 | 42.4 |
| Secondary and above education | 138 | 32.7 |
| Educational status of husband (N=403) | ||
| No formal education | 85 | 21.1 |
| Primary education | 176 | 43.7 |
| Secondary and above education | 142 | 35.2 |
| Monthly income | ||
| <500 Eth Birr | 94 | 22.3 |
| 501-1500 Eth Birr | 258 | 61.1 |
| 1501-2500 Eth Birr | 53 | 12.6 |
| 2500+ Eth Birr | 17 | 4 |
Note: *indicate single, divorce and widowed
Table 1: Socio-demographics characteristic of respondent’s in Goba Woreda, Bale Zone, Southeast Ethiopia, 2017.
Postnatal care and obstetric health related factors
From total respondent’s, majority 335 (84.1%) of the pregnancy desire for youngest child were intended. All most all 384 (91%) respondents had a history of ANC follow up out of these, 42 (10.9%) were visited one times and 95 (24.7%) were visited four and above times. From those ANC visited 316 (82.3%) were Iron supplemented. From all participants, only 6 (1.4%) faced danger sign of pregnancy during last child birth. Concerning place of last delivery, 308 (73%) gave birth in health institution with the help of skilled provider. From those who delivered in health institution, majority 226 (73.4%) were delivered at Health Center, 69 (22.4%) were delivered at Hospital and 13 (4.2%) were delivered at Health post. Out of 308 mothers who delivered at Health institution, 222 (72.1%) were given appointment for postnatal care by the health care professionals before discharge. The remaining 86 (27.9%) participants were not informed to have postnatal care by the health professionals before discharge. Regarding child sex from single birth out of 415 respondents’, 248 (59.8%) were male and the remaining 167 (40.2%) female [14,15]. Concerning number of children, majority, 193 (45.7%) of respondents had 3 to 4 children and only 80 (19%) had 5 and above children. Regarding PNC service utilization decision making power, 342 (81%) of respondents stated that they made decision together with their husbands (Table 2). The data revealed that only 27 (15%) utilized PNC with in the first 48 hours after child birth and 130 (73%) of respondents received postnatal care service within 7 to 42 days of child birth (Figure 1).
| Variables | Frequency (No) | Percent (%) |
|---|---|---|
| Pregnancy desire for youngest child | ||
| Intended | 335 | 84.1 |
| Unintended | 67 | 15.9 |
| ANC visit in the past pregnancy | ||
| Yes | 384 | 91 |
| No | 38 | 9 |
| Times of ANC visit (N=384) | ||
| Once | 42 | 10.9 |
| Twice | 100 | 26 |
| Three times | 147 | 38.3 |
| Four times and above | 95 | 24.7 |
| Iron supplementation during ANC (N=384) | ||
| Yes | 316 | 82.3 |
| No | 68 | 17.7 |
| Danger sign during Pregnancy | ||
| Yes | 6 | 1.4 |
| No | 416 | 98.6 |
| Place of Last delivery | ||
| Health Institution | 308 | 73 |
| Home | 114 | 27 |
| Number of current children | ||
| 01-Feb | 149 | 35.3 |
| 03-Apr | 193 | 45.7 |
| 5+ | 80 | 19 |
| Did you have postnatal care | ||
| Yes | 178 | 42.2 |
| No | 244 | 57.8 |
| Number of postnatal care visit (N=178) | ||
| One times | 143 | 80.3 |
| Two times | 30 | 16.9 |
| Three times | 5 | 2.8 |
| Decision making power in PNC service utilization | ||
| Wife | 80 | 19 |
| Both wife and husband | 342 | 81 |
Table 2: Obstetrics’ health related factors among the respondent’s in Goba Woreda, Bale Zone, Southeast Ethiopia, 2017.
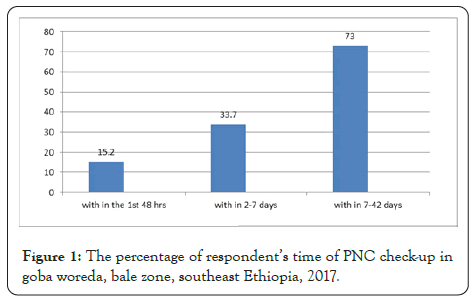
Figure 1: The percentage of respondent’s time of PNC check-up in goba woreda, bale zone, southeast Ethiopia, 2017.
Predictors of postnatal care utilization
In multivariable logistic regression model, after we entered the above 10 candidate variables the following five variables; educational status of mothers, whether or not know maternal dander sign and symptoms, pregnancy desire for youngest child, ANC visit and place of delivery had showed statistical significant association with PNC utilization. The odds of having postnatal care visit for those women who attended to Secondary and above education were nearly two times more likely to have PNC visit than those no formal education (AOR=1.96, 95% CI=1.06-3.62). In addition, knowledge of respondents on maternal danger sign and symptom of postpartum has also another predictor of PNC service utilization. Those mothers who know at least one maternal danger sign and symptom nearly two times more likely to be utilized postnatal care service than those who did not about maternal danger sign and symptom (AOR=1.78, 95% CI=1.16- 2.72). Those mothers who had planned pregnancy desire for youngest child were nearly two times more likely utilized postnatal care service than those unplanned (AOR=1.89, 95% CI=1.67- 3.35). ANC visit was also statically significant with postnatal care service utilization [16-19]. Those mothers who had attended ANC were nearly three times more likely utilize postnatal care service than non-attended (AOR=2.80, 95% CI=1.32-5.97).Women who delivered at health institution were two times more likely utilized postnatal care than those mothers who gave their last birth at home (AOR=2.09, 95% CI=1.30-3.34) (Table 3).
| Variable | PNC utilization | COR (95% CI) | AOR (95% CI) | |
|---|---|---|---|---|
| Yes (%) | No (%) | |||
| Educational status of mother | ||||
| No formal education | 55 (54.4) | 50 (47.6) | 1 | 1 |
| Primary education | 72 (40.2) | 107 (59.8) | 1.82 (1.11-2.96)* | 1.73 (0.10-3.00) |
| Secondary and above education | 51 (37) | 87 (63) | 1.95 (1.17-3.27)* | 1.96 (1.06-3.62)* |
| Educational status of husband | ||||
| No formal education | 44 (51.8) | 41 (48.2) | 1 | 1 |
| Primary education | 67 (38.1) | 109 (61.9) | 1.75 (1.04-2.95)* | 1.3 (0.72-2.35) |
| Secondary and above education | 61 (43) | 81 (57) | 1.43 (0.83-2.45) | 1.04 (0.55-1.94) |
| Occupation | ||||
| House wife (un employed) | 171 (41.7) | 239 (58.3) | 1.96 (0.61-6.27) | 2.68 (0.74-9.67) |
| Employed | 7 (58.3) | 5 (41.7) | 1 | 1 |
| Heard of postnatal care services utilization | ||||
| Yes | 146 (43.7) | 188 (56.3) | 0.74 (0.45-1.20) | 0.66 (0.39-1.13) |
| No | 32 (36.4) | 56 (63.6) | 1 | 1 |
| Knowledge about maternal danger sign and symptoms | ||||
| Yes | 89 (36.8) | 153 (63.2) | 1.68 (1.14-2.49)** | 1.78 (1.16-2.72)** |
| No | 89 (49.4) | 91 (50.6) | 1 | 1 |
| pregnancy desire for youngest child | ||||
| Intended | 139 (39.2) | 216 (60.8) | 2.16 (1.27-3.68)** | 1.89 (1.67-3.35)* |
| Unintended | 39 (58.2) | 28 (41.8) | 1 | 1 |
| ANC visit in the past pregnancy | ||||
| Yes | 156 (40.6) | 228 (59.4) | 2.01 (1.02-3.95)* | 2.80 (1.32-5.97)** |
| No | 22 (57.9) | 16 (42.1) | 1 | 1 |
| Place of Last delivery | ||||
| Health Institution | 118 (38.3) | 190 (61.7) | 1.79 (1.16-2.76)** | 2.09 (1.30-3.34)** |
| Home | 60 (52.6) | 54 (47.4) | 1 | 1 |
| Decision making power | ||||
| Wife | 28 (35) | 52 (65) | 1.45 (0.87-2.41) | 1.39 (0.80-2.44) |
| Both wife and husband | 150 (43.9) | 192 (56.1) | 1 | 1 |
Note: Reference category; ***p≤0.001; **p<0.01; *p<0.05
Table 3: Multivariable analysis of factors associated with postnatal care utilization Among Women who gave birth in the last 12 Months in Goba woreda, Bale Zone, Ethiopia, 2017.
Discussion
Evidence from the present study indicated that postnatal care service utilization was 42.2%. This result is higher than with the studies done in Debre Markos town, North western Ethiopia 33.5%, Jabitena District, Amhara 20.20%, Asella Town 35%, Nepal 25.1%, Nigeria 16.9%. This difference could be due to the improvement in accessibility of health facilities and the time difference between these studies. This finding was lower when comparable with the finding of study done in Lemo Woreda, Ethiopia 51.4%, Hossaian, South Ethiopia 51.4% and Addis Ababa 65.5%. This discrepancy could be due to less awareness and educated of the mothers on the importance of postnatal care service utilization it might be also due to methodology difference and social context variation between the present study and previous studies. In this study, it has been identified that five variables which is significantly associated with PNC service utilization. These included maternal educational status, knowledge of maternal danger signs and symptom, desire of pregnancy plan for youngest child, ANC and place of delivery.
Regarding educational status, mothers who had attended secondary and above educational level were more likely utilize PNC service than those who had no formal education. This finding is almost similar with previous studies, Central Statistical Agency, 2011. This could be explained by the fact that education has a valuable input in enhancing female autonomy and helps women develop greater confidence and capability to make decisions about their own health [18]. Thus, educated women try to find higher quality of health services and have greater ability to use health care inputs that offer better health outcomes. Knowledge on danger signs and symptoms of the mothers has also another positive association with PNC service utilization. Mothers who had knowledge for at least one possible postnatal danger sign and symptoms were more likely to utilize PNC service as compared to those who did not mention any postpartum danger signs and symptoms. This finding is supported by local studies conducted in Lemo Woreda, Hadiya Zone and Jabitena district, Amhara region [16]. The possible justification for these positive associations could be knowledge on obstetric danger signs and symptom during puerperium is an important factor in motivating mothers and their families to attend health care service at the earliest opportunity with the intention of prevention, early detection and getting managed their obstetric danger sign. In this study ANC attendance before giving last birth was also positively associated with PNC service utilization. Mothers who have attended at least one ANC visit before giving their last birth were more likely to utilize PNC service than those mothers who have not attended ANC visit at all. This result is consistent with the studies conducted in Lemo Woreda, Hadiya Zone (Belachew et al., 2016), studies done in Rural Ethiopia, Gondar Zuria District, Ethiopia Northwest Ethiopia Abuna Gindeberet District, West Shewa, Oromiya Region and Kenya. However, this result has disparity with the study conducted in Hossaina, Ethiopia and in Maiduguri, north-eastern Nigeria which showed that ANC follow up before giving last birth has no significant association with PNC service utilization. The possible reasons for the positive association between ANC attendance and PNC service utilization might be that mothers and their families receive health education and counseling during ANC visits and thus get good access to learn about the benefits of PNC services follow up in health care facilities.
According to this study the utilization of postnatal care was found significantly higher among women who had intended pregnancy as compared to those women whose pregnancy was unintended. Mothers who intended pregnancy desire more likely utilized postnatal care service than those mothers who didn’t intended. This finding is supported by local studies conducted in India (Chandra and Kumar, 2017). The possible justification might be women who were joyful with their pregnancy increase the possibility of seek postnatal care-taking services. This result is not in line with the study conducted in Ethiopia.
Place of delivery was statistically significantly associated with PNC service utilization. Mothers who gave birth in health institutions were more likely to utilize PNC service than those mothers who were gave birth at home. This finding is also consistent with the study conducted in Lemo woreda, Hadiya zone, south Ethiopia, Debremarkos town, North western Ethiopia, Jabitena district Amhara region, Ethiopia and Nepal. The possible explanation for this strong positive association of PNC services utilization with place of delivery could be that women who gave birth in health institution have greater opportunity for health education related to PNC services at the time of delivery and thus get access to learning about the types, benefits, and availabilities of PNC services during their stay in the health institutions.
Conclusion
Generally, this study found that more than half of respondents in Goba woreda were not utilized postnatal care service. Even though the first 48 hours a large proportion of maternal and neonatal death occurring and critical time for monitoring complication arising from delivery, this study found that postnatal care service utilization with in this period very low. The reason most of mothers were attended postnatal care service for recent delivery stated that for immunization and family planning and the major reasons for not attended postnatal care service were stated that because of being healthy of both mother and child, didn’t think it was necessary and being busy. Maternal educational status, maternal knowledge on postnatal danger sign and symptom, pregnancy plan, ANC attendance and place of delivery were found to be independent predictors for PNC service utilization.
REFERENCES
- Ambel AA, Andrews C, Bakilana AM, Foster E, Khan Q, Wang H. Maternal and child health inequalities in Ethiopia. World Bank Policy Research Working Paper. 2015:7508.
- Belachew T, Taye A, Belachew T. Postnatal care service utilization and associated factors among mothers in Lemo Woreda, Ethiopia. J Women’s Health Care. 2016;5(3):1-7.
- Belemsaga DY, Kouanda S, Goujon A, Kiendrebeogo JA, Duysburgh E, Degomme O, et al. A review of factors associated with the utilization of healthcare services and strategies for improving postpartum care in Africa. Afrika Focus. 2015;28(2):83-105.
- Berhanu S, Asefa Y, Giru BW. Prevalence of postnatal care utilization and associated factors among women who gave birth and attending immunization clinic in selected government health centers in Addis Ababa, Ethiopia, 2016. J Health Med Nursing. 2016;26(1):1-15.
- Darega B, Dida N, Tafese F, Ololo S. Institutional delivery and postnatal care services utilizations in abuna gindeberet district, west shewa, oromiya region, central Ethiopia: A community based cross sectional study. BMC Pregnancy Childbirth. 2016;16(1):149.
- Dutamo Z, Assefa N, Egata G. Maternal health care use among married women in Hossaina, Ethiopia. BMC Health Serv Res. 2015;15(1):365.
- Global Health Data Exchange. Ethiopia Mini Demographic and Health Survey 2014.
- Worku AG, Yalew AW, Afework MF. Factors affecting utilization of skilled maternal care in Northwest Ethiopia: A multilevel analysis. BMC Int Health Hum Rights. 2013;13(1):20.
- Worku AG, Yalew AW, Afework MF. Factors affecting utilization of skilled maternal care in Northwest Ethiopia: A multilevel analysis. BMC Int Health Hum Rights. 2013;13(1):20.
- Khanal V, Adhikari M, Karkee R, Gavidia T. Factors associated with the utilisation of postnatal care services among the mothers of Nepal: Analysis of Nepal demographic and health survey 2011. BMC Women's Health. 2014;14(1):1-3.
- Langlois ÉV, Miszkurka M, Zunzunegui MV, Ghaffar A, Ziegler D, Karp I. Inequities in postnatal care in low-and middle-income countries: A systematic review and meta-analysis. Bull World Health Organ. 2015;93(4):259-270.
- Limenih MA, Endale ZM, Dachew BA. Postnatal care service utilization and associated factors among women who gave birth in the last 12 months prior to the study in Debre Markos town, northwestern Ethiopia: A community-based cross-sectional study. Int J Reprod Med. 2016: 7095352.
- Muiruri NW. Factors affecting utilization of postnatal care services at central provincial general hospital, Nyeri Kenya. 2011:1-71.
- Nzioki JM, Onyango RO, Ombaka JH. Socio-demographic factors influencing maternal and child health service utilization in mwingi: A rural semi-arid district in Kenya. Am J Public Health Res. 2015;3(1):21-30.
- Somefun OD, Ibisomi L. Determinants of postnatal care non-utilization among women in Nigeria. BMC Res Notes. 2016;9(1):21.
- Paudel M, Khanal V, Acharya B, Adhikari M. Determinants of postnatal service utilization in a western district of Nepal: Community based cross sectional study. J Women’s Health Care. 2013;2(3):126.
- Tesfahun F, Worku W, Mazengiya F, Kifle M. Knowledge, perception and utilization of postnatal care of mothers in Gondar Zuria District, Ethiopia: A cross-sectional study. Matern Child Health J. 2014;18(10):2341-2351.
- Tesfaye S, Barry D, Gobezayehu AG, Frew AH, Stover KE, Tessema H, et al. Improving coverage of postnatal care in rural Ethiopia using a community‐based, collaborative quality improvement approach. J Midwifery Womens Health. 2014;59(S1):S55-S64.
- Takai IU, Dlakwa HD, Bukar M, Audu BM, Kwayabura AS. Factors responsible for under-utilization of postnatal care services in Maiduguri, north-eastern Nigeria. Sahel Medical J. 2015;18(3):109-115.
Citation: Lamore Y (2021) Postnatal Care Service Utilization and Associated Factors among Women in Goba Woreda, Bale Zone, Ethiopia. Clinics Mother Child Health. S11:005.
Copyright: © 2021 Lamore Y. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

